Ulcerative Colitis Symptoms And Causes
Ulcerative colitis is thought to develop when a person at genetic risk is exposed to certain environmental stressors.
These environmental stressors either change the ratio of gut bacteria or alter the way the immune system responds to bacteria .
As a result, the immune system attacks the intestinal lining causing inflammation and other symptoms, including:
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
Foods To Avoid With Ulcerative Colitis
Although there are foods that are common triggers during both Ulcerative Colitis flares and remission, the list expands when youre experiencing active Ulcerative Colitis symptoms. Keep in mind that Ulcerative Colitis triggers differ from person to person, so the real key to long-term Ulcerative Colitis management is identifying what works for you. Easier said than done, right?
If youve ever searched on your own to figure out how to manage your Ulcerative Colitis, youve probably found a ton of information. The challenge is that the information on the internet can be contradicting and confusing. If youre struggling with Ulcerative Colitis, we recommend enlisting the help of a registered dietitian. They will be able to help you better understand your UC and determine what foods and behaviors most trigger your symptoms.
Remember to limit fiber when you are experiencing an Ulcerative Colitis flare. High fiber foods are part of a healthy, well-rounded diet. However, when UC symptoms are active, you may need to temporarily limit fiber intake to reduce inflammation and allow your gut to heal. High fiber foods are harder to digest and can trigger UC symptoms. High fiber foods include whole grains, fruits with skin and seeds, vegetables with skin and seeds, raw vegetables, cruciferous vegetables, nuts, seeds, beans and legumes.
Read Also: History Of Ulcerative Colitis Icd 10
Nutritious Foods To Combat Ulcerative Colitis Complications
People with ulcerative colitis commonly experience anemia and unintended weight loss. Anemia is a low red blood cell count caused by chronic blood loss. It can cause fatigue unless treated. For this reason, the nutrients folate, magnesium, calcium, and iron are of special importance for individuals with UC.
Furthermore, steroid medications such as prednisone may contribute to risk of osteoporosis, which puts emphasis on dietary intake of calcium, vitamin D, magnesium, and vitamin K. Here are the vital body functions that depend on each of these nutrients, along with food sources rich in each.
Calcium
Calcium is important for healthy bones, teeth, and the heart. The best food sources include dairy products, such as yogurt, milk, cottage cheese, and more. Nondairy sources of calcium include sardines , fortified soy milk and almond milk, tofu, kale, broccoli, and chia seeds.
Folate
Folate is crucial for cell division and DNA synthesis. It is found in avocados, black-eyed peas, spinach, Brussels sprouts, asparagus, and fortified breakfast cereals.
Iron
Iron is an important mineral that helps transport oxygen in red blood cells from the lungs to body tissues. It is found in fortified breakfast cereals, tofu, spinach, lentils, chickpeas, and cashews.
Magnesium
Magnesium is an important electrolyte that may be lost through sweating or diarrhea. Foods such as halibut, nuts, nut butters, spinach, potatoes with skin, black-eyed peas, and spinach are rich in magnesium.
Vitamin D
Ulcerative Colitis Diet: What To Avoid In A Flare Up
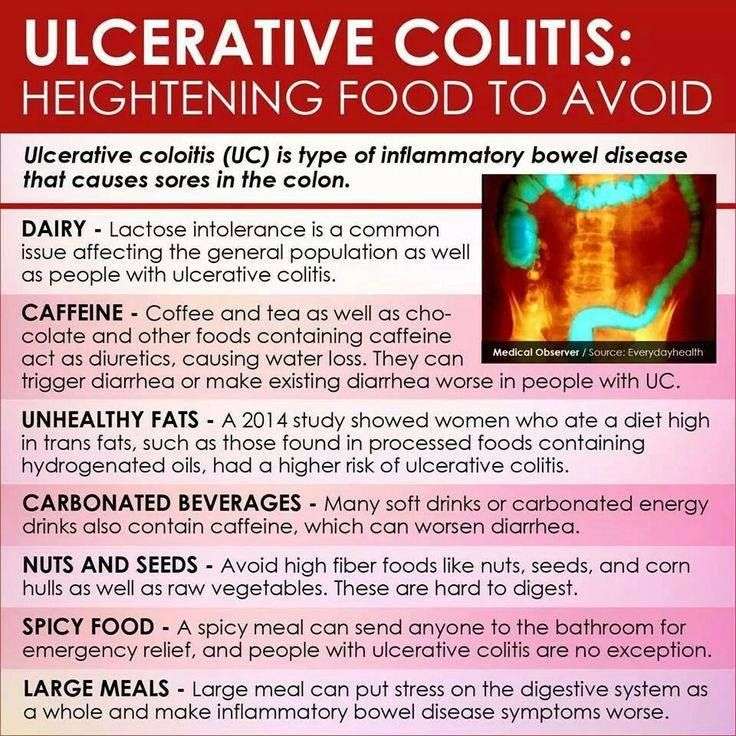
A study in the journal of Advances in Nutrition found that a high fat diet can increase intestinal permeability, something that is already a problem for those with ulcerative colitis. A review in the Mediators of Inflammation journal indicates that the upset caused to the gut wall by ulcerative colitis may also increase intestinal permeability and as such, reducing foods that also impact intestinal permeability, particularly during a flare up, is advisable.
A spokesperson from Crohns & Colitis UK explains that there is no one-size-fits-all approach to eating while in a flare up.
No particular diet has been proven to help people with ulcerative colitis, they say. Some people find that certain foods trigger symptoms or flare-ups but others do not. Everyone is different and what works for one person may not work for another. Theres no single diet that works for everyone. While changing your diet can help you manage your symptoms, it does not replace medical treatment. Its important not to make any changes to your diet without speaking to your IBD team or dietitian first.
You May Like: How To Tell Stomach Ulcer
An Ulcerative Colitis Diet: Summarizing The Evidence
Despite many reports online that certain diets or supplements can cure ulcerative colitis, the only known cure is total removal of the colon and rectum.
Those with digestive symptoms during remission may find relief from a low FODMAP diet to identify trigger foods.
A semi-vegetarian diet has also shown promise in maintaining remission in Crohns disease and may be helpful for ulcerative colitis, but we cannot make firm conclusions.
Even without following elimination diets, certain patterns have been shown to reduce symptoms:
- A diet that is rich in fruits and vegetables provides fiber and antioxidants, which are linked to lower disease risk. Reducing intake of high-fiber fruits and vegetables may increase comfort during flares.
- Limiting dietary fat, especially fatty meats, may be beneficial.
- Certain probiotics are helpful in bringing about and maintaining remission. Ask your doctor for a recommendation.
- A few herbal supplements show promise but lack sufficient scientific evidence to support their use.
- Avoid foods that irritate the gut during flares, including fatty foods, caffeine and alcohol.
A registered dietitian can help you identify foods that trigger your symptoms and design a well-balanced meal plan.
If you would like more information on how to eat for Ulcerative Colitis, which involves what we call a low FODMAP diet, tap the button below to download our Eat This, Not That list as well as additional resources for Ulcerative Colitis
SEND ME THE LIST
Reintroducing Your Usual Diet
Your IBD team and dietitian will give you information about returning to your usual diet after youve finished enteral nutrition. They may suggest reintroducing foods slowly so you can see if any foods affect your symptoms and to help you feel more confident about eating again. There are three ways of doing this:
- the elimination diet – after excluding all foods, they are reintroduced one by one every few days, to see if they cause problems
- the Royal Free method – this is similar to the elimination diet but foods are reintroduced more quickly, over a period of days rather than weeks
- the LOFFLEX diet – this excludes foods high in fat and fibre.
There isnt much evidence to show how well these diets work, or whether one works better than another. Your dietitian will explain the benefits and risks of all your options.
Ive found that you have to be very careful on the internet as there are many websites claiming to cure IBD through untested diets and supplements – which are not properly regulated and could be harmful and also expensive.
Zaineb
This is an extreme form of low carbohydrate diet that limits:
Read Also: Ulcerative Colitis High Calorie Diet
Eating With A Stricture
If you have a stricture , you may need to change what you eat to help prevent the intestine getting blocked.You might be advised to avoid foods that could block the intestine, such as:
If you have a severe stricture, you may only be able to eat very soft or liquid foods.Its important to speak to a dietitian to make sure youre eating a healthy, balanced diet. In some cases, they may recommend a vitamin and mineral supplement.
Is This Diet Effective
There are no formal published studies on the benefits of paleo in the management or prevention of IBD.
Similar to other diets, avoiding certain foods will help reduce inflammation and relieve symptoms of UC.
However, the paleo diet encourages the consumption of high levels of saturated fat in the form of red meat. Saturated fats have a high caloric content, which
hypothesize that germs may enter when there are gaps in the gut microbiota, inducing an autoimmune response. The AIP diet aims to target this to reduce inflammation and prevent autoimmune responses.
A on people with active IBD found improvements in UC and Crohnâs disease indexes and simple endoscopic scores that measure the size of ulcers.
Additionally, it can benefit other conditions. The showed that females on the AIP diet with Hashimotoâs thyroiditis experienced:
- improvements in quality of life
- less symptom burden
Read Also: Is Ginger Tea Good For Ulcerative Colitis
Herbal Remedies And Supplements
There are lots of supplements that claim to treat Crohns and Colitis. But there isnt enough evidence to recommend any herbal remedies or supplements. This is because its difficult to know whether the supplement is directly affecting a persons Crohns or Colitis or whether something else is causing a change in symptoms. Also, everyone is different so what helps one person may not help another.Some people find that some herbal remedies, such as aloe vera or curcumin , help them manage their symptoms when they use them together with their prescribed medicines. There have been reports of cannabidiol , an ingredient in cannabis, helping with symptoms like diarrhoea, pain and loss of appetite. But we dont know enough about how it works or how much is a safe amount to take. It isnt currently recommended and isnt available on prescription for people with Crohns or Colitis.There have been claims in the media about the benefits of kefir a fermented milk drink that contains probiotics. But there isnt any medical evidence to show that it helps people with Crohns or Colitis.If you want to take herbal remedies, its important to speak to your IBD team or dietitian first. Dont stop taking your prescribed medicine without talking to your IBD team, even if your symptoms improve.
I think it is so important to remember that the relationship with food and IBD is so different for everyone!
Read Also: Can You Donate Blood If You Have Ulcerative Colitis
Tips For Preparing Nutritious Foods For Uc
Its one thing to know which foods are nutritious for you, but another to safely consume them. As one MyCrohnsAndColitisTeam member put it, The hard part is getting your nutritional requirements in with limited choices. Practicing meal planning and preparation techniques can be helpful to ensure adequate nutrition.
Members often share creative ways theyve found to incorporate nutritious foods into their diet safely. I made some pureed green sauce with greens, anchovies, garlic, and EVOO to add to roasted veggies and soups, said one. I have a Nutri Ninja. It purees my fruits and veggies, so I eat lots of smoothies with almond milk and Activia yogurt added, shared another.
It may also be helpful to purchase meal replacements, such as protein shakes, to keep your weight up. One member had a tip for weight gain: I increase the recipes that use lots of natural fats olive oil, coconut oil, coconut cream, avocado and I might increase my red meat. All of those make me feel super healthy.
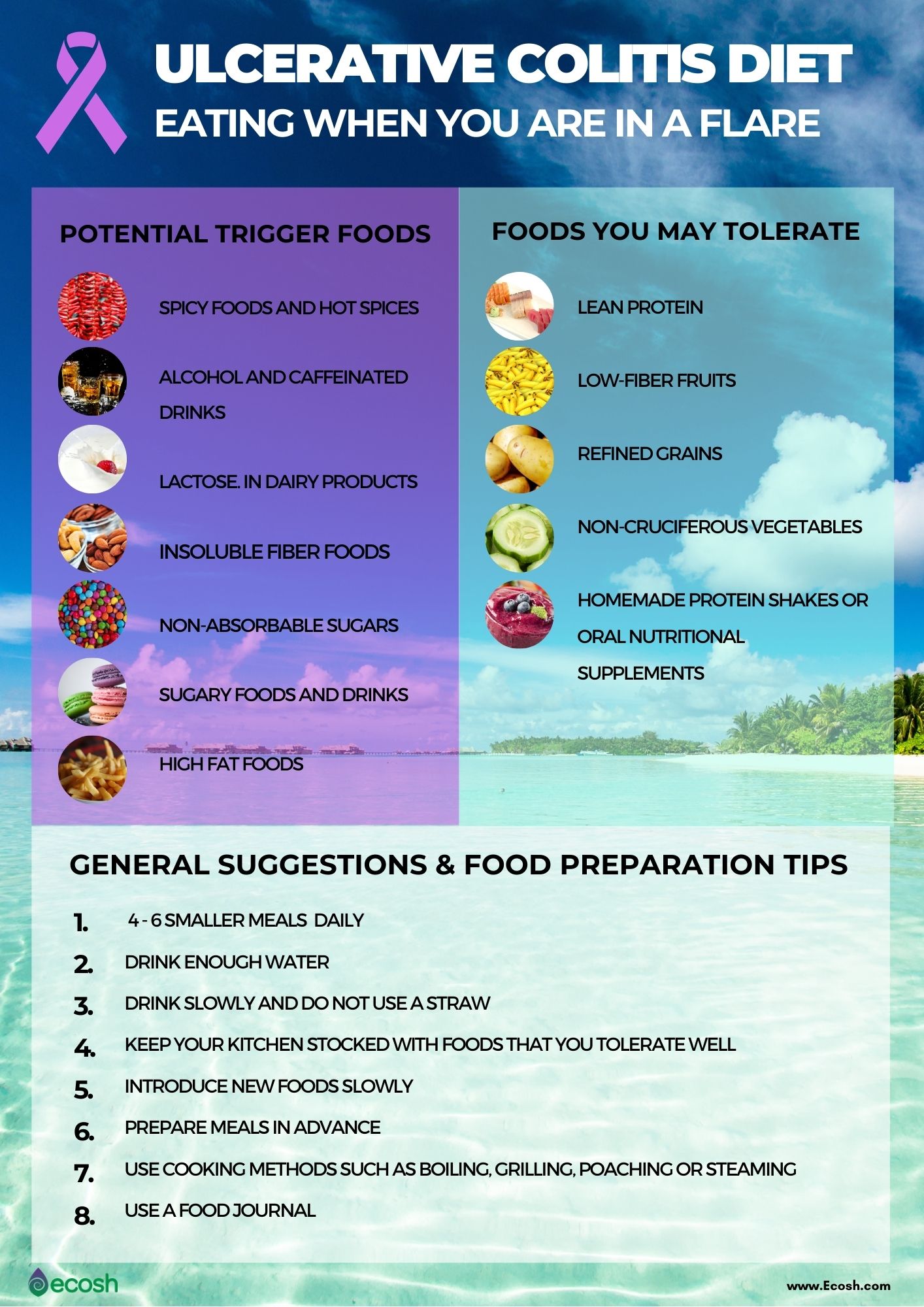
During a flare, ulcerative colitis symptoms become more severe, and certain foods can worsen them further.
Following these guidelines can keep you away from the most common food triggers during UC flares:
Don’t Miss: Ulcerative Colitis And Muscle Pain
Lifestyle Diet In Inflammatory Bowel Disease
Inflammatory bowel disease, also known as IBD, consists of Crohn’s disease and ulcerative colitis. No specific food, diet or lifestyle causes, prevents or cures inflammatory bowel disease. And multiple factors can trigger the diagnosis.
Your diet does not cause inflammatory bowel disease, or induce a flare. However, modifying your diet can manage symptoms during a flare.
While several specialized diets may help certain patients, no plan has been proven to prevent or control inflammatory bowel disease, except for enteral nutrition, which is delivered in a nutrient-rich formula.
Keeping a food diary is a great way to manage flare-ups. A dietitian specializing in inflammatory bowel disease may recommend a particular diet based on your symptoms.
These tips may help you manage inflammatory bowel disease:
Be careful with vitamins and mineral supplements. Remember, most of your needed vitamins are obtained by eating a balanced diet. Some over-the-counter supplements can contain lactose, starch and other ingredients that can worsen your symptoms.
Besides eating a recommended diet, some supplements may be suggested for patients with inflammatory bowel disease. Talk to your health care professional about healthy levels of calcium, vitamin D, folic acid, vitamin B12, iron and zinc.
As with any health condition, a healthy lifestyle makes it easier to manage your diagnosis:
Diana Franco Corso, M.D., specializes in gastroenterology and hepatology in Mankato, Minnesota.
Should You Take Nutritional Supplements With Uc
In some cases, you may not be able to get all your nutritional needs directly from food your intestines just cant do their best nutrient-absorbing job when its dealing with ulceration. Thats where come in. Again, its important to understand that theres not a set list of supplements that everyone with UC should takeit really varies from person to person.
Your GI or registered dietitian will recommend supplements based on your specific situation after looking at your symptoms and test results. And always get the green light from your doctor before adding a supplement to your routinesome may actually contain sugar alcohols, lactose, and preservatives that can actually aggravate your symptoms.
That said, here are some supplements that are commonly recommended for people with UCdont forget to take them on a full stomach, or else they could irritate your GI tract:
Keep in mind, this isnt an exhaustive list of possibilitiesyour doctor may recommend other vitamin or mineral supplements, including potentially a multivitamin, depending on your specific nutritional needs.
Don’t Miss: How To Diagnose Gastric Ulcer
Recommended Diet For Lymphocytic Colitis
Lymphocytic colitis occurs when all or part of your large or small intestines becomes inflamed. Symptoms include fecal incontinence, abdominal pain, watery diarrhea, weight loss and nausea. After performing a colonoscopy or flexible sigmoidoscopy to properly diagnose you with this condition, your doctor will recommend that you to alter your diet in addition to treating you with anti-inflammatory drugs and anti-diarrhea medications.
Video of the Day
What Foods Can I Eat When I Am Having An Ulcerative Colitis Flare
Certain foods are less likely to make your UC symptoms worse and can also help to reduce inflammation. These foods help settle your stomach and ensure you receive enough vitamins and minerals during an UC flare and include:
- Low-fiber fruits such as bananas, cantaloupe, honeydew melon, and cooked or canned fruits
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Refined grains, found in sourdough, potato or gluten-free bread, white pasta, white rice, mashed potatoes, and oatmeal
- Fully cooked, de-seeded, skinless, non-cruciferous vegetables such as asparagus tips, cucumbers, potatoes, and squash
- Homemade protein shakes or oral supplements
- Use olive oil instead of other oils or fats
- Apple sauce
- Herbal or green tea.
Recommended Reading: How To Calm An Ulcer
Eating When You Are In Remission
While theres no cure for UC, you may experience periods of remission. During this time, youll be symptom-free and your UC wont interfere with your daily life.
Theres no definitive way to avoid flare-ups forever, but you can prolong your remission periods by maintaining a diverse and nutrient-rich diet that does not include trigger foods.
To stay symptom-free, it may be helpful to follow one of the diets that other individuals with UC find successful, as well as introduce new foods slowly and stay hydrated.
However, its important to consult with your doctor or dietician before making any changes to your diet.
Some foods that may help keep you feeling good and hydrated during remission
Food Prep And Meal Planning
Although there is no cure for UC, meal planning and prepping food ahead of time can help people living with UC limit foods that trigger their symptoms.
Planning meals, snacks, and even your hydration efforts in advance gives you control over everything youll be consuming.
With preparation, you can avoid making quick decisions when youre hungry or thirsty that could result in a flare-up.
Taking the time to plan out your meals and read nutrition labels may take a couple of hours initially, but it can save tons of time throughout the week overall. Helpful steps include:
- buying ingredients in bulk
- cooking in batches
- preportioning your meals before storing them in the fridge or freezer, making them easier to reheat and eat
Not only will you have your meals prepared ahead of time, but youll also help limit food triggers, allowing you to feel better and be more productive overall. Buying and planning your snacks ahead of time is a good way to avoid reaching for trigger foods, too.
Additionally, because frequent diarrhea from UC can cause you to lose more fluid than you put into your body, planning water intake can help you avoid dehydration.
Constipation can be a symptom for some individuals, and their dietary needs may differ.
Don’t Miss: Does Ulcerative Colitis Make You Tired