Symptom Development And Flares
The symptoms of UC usually start out fairly mild, such as slightly looser or more frequent bowel movements. The symptoms may become more severe as inflammation worsens and open sores develop in the bowel. Eventually, a person with UC might experience fatigue, fever, nausea, and weight loss.
Some people experience ulcerative colitis constantly. However, it is more common to have flare-ups, during which symptoms begin or worsen, followed by periods of remission, when symptoms go away or improve for a while.
What Do Chills Feel Like With Ibd
Many people with IBD experience chills. MyCrohnsAndColitisTeam members describe this symptom in different ways. As one shared, Its like I cannot get warm.
Some people find that chills are accompanied by other symptoms, like fevers: I get flu-like episodes which come on suddenly, wrote one member. Headache, very sore neck and back, big spike in temperature, alternating sweats and chills. Its gone by the next morning. Another shared, The night sweats are horrible! My sheets are soaked every morning.
Sometimes, these chills and other flu-like symptoms are what spur a person with IBD to see a doctor in the first place. If a persons gastrointestinal symptoms are not particularly severe, fever and chills might be the first indication that something is wrong. As one member commented, Fevers and chills were part of what led to my Crohns diagnosis.
These symptoms may occur during IBD flares in some cases, even without accompanying gastrointestinal symptoms. Fever and chills are part of the symptoms of a Crohns flare-up I had, shared one member. These were the only symptoms for about a week.
However, some people with IBD experience these symptoms on a regular basis. For the past month or so, I have been getting chills while I have a bowel movement, and they are getting worse each day, one member wrote.
Growth And Development Problems For Children
You can get ulcerative colitis at any age, but its more common among 15- to 30-year-olds. A child with UC may:
- Be underweight
- Red or discolored
Continued
Talk to your doctor right away if youre worried that you might have DVT. Its possible for a deep-vein blood clot to break loose and get stuck in a lung artery. If that happens, its an emergency called a pulmonary embolism . You could have symptoms like shortness of breath, sharp chest pain, and a cough with or without blood. Call 911 if you have these signs.
Doctors can treat DVT and pulmonary embolisms with medications, a filter through a vein that removes the clot, or surgery.
You could be more likely to get DVT or PE if you:
- Have ulcerative colitis that flares often or affects a large amount of your colon.
- Get surgery for severe ulcerative colitis.
Some studies also link certain ulcerative colitis meds, like steroids or tofacitinib, to DVT and PE.
Read Also: How To Reduce Bloating With Ulcerative Colitis
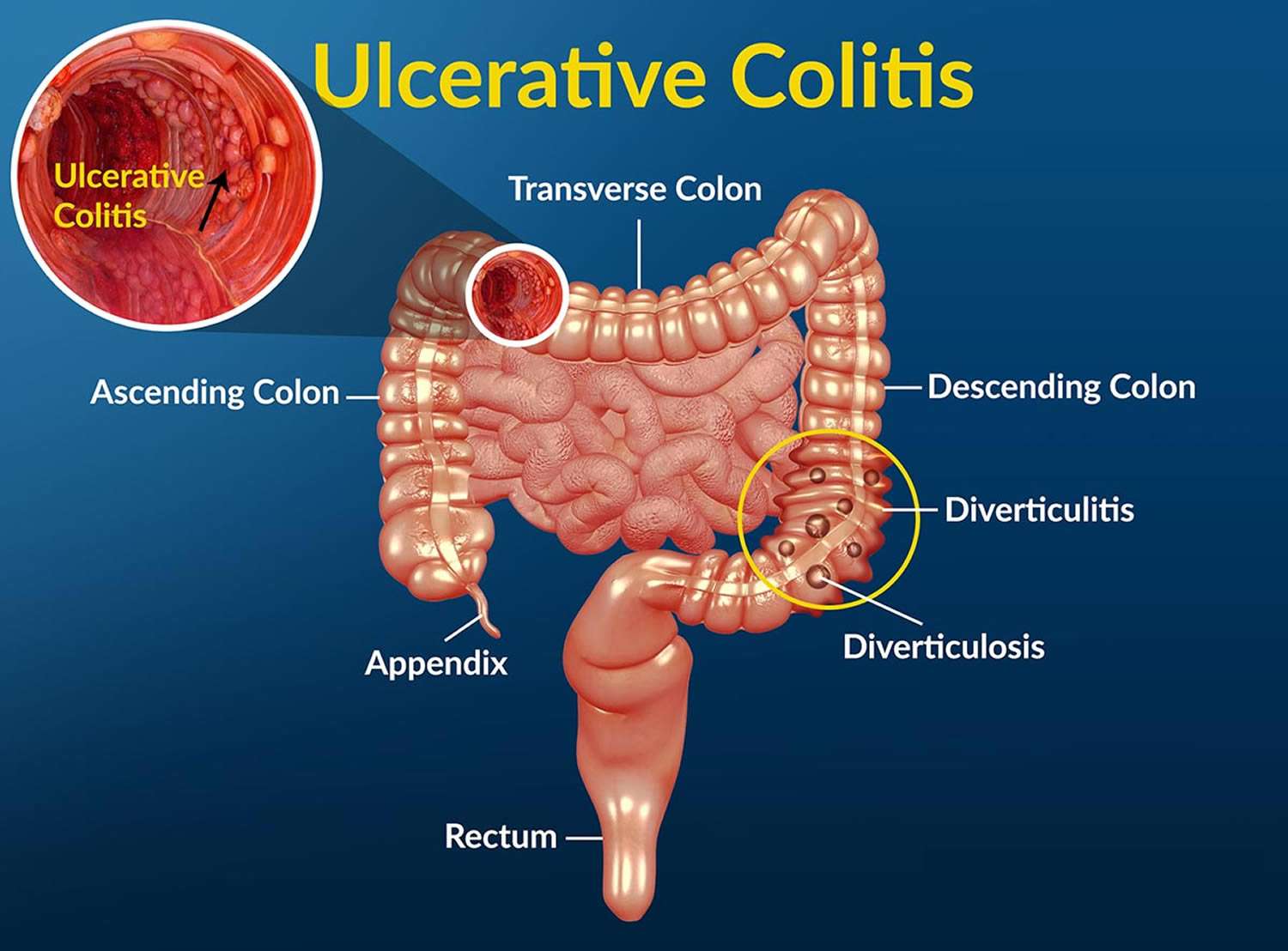
Perforation Of The Colon
Long-term inflammation and ulcers in the colon can weaken the intestinal wall. Over time, these weaknesses may develop into a perforation.
A perforation can allow bacteria and other intestinal contents to leak out into the abdomen, causing a serious condition called peritonitis.
Peritonitis is the inflammation of the peritoneum, which is the lining of the abdomen. This condition may cause the abdomen to fill with fluid. It can also lead to blood poisoning and sepsis, which is a whole-body inflammatory response to infection.
One in three people who develop sepsis die from the condition.
Symptoms
It is vital to know the symptoms of a perforated colon to help prevent peritonitis and sepsis. According to the , these may include:
- severe stomach pain
- chills
- fever
A perforated colon is a medical emergency that usually requires surgery to repair the hole in the intestines.
People who experience sepsis also require urgent treatment with antibiotics and fluids.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Recommended Reading: What Is An Ulcer Diet
Get Support For Your Ibd Today
MyCrohnsAndColitisTeam is the social network for people diagnosed with IBD and the people who love, support, and care for them. More than 142,000 members come together to ask questions, give advice, and share their experiences of life with IBD.
Have you experienced chills with Crohns disease or ulcerative colitis? Share your experience in the comments below or by posting on MyCrohnsAndColitisTeam.
Uc And Your Mental Health
It almost goes without saying that UC can have a major impact on your mental health. The mind-gut connection is real, meaning that everyday stress can manifest in digestive symptoms. Of course, this relationship goes both ways, too: Stress can cause GI symptoms that can cause stress you get the idea.
Whats more is that research, like this study in the Canadian Journal of Gastroenterology and Hepatology, shows that people with IBD are at increased risk of developing symptoms like anxiety and depression, and sometimes full-blown depressive or anxiety disorders.
Its no wonderliving with a condition like UC thats shrouded in stigma can be isolating, and the fear of symptoms flaring up unexpectedly is often anxiety-provoking and stressful. When your symptoms can interfere with your ability to go to work, go to school, or even just hang out with friends and family, it can take a serious toll on your mental health.
Building a strong support system of friends, family, and your health care team is important to remove some of that emotional burden. Working with a therapist is also a valuable optionthey can teach you techniques to reduce your anxiety, transform your mindset, and more.
Read Also: Stomach Ulcer Foods To Eat
Ulcerative Colitis: When To Call
if you have been diagnosed with ulcerative colitis and you have:
- Fever over 101°F or shaking chills.
- Lightheadedness, passing out, or a rapid heart rate.
- Stools that are almost always bloody.
- Severe dehydration, such as passing little or no urine for 12 or more hours.
- Severe belly pain with or without bloating.
- Pus draining from the area around the anus or pain and swelling in the anal area.
- Repeated vomiting.
- Not passing any stools or gas.
If you have any of these symptoms and you have been diagnosed with ulcerative colitis, your disease may have become significantly worse. Some of these symptoms also may be signs of toxic megacolon. This is a condition in which the colon swells to many times its normal size. It requires emergency treatment. Left untreated, it can cause the colon to leak or rupture. This can be fatal.
People with ulcerative colitis usually know their normal pattern of symptoms. Call your doctor if there is a change in your usual symptoms or if:
- Your symptoms become significantly worse than usual.
- You have persistent diarrhea for more than 2 weeks.
- You have lost weight.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
You May Like: What Is Ulcer Pain Like
What Foods Cause Colitis
Foods with high fiber content like brown rice, quinoa, oats can trigger the symptoms of Colitis especially Ulcerative colitis . It is difficult to digest high fiber foods which increase the bowel movements and abdominal cramps. Caffeine. Coffee, tea and other caffeine-rich drinks are known to flare up the UC.
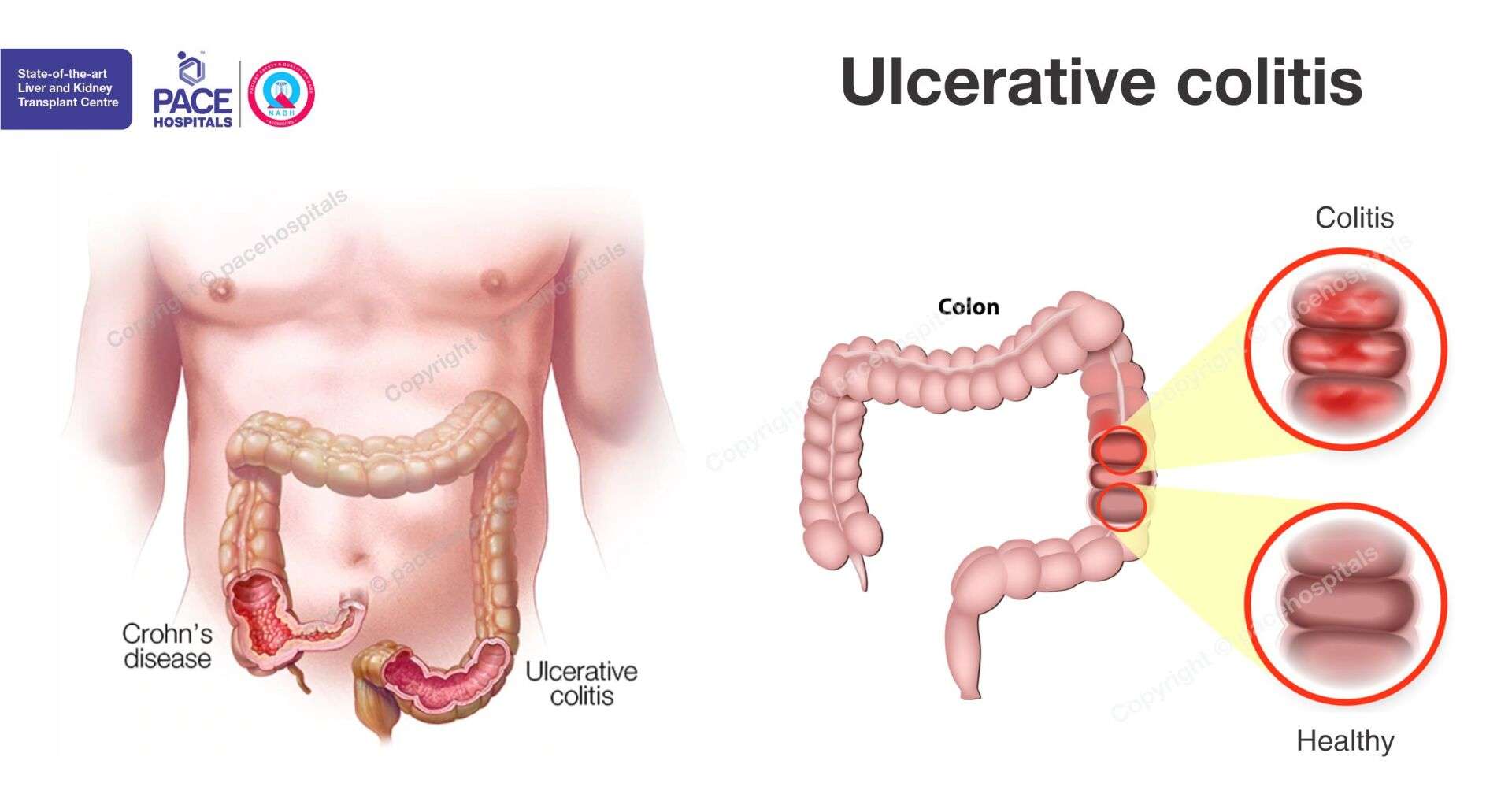
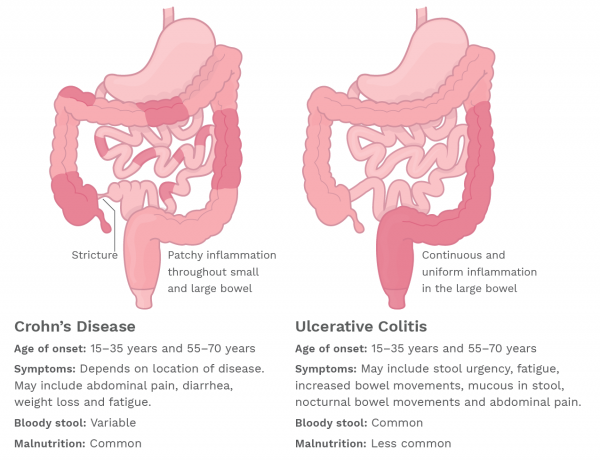
Crohns Disease And Ulcerative Colitis
A serious but rare complication of these forms of inflammatory bowel disease is fulminant or toxic colitis, formerly called toxic megacolon.
The signs and symptoms of this condition can include bloody diarrhea along with fever, racing heartbeat , low blood pressure , metabolic acidosis , low urine output , and acute kidney failure.
Toxic colitis is more common with ulcerative colitis than it is with Crohns disease.
Read Also: Best Supplement For Gastric Ulcers In Horses
Are There Different Types Of Uc
When you get diagnosed with UC, your gastroenterologist may tell you that you have a certain type of UC. There are a few different subtypes, and each can have slightly different symptoms. Heres a breakdown.
-
Ulcerative proctitis. In this type of UC, the inflammation is confined to the rectum, rather than both the rectum and the colon. Symptoms of this type of UC include rectal pain and bleeding and a sense of urgency to have bowel movements.
-
Left-sided colitis. In left-sided colitis, inflammation can extend from the rectum to the splenic flexure, a bend in the colon near your spleen. Another type of UC called proctosigmoiditis also falls under the umbrella of left-sided colitis, and it affects your rectum and the sigmoid colon, which is the lower part of your colon. Symptoms of these types of UC include bloody diarrhea, weight loss, reduced appetite, and pain on the left side of your abdomen.
-
Extensive colitis. This type of UC involves usually inflammation involving the entire colon is called pancolitis. Symptoms include bloody diarrhea, abdominal pain, weight loss, and reduced appetite.
What Are The Complications Of Ulcerative Colitis
UC can also lead to complications, especially if left untreated or if you dont follow the directions for your medications to a T . Common complications of UC include:
-
Rectal bleeding, which can lead to iron-deficiency anemia
-
A rupture of the bowel
-
Increased risk of colon cancer
-
Deficiencies in vitamins and minerals, which can lead to bone loss in the form of osteopenia or osteoporosis
-
Inflammation throughout the body, such as the eyes, skin, and joints
If youve had surgery for UC, keep in mind there may be surgical complications as well. Talk with your doctor about any warning signs to watch for.
Read Also: How Do You Get Ulcers In Your Stomach
Where And How Does Ulcerative Colitis Start
Ulcerative colitis is an inflammatory bowel disease . This chronic digestive disorder is characterized by inflammation in the colon and the rectum. People diagnosed with ulcerative colitis can develop sores on the inside of their large intestine, which can lead to bleeding, diarrhea, and other symptoms.
If youve experienced these symptoms or have been diagnosed with ulcerative colitis, you may be unsure exactly how the disease began. Heres what you need to know about where in the body ulcerative colitis starts and how.
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
- low energy
- weight loss
Ulcerative coliits can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow well as well as other kids their age and puberty may happen later than normal.
Don’t Miss: How Effective Is Humira For Ulcerative Colitis
Signs Your Ibd May Be Flaring
Robert Burakoff, MD, MPH, is board-certified in gastroentrology. He is the vice chair for ambulatory services for the department of medicine at Weill Cornell Medical College in New York, where he is also a professor. He was the founding editor and co-editor in chief of Inflammatory Bowel Diseases.
Recognizing Acute Severe Ulcerative Colitis
Also known as fulminant colitis, this complication affects less than 10 percent of people with ulcerative colitis and involves damage to the entire thickness of the intestinal wall, according to the Crohn’s and Colitis Foundation.
In fulminant colitis, the whole lining of the colon becomes inflamed, causing severe symptoms like bloody diarrhea and belly pain. Unless the inflammation is brought under control, patients with fulminant colitis are at risk of developing toxic megacolon, the most severe form of colitis.
Call your healthcare provider immediately if you notice your loved one is having more than six bowel movements per day that include a lot of blood, accompanied by any one of the following: a fast heart rate, a fever, a low temperature, and signs of anemia . These are signs that their ulcerative colitis has become severe, according to the American Gastroenterological Association.
It’s essential for acute severe ulcerative colitis to be recognized early and that the patients condition is monitored closely while they receive intravenous corticosteroids, according to a review published in January 2019 in the BMJ Postgraduate Medical Journal. Patients will also need to receive fluids intravenously to replenish electrolytes.
RELATED: Are Your Ulcerative Colitis Symptoms Under Control?
You May Like: Whey Protein And Ulcerative Colitis
Treatment Of Ulcerative Colitis
Vedolizumab is a drug for people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The most serious side effect it causes is increased susceptibility to infection. Vedolizumab has a theoretical risk of a serious brain infection called progressive multifocal leukoencephalopathy Progressive Multifocal Leukoencephalopathy Progressive multifocal leukoencephalopathy is a rare infection of the brain that is caused by the JC virus. People with a weakened immune system are most likely to get the… read more because this infection has been reported with the use of a related drug called natalizumab.
Ustekinumab is another kind of biologic agent given to people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The first dose is given by vein and then by injections under the skin every 8 weeks. Side effects include injection site reactions , cold-like symptoms, chills, and headache.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Recommended Reading: Ulcerative Colitis Surgery Pros And Cons
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Complications Of Ulcerative Colitis
Problems from ulcerative colitis can include:
- Narrowed areas of the intestine . They can make it hard to pass stools.
- Increased risk of cancer of the colon and rectum. This risk is higher than average if you have had ulcerative colitis for 8 years or longer.
- Complications outside the digestive tract. These include joint pain, skin problems, and eye problems.
- The colon swelling to many times its normal size. This is called toxic megacolon. It’s rare, but it needs treatment right away.
- Other rare complications, such as scarring of the bile ducts and the pancreas.
- Inflammatory bowel disease, which also increases the risk of melanoma, a serious type of skin cancer. Your doctor may recommend regular screening by a dermatologist.footnote 2
Also Check: How To Use Aloe Vera Gel For Ulcerative Colitis
How Is Fever Treated
General advice for a fever is to drink plenty of fluids. Do not bundle up with extra layers of clothing or bedding. This can cause your temperature to rise higher. Set the room to a comfortable temperature.1
Acetaminophen may be a better option than ibuprofen for treating a fever.10 There is concern that taking ibuprofen could worsen a IBD flare. Ask your health care provider what type of over-the-counter medications you should take for a fever.
Fever plus bloody diarrhea, pain, abdominal swelling, rapid heart beat, dehydration, or low urine output could be serious. These are symptoms of toxic megacolon, a rare but life-threatening complication of Crohns disease and ulcerative colitis. If you have these symptoms, seek medical care right away.