Diagnosis Of Ulcerative Colitis
X-rays of the abdomen taken after barium is given by enema do not require any special preparation . These x-rays usually can show a blockage or paralysis… read more ) may indicate the severity and extent of the disease but are not done when the disease is active, such as during a flare-up, because of the risk of causing a perforation. Other x-rays of the abdomen may also be taken.
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Outlook For People With Ulcerative Colitis
If you have UC, a doctor will need to monitor your condition, and youll need to carefully follow your treatment plan throughout your life.
The only true cure for UC is removal of the entire colon and rectum. Your doctor will usually begin with medical therapy unless you have a severe complication that requires surgery. Some people will eventually require surgery, but most do well with nonsurgical therapy and care.
You May Like: Ulcer Cause Blood In Stool
How Do You Take Adalimumab
Adalimumab is administered by subcutaneous injection at regular intervals . Subcutaneous means that an injection is given into the fat between your skin and muscle.
Some people administer the injection themselves at home, while others receive it from a nurse. If you are considered suitable to self-administer you will receive full training from a qualified professional who will teach you how to do it and observe you the first couple of times. If you are self-administering adalimumab your dosages will be delivered to you in loaded pens with a short needle under the cap. These pens need to be kept refrigerated.
The first time you receive adalimumab will be your loading dose. This will be a higher dose than the usual dose you will receive. The loading dose is usually 160mg of adalimumab – four loaded pens. The second dose is taken 2 weeks later – usually 80mg or 2 loaded pens. After that you will usually take 40mg every two weeks.
If you are self-administering your adalimumab you will be provided with a sharps bin to discard of the used pen.
Some people report that adalimumab stings when it is administered.
Treatment Of Ulcerative Colitis
Vedolizumab is a drug for people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The most serious side effect it causes is increased susceptibility to infection. Vedolizumab has a theoretical risk of a serious brain infection called progressive multifocal leukoencephalopathy Progressive Multifocal Leukoencephalopathy Progressive multifocal leukoencephalopathy is a rare infection of the brain that is caused by the JC virus. People with a weakened immune system are most likely to get the… read more because this infection has been reported with the use of a related drug called natalizumab.
Ustekinumab is another kind of biologic agent given to people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The first dose is given by vein and then by injections under the skin every 8 weeks. Side effects include injection site reactions , cold-like symptoms, chills, and headache.
Recommended Reading: How To Reduce Bloating With Ulcerative Colitis
Best Methods Of Marijuana Treatment For Ulcerative Colitis Symptoms
Now you know how medical pot can help you, lets look at the methods of marijuana treatment so you can decide which to use to treat your ulcerative colitis symptoms:
- Smoking. Smoking pot gives you instant relief and is inexpensive. However, smoke could harm your lungs, and youll smell of cannabis.
- Vaping. Vaping provides fast relief, doesnt make you smell as much as smoking and isnt as harsh on your lungs as smoking a joint.
- Juices. You can blend raw, fresh cannabis leaves with some healthy juice. Drinking juice is a good option if you have little appetite.
- Sprays. Cannabis sprays come in a variety of mild flavors.
- Tinctures. These are alcohol-based extracts that you add to your food and drinks.
- Suppositories. Dispensaries also sell medical pot in suppository form. You can purchase suppository-making kits in health food stores, or you can buy them online.
- Edibles. You can buy or make your own edibles. You can also buy cannabis-infused lollipops and lozenges that are perfect if youve no appetite.
The medical community has woken up to the benefits of medical pot in recent years. It no longer has the stigma it once had, and for a good reason. If you or someone you love are seeking a way to naturally and gently relieve your UC symptoms, search for a medical marijuana doctor or dispensary today to find out more about cannabis and ulcerative colitis.
When To Call The Doctor
- Cramps or pain in your lower stomach area
- Bloody diarrhea, often with mucus or pus
- Diarrhea that cannot be controlled with diet changes and drugs
- Rectal bleeding, drainage, or sores
- Fever that lasts more than 2 or 3 days, or a fever higher than 100.4°F without an explanation
- Nausea and vomiting that lasts more than a day
- Skin sores or lesions that do not heal
- Joint pain that keeps you from doing your everyday activities
- A feeling of having little warning before you need to have a bowel movement
- A need to wake up from sleeping to have a bowel movement
- Failure to gain weight, a concern for a growing infant or child
- Side effects from any drugs prescribed for your condition
You May Like: Remicade Infusion For Ulcerative Colitis
Ulcerative Colitis Diet: Advice From A Dietitian
If you have ulcerative colitis, knowing what to eat can be tricky. Its important to customize your food choices based on your current tolerance and health goals. This post will help you understand the current scientific thinking on ulcerative colitis and diet and how to move forward with the approach that is right for you.
We have been working with clients with Crohns disease and ulcerative colitis in our practice for over seven years its an area I am passionate about because of the massive toll these diseases take on peoples quality of life. I also believe that nutrition can play a much larger role in the management of the diseases than is often discussed in the doctors office.
As a dietitian, I believe that the goal of nutrition is more than just ensuring you get all the vitamin D you need. I believe and have seen firsthand in my practice that creating a strong individualized approach to nutrition can help people find healing and learn how to thrive, no matter their diagnosis. Which is why it is frustrating that much of the scientific literature on ulcerative colitis is focused on either associating the risk of disease with certain foods, or acute strategies for securing remission in a flare.
The Main Types Of Drugs
The aim of drug treatment for Ulcerative Colitis is to reduce inflammation. The main types of drugs are:
Aminosalicylates reduce inflammation in the lining of the intestine. Examples include mesalazine , olsalazine , sulphasalazine and balsalazide .
Corticosteroids work by blocking the substances that trigger allergic and inflammatory responses in your body. They include prednisolone, prednisone, methylprednisolone, budesonide , hydrocortisone and beclometasone dipropionate .
Immunosuppressants suppress the immune system, and reduce levels of inflammation. The main immunosuppressants used in IBD are azathioprine , mercaptopurine or 6MP , methotrexate, ciclosporin and tacrolimus. They are often used in patients who relapse when they come off steroids.
Biological drugs are the newest group of drugs used to treat IBD. Anti-TNF drugs, such as infliximab , adalimumab and golimumab target a protein in the body called TNF, or tumor necrosis factor, preventing inflammation. Another type of biological drug is vedolizumab , which works by stopping white blood cells from entering the lining of the gut and causing inflammation.
You can find more information about some of the drugs used for Colitis: Adalimumab, Aminosalicylates , Azathioprine and Mercaptopurine, Biologic Drugs, Golimumab, Methotrexate, Infliximab, Steroids, Ustekinumab and Vedolizumab.
About a quarter of people diagnosed with Crohn’s or Colitis are children or adolescents at the time they are diagnosed.
You May Like: What Causes Ulcers On The Feet
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
What Is Uc Cramping
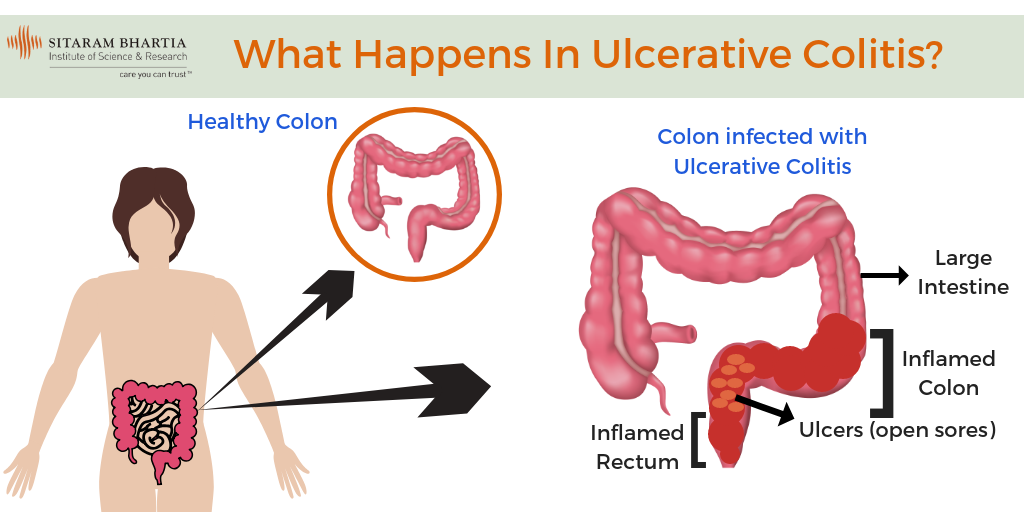
Abdominal pain and cramping from UC is most commonly caused by the conditions inflammatory process, according to Christina Ha, MD, a gastroenterologist at Cedars-Sinai Medical Center in Los Angeles. Such inflammation usually starts at the rectum and moves throughout the large colon. The greater the inflammation, the more severe the pain.
Also Check: How To Heal Venous Stasis Ulcers
What Is Ulcerative Colitis Exactly
Ulcerative colitis is one of the two main forms of inflammatory bowel disease . The other is Crohns disease. U.C. occurs when the immune system malfunctions, causing inflammation and ulcers to appear on the inner lining of the large intestine, according to the National Institute of Diabetes and Digestive and Kidney Diseases . Its not comfortable, to put it mildly, and not something that will clear up quickly.
Ulcerative colitis is a chronic illness that does not yet have a medical cure. That doesnt mean nothing can be done though, so dont despair if youre experiencing symptoms. Sidhartha Sinha, M.D., a gastroenterologist, assistant professor at Stanford Medicine, and researcher who specializes in IBD, tells SELF that while there arent medical cures for ulcerative colitis, there are medical treatments. And we have made great advancements in these treatments, he says. The last resort is a surgical option called colectomythe removal of the entire colonwhich can eliminate U.C. entirely.
Foods To Avoid With Ulcerative Colitis
- Added sugars and hyper-processed foods
Our North American love affair with low fibre, high sugar and high fat hyper-processed food is associated with our risk of ulcerative colitis. It is this type of eating that is thought to drive gut dysbiosis or the overgrowth of more pro-inflammatory gut bacteria that can harm gut barrier integrity leading to leaky gut and inflammation. In laboratory studies, this type of diet can decrease the number or acetate and butyrate producing bacteria and increase the risk of colitis.
Another issue with hyper-processed foods is that they contain emulsifiers like xanthan gum and carrageenan which may alter gut barrier integrity. While their true impact on gut health is still hotly debated, in one double-blinded trial, people with ulcerative colitis on a carrageenan free diet had lower relapse rates than those given two capsules of carrageenan. For me, this would not be the first place I look when adjusting someones diet instead, it would be a refinement only after taking more global steps towards a more whole foods, plant-based approach.
- Meat, particularly red meat
If you arent a huge fan of red meat, ditch it entirely. If you truly love red meat, try to limit yourself to one 3-4 ounce portion every week or two, no more.
- Dairy
Dairy could be impacting symptoms for a few reasons:
- Omega 6-rich cooking oils like soy, corn and safflower oils
Recommended Reading: Ulcerative Colitis Diet Plan During Flare Up
Common Symptoms Of Ulcerative Colitis
While UC symptoms can vary over time and from person to person, the most common symptoms are diarrhea with blood and abdominal discomfort.
However, your symptoms may vary depending on where inflammation occurs in your GI tract and how severe it is.
Other signs and symptoms include:
- An urgent need to have a bowel movement
- Feeling tired
- Nausea or loss of appetite
- Weight loss
- Fever
- Anemiaa condition in which the body has fewer red blood cells than normal
Is There A Cure For Nsaid
Pathogenesis of NSAID-induced colitis is still controversial. Local and/or systemic effects of NSAIDs on mucosal cells might lead to an increased intestinal permeability, which is a prerequisite for colitis. Treatment of NSAID-induced colitis should be to discontinue the drug, or at least, to reduce the dose as much as possible.
Don’t Miss: Different Stages Of Pressure Ulcers
How Does Ulcerative Colitis Progress
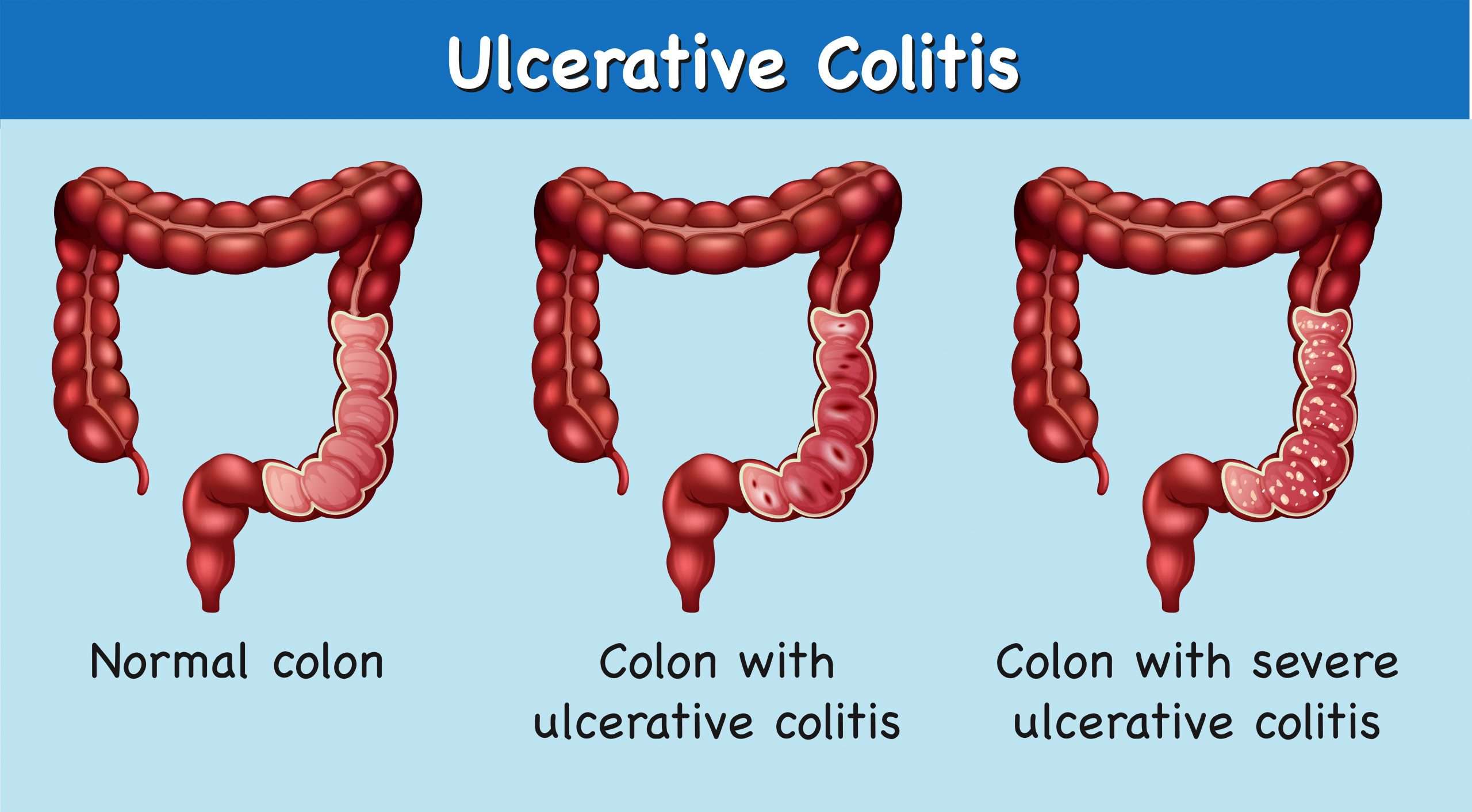
Ulcerative colitis is a chronic, relapsing condition. Chronic means that it is persistent and ongoing. Relapsing means that there are times when symptoms flare up and times when there are few or no symptoms . The severity of symptoms and how frequently they occur vary from person to person. The first flare-up of symptoms is often the worst.
It starts in the rectum in most cases. This causes a proctitis, which means inflammation of the rectum. In some cases it only affects the rectum and the colon is not affected. In others, the disease spreads up to affect some, or all, of the colon. Between flare-ups the inflamed areas of colon and rectum heal and symptoms go away. The severity of a flare-up can be classed as mild, moderate or severe:
- Mild – you have fewer than four stools daily and only have small amounts of blood in your stools. You do not feel generally unwell .
- Moderate – you have four to six stools a day, have some blood in your stools but do not feel generally unwell in yourself .
- Severe – you have more than six stools a day and have blood in your stools. You also feel generally unwell with more marked systemic disturbance with things such as high temperature , a fast pulse rate, anaemia, etc.
What Should You Know About Biologic Administration Doses And Schedules
A variety of biologic drugs are used to treat Crohn’s disease and ulcerative colitis. Some biologics treat both conditions, while others treat only one. There are several ways biologics are administered, dosed, and scheduled. Talk to your gastroenterologist and health care team about the specific usage guidelines for your prescribed medications.
Biologics used to treat Crohn’s disease and ulcerative colitis include a class of drugs called tumor necrosis factor-alpha inhibitors that target specific inflammatory proteins in the immune system. Some of these include:
Other biologic drugs known as integrin receptor antagonists block a protein on the surface of cells that cause inflammation. This process keeps the proteins from leaving the blood vessels and entering tissues. Examples of integrin receptor antagonists are Tysabri and Entyvio .
A third type of biologic targets interleukin proteins in the immune system, including IL-12 and IL-23, to reduce inflammation. Stelara is an example of an interleukin inhibitor that treats IBD.
Read Also: How To Use Aloe Vera Gel For Ulcerative Colitis
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
How Is Ulcerative Colitis Different From Crohns Disease
Ulcerative colitis is different from other inflammatory bowel diseases like Crohns disease. Crohns can affect any area of the gastrointestinal tract, including the small intestine and colon. Ulcerative colitis, on the other hand, affects only the colon. The inflammation involves the entire rectum and extends continuously up the colon. There are no normal areas of the intestine between the areas of ulceration. In Crohns, the inflamed areas are scattered and can affect the entire thickness of the bowel wall.
You May Like: What Medicine Is Best For Stomach Ulcers
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you haven’t been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If you’ve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you can’t contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
What Does Ulcerative Colitis Look Like

With UC there is a wide variation in the amount of inflammation from person to person, so that in mild cases the bowel can look almost normal but, when the inflammation is bad, the bowel can look very red and ulcerated. Ulcerative colitis usually affects the rectum, but occasionally there is no inflammation . Sometimes the inflammation is limited just to the rectum . However, the inflammation can involve varying lengths of the colon. When the whole large bowel is affected, this is called pan-colitis .
Read Also: Can Ulcers In The Colon Be Cancerous
Testing For Ulcerative Colitis
Often, symptoms alone can provide doctors with the information they need to diagnose ulcerative colitis. Your doctor will perform a physical examination and take a complete medical history that includes a careful review of your symptoms. For this reason, it is important to be candid and specific with your doctor about the problems you are having.
There is no one specific laboratory test, X-ray or scope to diagnose ulcerative colitis, however, to help confirm the condition and rule out other problems, your doctor may send you to have one or more of the following tests: