Wound Care And Dressings
Care for your wound as instructed by your provider. Other instructions may include:
- Keep your blood sugar level under good control. This helps you heal faster and helps your body fight infections.
- Keep the ulcer clean and bandaged.
- Cleanse the wound daily, using a wound dressing or bandage.
- Try to reduce pressure on the healing ulcer.
- Do not walk barefoot unless your provider tells you it is OK.
Q: What Is A Podiatrist
A: Podiatrists are Doctors of Podiatric Medicine, DPM. Podiatrists are also known as podiatric physicians, foot doctors, or podiatric surgeons. Podiatrists often diagnose and treat the foot, ankle, and other related structures of the leg.
Podiatrists receive similar training that other doctors complete. They complete four years of training in a podiatric medical school and three years of hospital residency training.
The podiatrists at Prime Foot & Ankle Specialists have received extra training such as fellowships beyond residency and board certifications by the board of foot and ankle surgery and the board of podiatric medicine.
Can I Avoid Diabetic Foot Ulcers
The best way to treat diabetic foot ulcers is to avoid them in the first place. The first step in preventing a foot ulcer is to control your blood sugar. Elevated blood sugar creates nerve damage, which can trigger foot problems.
Diabetic feet often have increased pain and swelling, and cold and warm baths can help. Warm water increases blood flow while cold water baths reduce inflammation. You can alternate between the two or add ice massages for optimal relief.
Staying active helps improve circulation and decrease your risk of developing nerve damage. Regular walking helps manage your blood sugar and prevent diabetic neuropathy, which is associated with diabetic foot ulcers.
Be sure to wear proper footwear and avoid shoes that cause the blisters, calluses, and sores that lead to diabetic ulcers. Our podiatrists can help fit you for diabetic shoes or inserts to ensure the best preventive care for your feet.
Finally, if you have diabetes its important to develop a healthy foot care routine with the help of a diabetic foot care specialist. Specialized care includes:
- Regular foot examinations
- Professional care of calluses and corns
- Treating wounds and blisters
- Trimming toenails to prevent injury
Don’t Miss: What Foods Not To Eat If You Have An Ulcer
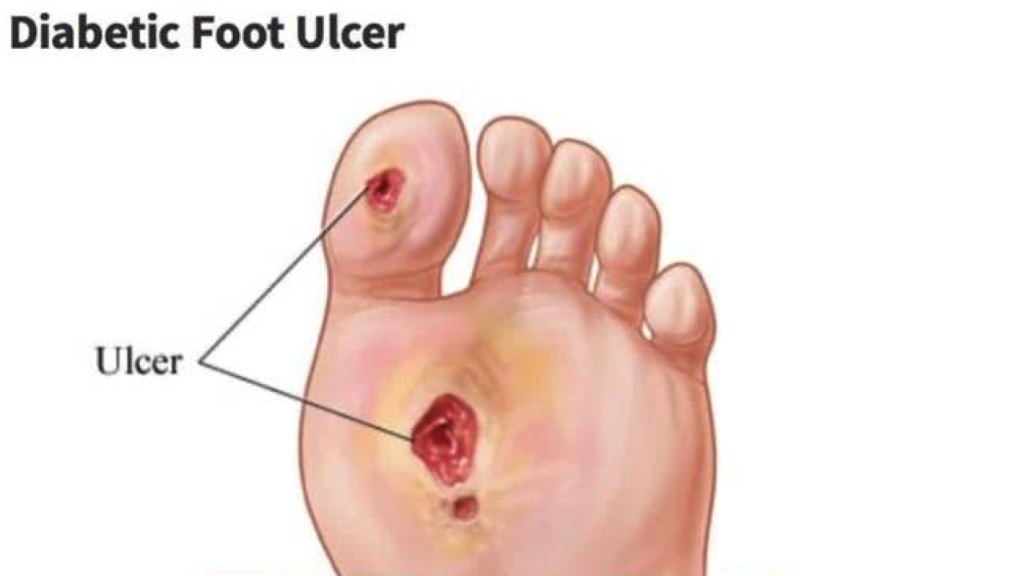
What Are Foot Ulcers
A foot ulcer is an open sore on the foot.
A foot ulcer can be a shallow red crater that involves only the surface skin. A foot ulcer also can be very deep. A deep foot ulcer may be a crater that extends through the full thickness of the skin. It may involve tendons, bones and other deep structures.
People with diabetes and people with poor circulation are more likely to develop foot ulcers. It can be difficult to heal a foot ulcer. In people with these conditions, even a small foot ulcer can become infected if it does not heal quickly.
If an infection occurs in an ulcer and is not treated right away, it can develop into:
- An abscess
- A spreading infection of the skin and underlying fat
- A bone infection
- Gangrene. Gangrene is an area of dead, darkened body tissue caused by poor blood flow.
Among people with diabetes, most severe foot infections that ultimately require some part of the toe, foot or lower leg to be amputated start as a foot ulcer.
Foot ulcers are especially common in people who have one or more of the following health problems:
- Peripheral neuropathy. This is nerve damage in the feet or lower legs. Diabetes is the most common cause of peripheral neuropathy. When nerves in the feet are damaged, they can no longer warn about pain or discomfort. When this happens, tight-fitting shoes can trigger a foot ulcer by rubbing on a part of the foot that has become numb.
In addition to diabetes, other medical conditions that increase the risk of foot ulcers include:
Which Ointment Is Best For Diabetic Wound
Hydrogen peroxide is used for very small wounds, but it’s more important to prevent infection when treating diabetic wounds. For a closed incision or wound, you would want to cover the entire surface of the skin with dry non-stick dressing and secure it with adhesive tape.
For an open wound or ulcer, it’s important to cleanse using soap and water as well as to irrigate your wound twice per day in order to maintain a sanitary environment. Wet dressings may be recommended after cleaning which may include sterile gauze/adhesive tapes applied so that the material can absorb any fluids from the surrounding area.
Newer products such as hydrocolloid dressings which are able to create a moist healing environment on surfaces by absorbing wound fluid while protecting the area from infection, dirt, and other external contaminants are available over-the-counter at pharmacies or grocery stores.
If you have a non-healing ulcer after six months of treatment, consult your doctor for further help in promoting wound healing. They may prescribe antibiotics to prevent infections.
Here is a list of supplies required when treating sores on diabetics:
- Hydrogen peroxide
- Non-adherent dressings
- Wet non-adherent dressing
- Cotton balls or cotton swabs
- Gauze pads: regular and compression
- Gauze roll bandages/tubular gauzes
- Tape
- Scissors
Here are some ways you can avoid getting cuts or sores on your feet.
Also Check: How To Heal Leg Ulcers Quickly
Understanding How The Oxygen Study Was Conducted
To be included in the study, patients had to be diagnosed diabetes and have a non-healing, full-thickness foot wound. These individuals had to meet the standard classification, known as the University of Texas Classification grade 1 or 2 diabetic foot ulcer, measuring more than 0.39 of an inch but less than 7.8 inches after surgical removal of unhealthy tissue .2 On average, patients were in their 60th decade of life.
These patients had had food ulcers for as little as a month and lasting up to one year, and they had been receiving the standard care during this time. According to the American Podiatric Medical Association, several factors are key in the typical management of foot ulcers, such as preventing infection, taking pressure off the area , removing dead skin and tissue , topical medications or dressings, as well as assuring that patient is under care for blood glucose management and related health issues.1
After three months of treatment, 15 of the wounds that were present at the beginning of the study were completely healed in the group getting active oxygen therapy but only 5 wounds, or 13.5%, in the group receiving no treatment .
Put another way, those receiving the pure oxygen were 4.5 times more likely to have their foot ulcer heal. After the researchers took into account the severity of the ulcers, the patients on the oxygen showed even greater improvement6 times more likely to completely healover the 12 weeks.
Management Of Systemic And Local Factors
Treatment of diabetic foot ulcers requires management of a number of systemic and local factors.
Precise diabetic control is, of course, vital, not only in achieving resolution of the current wound, but also in minimizing the risk of recurrence. Management of contributing systemic factors, such as hypertension, hyperlipidemia, atherosclerotic heart disease, obesity, or renal insufficiency, is crucial. Management of arterial insufficiency, treatment of infection with appropriate antibiotics, offloading the area of the ulcer, and wound care are also essential.
References
Amin N, Doupis J. Diabetic foot disease: From the evaluation of the foot at risk to the novel diabetic ulcer treatment modalities. World J Diabetes. 2016 Apr 10. 7 :153-64. . .
Naves CC. The Diabetic Foot: A Historical Overview and Gaps in Current Treatment. Adv Wound Care . 2016 May 1. 5 :191-197. . .
Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for Medicare and private insurers. Diabetes Care. 2014. 37 :651-8. .
Gentile AT, Berman SS, Reinke KR, Demas CP, Ihnat DH, Hughes JD, et al. A regional pedal ischemia scoring system for decision analysis in patients with heel ulceration. Am J Surg. 1998 Aug. 176:109-14. .
Mills JL Sr, Conte MS, Armstrong DG, et al. The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: risk stratification based on wound, ischemia, and foot infection . J Vasc Surg. 2014 Jan. 59 :220-34.e1-2. . .
You May Like: Can Ulcerative Colitis Cause Blood In Urine
Q: Is Podiatrist Toenail Trimming Covered By Insurance
Yes, this service may be covered for people with help issues that cannot help themselves. If your foot is in pain or has a health issue, a podiatrist is recommended to evaluate you, and this is a covered option.
If you have foot pain, please call our office and schedule a no-obligation consultation with our podiatrists to assess your eligibility for foot care.
What Is A Total Contact Cast
The total contact cast is a specific casting technique that is used to heal diabetic foot ulcers and to protect the foot during the early vulnerable phases of Charcot fracture dislocations. The cast is used to heal diabetic foot ulcers by distributing weight along the entire plantar aspect of the foot. It is applied in such a way to intimately contact the exact contour of the foot hence the name, “total contact cast.”
The cast relieves the pressure on the prominent areas of the foot, permitting the ulcers to heal. The cast should applied in such a way that the patient can remain mobile during the treatment of the ulcer. The cast is molded to the contours of the foot from the back of the heel through the arch region, in the region of the metatarsals, around the metatarsals, and even to the toes. The pressure, which has been concentrated on the bony prominence, is now distributed over the entire sole of the foot.
For the Charcot foot, the total contact cast is used in two ways. In the initial treatment of the Charcot foot when the breakdown is occurring and the foot is quite swollen and reactive, the cast is applied to control the movement of the foot and support its contours. In this instance the patient is often asked not to bear weight on the foot. In the second instance when the foot has already become deformed and ulceration has occurred, the principle using the cast is the same as described for the foot that has become deformed due to paralysis of the small muscles.
Read Also: Do Enemas Help Ulcerative Colitis
Identifying Symptoms And Diagnosis
One of the first signs of a foot ulcer is drainage from your foot that might stain your socks or leak out in your shoe. Unusual swelling, irritation, redness, and odors from one or both feet are also common early symptoms.
The most visible sign of a serious foot ulcer is black tissue surrounding the ulcer. This forms because of an absence of healthy blood flow to the area around the ulcer.
Partial or complete gangrene, which refers to tissue death due to infections, can appear around the ulcer. In this case, odorous discharge, pain, and numbness can occur.
Signs of foot ulcers are not always obvious. Sometimes, you wont even show symptoms of ulcers until the ulcer has become infected.
Talk with your doctor if you begin to see any skin discoloration, especially tissue that has turned black, or feel any pain around an area that appears callused or irritated.
Your doctor will likely identify the seriousness of your ulcer on a scale of 0 to 5 using the Wagner Ulcer Classification System:
- 0: no open lesions may have healed lesion
- 1: superficial ulcer without penetration to deeper layers
- 2: deeper ulcer, reaching tendon, bone, or joint capsule
- 3: deeper tissues involved, with abscess, osteomyelitis, or tendonitis
- 4: gangrene in a portion of forefoot or heel
- 5: extensive gangrenous involvement of the entire foot
Ulcers in people with diabetes are most commonly caused by:
- poor circulation
- nerve damage
- irritated or wounded feet
Infection of a foot ulcer can be prevented with:
Diabetic Foot Ulcer Symptoms
Normally a wound or sore on the skin would cause pain. But the same loss of feeling in the feet that often contributes to the development of a diabetic foot ulcer means that theres often no pain associated with the ulcer. This can make it difficult for people to realize that an ulcer is even there in the early stages, when treatment is most effective.
Aside from pain, another sign to look for is discharge or drainage from the wound in the socks. Ulcers that have been present for some time and that have become infected may also cause an unpleasant odor.
You May Like: Can You Get An Ulcer In Your Intestines
Treatment Of Diabetic Foot Ulcers
Once an ulcer has developed, the cause should be ascertained. Is it neuropathic, vascular, or both? A neuropathic ulcer must be protected from further injury until it heals. Strenuous efforts must be made to prevent another ulcer from forming by wearing the appropriate footwear.
A vascular or ischaemic ulcer should be evaluated by an Interventional Radiologist / Endovascular surgeon. He will determine the extent of damage and whether surgery is necessary. In extreme cases, this could mean partial amputation of a toe, foot, or limb. The Interventional Radiologist / Endovascular surgeon will also take an X-ray to determine whether the patient suffers from osteomyelitis followed by an Arterial doppler scan to evaluate the status of the arteries
The primary goal of treating a diabetic foot ulcer is to obtain healing as quickly as possible to prevent the ulcer from becoming infected. There are several key factors in the treatment of a diabetic foot ulcer. Some of them are:
- Prevention of infection
- Removing pressure from the area, called offloading
- Removing dead skin and tissue, called debridement
- Managing blood glucose and other health problems
- Applying medications and dressings to the ulcer
For more information about Diabetic Foot Ulcers, as well as the treatment for DVT, Varicose veins or other vascular conditions, contact Dr. Abhilash Sandhyala at 9989649498 or 9959033037, or at contact@drabhilash.com or visit our website at www.drabhilash.com
How To Prevent Diabetic Ulcers

For those who are diabetic or who have experienced ulcers in the past, there are some ways to prevent foot ulcers. If a foot wound has occurred due to a diabetic ulcer, there is a risk that it may return.
You May Like: Yea Sacc For Horses With Ulcers
Q: When Should I Call A Podiatrist For An Appointment
A: Pain is never normal, especially if it has been going on for longer than one week. This means that most insurance plans will cover a visit if you feel you have a problem developing with your feet.
The longer you wait, the more serious the pain may become, which can lead to hospitalization or further foot problems.
It would help if you had it evaluated and treated to avoid long-term problems.
How Is Diabetes Linked To My Feet
You probably know that diabetes develops when your blood glucose level, or blood sugar, is too high. With Type 1 diabetes, your body cant produce enough insulin. With Type 2 diabetes, on the other hand, your body doesnt use the insulin it does produce correctly.
Whether you have Type 1 or 2 diabetes, youre at greater risk of having elevated blood sugar levels. And when your blood sugar remains elevated, it damages nerve tissues creating a condition called peripheral neuropathy.
Peripheral neuropathy, also sometimes called diabetic neuropathy, creates numbness and loss of sensitivity in the lower extremities and feet. If you cant feel cuts, blisters, or sores on your feet, there a greater risk of bacteria entering the wound and creating an infection.
Don’t Miss: Can Ulcerative Colitis Cause Cancer
Evaluation And Treatment Of Diabetic Foot Ulcers
Diabetic foot problems, such as ulcerations, infections, andgangrene, are the most common cause of hospitalization among diabeticpatients. Routine ulcer care, treatment of infections, amputations, andhospitalizations cost billions of dollars every year and place a tremendousburden on the health care system.
The average cost of healing a single ulcer is $8,000, that of an infectedulcer is $17,000, and that of a major amputation is $45,000. More than 80,000amputations are performed each year on diabetic patients in the United States,and 50% of the people with amputations will develop ulcerations andinfections in the contralateral limb within 18 months. An alarming 58% willhave a contralateral amputation 3-5 years after the first amputation. Inaddition, the 3-year mortality after a first amputation has been estimated ashigh as 20-50%, and these numbers have not changed much in the past 30 years,despite huge advances in the medical and surgical treatment of patients withdiabetes.
How Does Hbot Help Your Diabetic Wounds Heal
Oxygen can only make its way through the blood within red blood cells. Since the circulation problems associated with diabetes slow the movement of red blood cells, important tissues become deprived of oxygen.
Without enough oxygen, cells struggle to produce the energy they need to block bacteria, synthesize new collagen, or regenerate and repair after injury. This is why diabetic wound healing slows until it comes to a full stop. Inhaling the concentrated flow of oxygen provided through regular HBOT treatments makes it possible to overcome oxygen deficiencies and stimulate a more effective healing process.
Overall, HBOT helps your diabetic wounds heal faster. It recruits white blood cells by providing the oxygen they need to effectively kill bacteria, reduce swelling, and allow the rapid reproduction of new blood vessels. When you commit to weekly treatments in an ongoing protocol, HBOT revitalizes the bodys healing process and renews tissues you thought may never recover.
You May Like: How Do You Heal Leg Ulcers