Is Ulcerative Colitis Curable
Currently, theres no nonsurgical cure for UC. Treatments for the inflammatory disease aim to extend periods of remission and make flare-ups less severe.
For people with severe UC, curative surgery is a treatment option. Removing the entire large intestine will end the symptoms of UC.
This procedure requires your doctor to create a pouch on the outside of your body where waste can empty. This pouch can become inflamed and cause side effects.
For that reason, some people choose to have only a partial colectomy. In this surgery, your doctor only removes the parts of the colon that are affected by UC.
While these surgeries can help ease or end symptoms of UC, they can have adverse effects and possible long-term complications. Read more about these issues to determine if surgery is an option for you.
What Is The Most Important Information I Should Know About Humira
You should discuss the potential benefits and risks of HUMIRA with your doctor. HUMIRA is a TNF blocker medicine that can lower the ability of your immune system to fight infections. You should not start taking HUMIRA if you have any kind of infection unless your doctor says it is okay.
- Serious infections have happened in people taking HUMIRA. These serious infections include tuberculosis and infections caused by viruses, fungi, or bacteria that have spread throughout the body. Some people have died from these infections. Your doctor should test you for TB before starting HUMIRA, and check you closely for signs and symptoms of TB during treatment with HUMIRA, even if your TB test was negative. If your doctor feels you are at risk, you may be treated with medicine for TB.
- Cancer. For children and adults taking TNF blockers, including HUMIRA, the chance of getting lymphoma or other cancers may increase. There have been cases of unusual cancers in children, teenagers, and young adults using TNF blockers. Some people have developed a rare type of cancer called hepatosplenic T-cell lymphoma. This type of cancer often results in death. If using TNF blockers including HUMIRA, your chance of getting two types of skin cancer may increase. These types are generally not life-threatening if treated tell your doctor if you have a bump or open sore that doesnt heal.
What Should I Tell My Doctor Before Starting Humira
Tell your doctor about all of your health conditions, including if you:
- Have an infection, are being treated for infection, or have symptoms of an infection
- Get a lot of infections or infections that keep coming back
- Have TB or have been in close contact with someone with TB, or were born in, lived in, or traveled where there is more risk for getting TB
- Live or have lived in an area where there is an increased risk for getting certain kinds of fungal infections, such as histoplasmosis, coccidioidomycosis, or blastomycosis. These infections may happen or become more severe if you use HUMIRA. Ask your doctor if you are unsure if you have lived in these areas
- Have or have had hepatitis B
- Are scheduled for major surgery
- Have or have had cancer
- Have numbness or tingling or a nervous system disease such as multiple sclerosis or Guillain-Barré syndrome
- Have or had heart failure
- Have recently received or are scheduled to receive a vaccine. HUMIRA patients may receive vaccines, except for live vaccines. Children should be brought up to date on all vaccines before starting HUMIRA
- Are allergic to rubber, latex, or any HUMIRA ingredients
- Are pregnant, planning to become pregnant, breastfeeding, or planning to breastfeed
- Have a baby and you were using HUMIRA during your pregnancy. Tell your babys doctor before your baby receives any vaccines
Recommended Reading: Is Pepcid Good For Ulcers
Ulcerative Colitis Questions To Ask Your Doctor
Whether youâre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
Living With Ulcerative Colitis
With careful management, most people with UC are able to enjoy life, including work, travel, recreation, sex and having children.
To keep healthy, consider:
- eating a nutritious diet to help with healing and reduce fatigue
- keeping a food diary to check if there are any foods that make your symptoms worse during a flare-up
- asking your doctor about supplements if you think you may be malnourished
- exercising regularly to lift your mood and help relieve stress
- learning some relaxation techniques to help manage stress
Recommended Reading: How To Help Ulcerative Colitis Flare Up
Pearls And Other Issues
There is an increased risk of colorectal cancer in patients with ulcerative colitis. The risk is cumulative, with a 2% chance of colorectal cancer after ten years of diagnosis, 8% after 20 years, and 20% to 30% after 30 years. Two factors associated with increased risk of colorectal cancer are the duration and extent of the disease.
How Can You Use This Information
You dont need to become an expert in the tools your doctor uses to determine the severity of your condition. However, it is helpful to understand how this information is used.
Determining severity helps your doctor know how to best treat your IBD. Following changes in severity over time helps you and your doctor know if treatments are working.
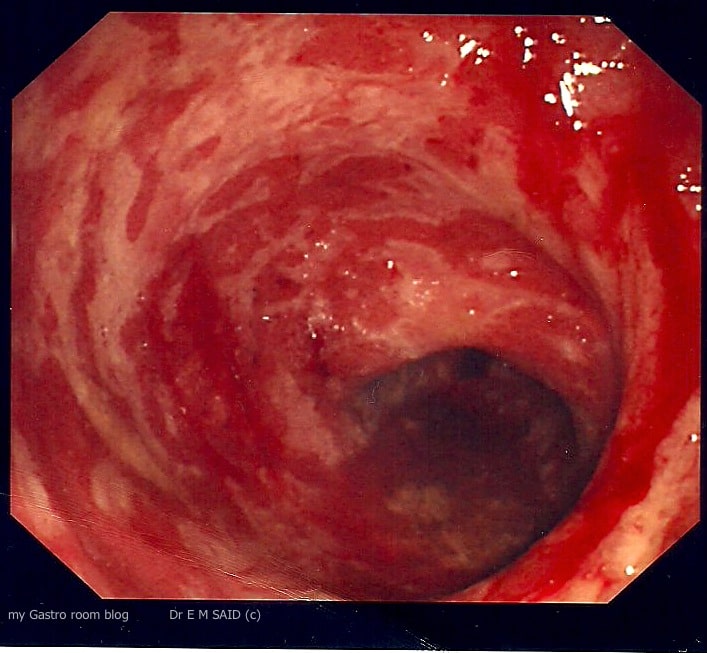
There are two separate goals of treatment: improving your symptoms and healing your bowels. While the two usually go hand in hand, your health care provider may see improvement in your bowels before you experience an improvement of your symptoms, or vice versa. If youre not seeing improvement in symptoms or in your bowels, it may be time to discuss different treatment options.
It is important to discuss your treatment goals with your doctor, so you can work together to meet those goals.
Dont Miss: I Think I Have Ulcerative Colitis
You May Like: How Do I Treat Mouth Ulcers
How Are Ulcerative Colitis And Colitis Different
A key difference is what triggers colitis. For instance, IBD is usually an autoimmune issue. Thatâs when your immune system attacks healthy tissue in your body. Other kinds of colitis can be the result of outside factors, such as germs or medical treatments.
People with UC or other kinds of IBD may also have inflammatory symptoms alongside bowel problems, including:
But those arenât the only distinctions. Hereâs a breakdown by colitis type:
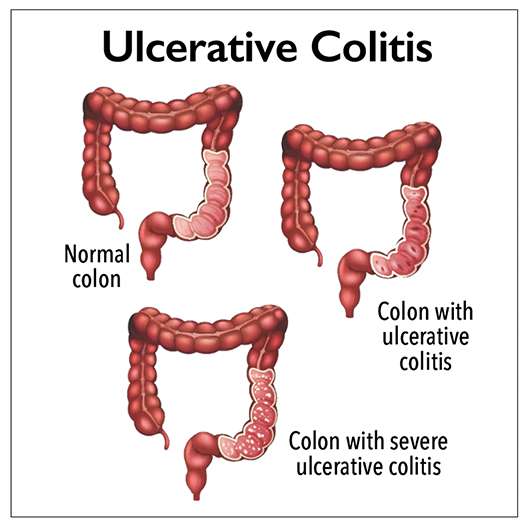
Ulcerative colitis . This type of IBD causes sores and constant inflammation in the inner lining of your large intestine. UC often starts in the rectum and extends through the left side of your colon. But some people have colitis throughout most or all of their colon. Thatâs called extensive colitis or pancolitis.
Crohnâs colitis. This is a feature of Crohnâs disease, another type of IBD. Crohnâs can impact any part of your gastrointestinal tract â thatâs your mouth to your . Unlike UC, you may have healthy tissue in between spots of inflammation. Crohnâs disease can also affect many layers of your GI tract.
Microscopic colitis. This is another type of IBD. Itâs not related to ulcerative colitis or Crohnâs disease, but itâs associated with other autoimmune diseases. Like the name suggests, your doctor has to use a microscope to see any evidence of this kind of colitis.
There are two main forms:
Some experts think collagenous and lymphocytic colitis may be different phases of the same condition.
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove some or all of your bowel may be an option.
During surgery, your small intestine can be diverted out of an opening in your abdomen known as a stoma. This type of surgery is known as an ileostomy.
In some cases, the stoma is only temporary and can be closed up once your bowel has healed.
Recommended Reading: How To Treat Rodent Ulcers In Cats At Home
Ulcerative Colitis Risk Factors & Comprehensive Care
University Hospitals inflammatory bowel specialists have significant experience in ulcerative colitis diagnostics, management and treatment. Ulcerative colitis is identified when swelling and inflammation occur in the lining of your large intestine and your rectum. It is part of a group of diseases called inflammatory bowel disease .
Ulcerative Colitis can range in severity and complexity some individuals have mild UC while others have a more serious and complex disease. Because every patient is treated with an individualized plan, our gastrointestinal, or GI specialists provide personalized care, depending on their disease severity.
Whats The Difference Between Ulcerative Colitis And Crohns Disease
UC and Crohns disease are the most common forms of IBD. Both conditions are thought to be the result of an overactive immune system.
They also share many symptoms, including:
However, UC and Crohns disease do have distinct differences. Understanding the key differences between them can help you obtain a proper diagnosis.
Location
These two conditions affect different portions of the GI tract.
Response to treatment
Similar medications are prescribed to treat both conditions. Surgery is also a treatment option. Its a last resort for both conditions, but it can be a cure for UC, whereas its only a temporary therapy for Crohns.
Read Also: Hind Gut Ulcers In Horses Treatment
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Favorite Orgs For Essential Uc Info
CCF is the leading nonprofit organization dedicated to finding the cure for UC and Crohns. The organization is at the forefront of IBD research and works to educate, empower, and support individuals afflicted with these diseases. Find your local chapter by visiting the CCF website.
This research institute at Virginia Mason in Seattle is one of the few establishments devoted to finding the causes of autoimmune diseases like UC and their cures. Benaroya has already helped advance research in more than 80 diseases of the immune system. The autoimmune life blog provides information on community events and personal stories from patients living with an autoimmune disease.
You May Like: Can Ulcerative Colitis Cause Weight Gain
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or poo sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be urgently admitted to hospital for immediate care.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
What Are The Medication Options For Ulcerative Colitis
There are a few types of drugs used to treat ulcerative colitis.
Aminosalicylates are typically the first kind of drug prescribed for ulcerative colitis. They work by reducing inflammation directly in your digestive tract and can be taken on an ongoing basis.
Corticosteroids, also known simply as steroids, are used to treat disease flares. Most drugs of this type work by suppressing the entire immune system, so they can have severe side effects and shouldnt be taken for long periods.
Biologics are made of antibodies that are grown in the lab and work by stopping certain proteins in the body from causing inflammation.
Small molecules are oral medications that also work on the immune system but act differently from biologics.
These drugs are used to treat moderate to severe ulcerative colitis.
Immunomodulators are a second-line drug for treating ulcerative colitis. These drugs limit inflammation at its source in the immune system.
Other drugs for ulcerative colitis may include antibiotics and certain pain relievers.
Don’t Miss: Liver Disease Associated With Ulcerative Colitis
What Should I Watch For After Starting Humira
HUMIRA can cause serious side effects, including:
Common side effects of HUMIRA include injection site reactions , upper respiratory infections , headaches, rash, and nausea. These are not all of the possible side effects with HUMIRA. Tell your doctor if you have any side effect that bothers you or that does not go away.
Favorite Ulcerative Colitis Blogger
Sam Cleasby created her blog in 2013 to raise awareness of IBD and her struggles with self-esteem. Cleasby also has a radio show on BBC Radio Sheffield in which she shares about modern family life, including relationships, disability, nutrition, and kids. You can subscribe to her blog via email or follow her on or .
Recommended Reading: Where To Buy Cabbage Juice For Ulcers
How Are Ulcerative Colitis And Crohn’s Disease Similar
- Both diseases often develop in teenagers and young adults although the disease can occur at any age
- Ulcerative colitis and Crohn’s disease affect men and women equally
- The symptoms of ulcerative colitis and Crohn’s disease are very similar
-
The causes of both UC and Crohn’s disease are not known and both diseases have similar types of contributing factors such as environmental, genetic and an inappropriate response by the body’s immune system
Follow Up With Your Doctor
You may only need at-home or short-term care for some kinds of colitis. But UC is a condition youâll have for the rest of your life. And it affects everyone in a different way. Youâll need to work with your doctor to find a treatment plan that works for you.
No matter whatâs causing your symptoms, get medical care right away if you have:
- Watery diarrhea for more than a few days
- Heavy, ongoing diarrhea
Recommended Reading: Photos Of Venous Leg Ulcers
When To See A Doctor
People who live with any form of ulcerative colitis should have a close relationship with a gastroenterologist .
Other specialists, such as a colorectal surgeon, may also be part of the medical team. A gastroenterologist will help monitor your condition and offer you an understanding of the probabilities of relapse.
There are some symptoms, however, for which it is crucial to see a doctor sooner. These include:
What Is The Best Diet For Ulcerative Colitis

Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Don’t Miss: What Type Of Disease Is Ulcerative Colitis
How Do You Get Diagnosed With Ulcerative Colitis
Common tests used in patients with UC are:
- Colonoscopy: this is the test used most commonly to make the initial diagnosis of UC and later for ongoing monitoring of disease severity.
- Routine blood tests: detect infection, anemia, inflammation and vitamin deficiencies.
- Fecal blood test: detects blood in your stool and bleeding in the intestines.
- Other stool tests: detect infection and monitor disease severity.
- Computerized tomography : shows different images of the bowels and surrounding tissue.
Read Also: Treating Hindgut Ulcers In Horses
Differences Between Ulcerative Colitis And Crohn’s Disease
The differences between ulcerative colitis and Crohn’s disease are:
- In Crohn’s disease, there are healthy parts of the intestine mixed in between inflamed areas. Ulcerative colitis, on the other hand, is continuous inflammation of the colon
- Ulcerative colitis only affects the inner most lining of the colon while Crohn’s disease can occur in all the layers of the bowel walls
Read Also: Is Pineapple Good For Ulcerative Colitis
Cyclosporine For Refractory Acute Severe Uc
Patients with fulminant UC who have not responded to high-dose IV steroids for 57 days may respond to IV cyclosporine.,, IV cyclosporine has been demonstrated to induce response or remission in 6482% of patients ,, however, up to 50% of patients ultimately undergo a colectomy. Because long-term cyclosporine is not effective for maintenance of remission, bridge therapy to 6-MP or azathioprine is necessary. Concurrent use of 6-MP or azathioprine as a bridge therapy with cyclosporine may decrease the release rate in those individuals who initially respond to cyclosporine to as low as 10%. Potential side effects associated with cyclosporine include severe, opportunistic infections , nephrotoxicity, hypertension, seizures, peripheral neuropathy, and anaphylaxis.,,
Role Of Rectal Therapy
When considering the various treatment modalities for UC, it is important to recognize that the rectum requires separate treatment. Patients receiving a biologic agent or mesalamine may require a second agent to address rectal symptoms such as tenesmus, urgency, or worsening continence. Although such rectal symptoms may qualify as mild to moderate by standard definitions, they are often considered severe by patients living with the condition. For example, incontinence can be embarrassing and difficult to manage.
The decision to use rectally administered therapy is guided by the proximal extent of disease and by patient preference. There are clear advantages to rectal delivery over oral therapy in some circumstances. It has long been recognized that left-sided disease and extensive disease have improved responses when topical therapy is added to the existing oral mesalamine regimen., Topical mesalamine has been advocated as preferable to oral therapy in patients with proctitis/proctosigmoiditis and left-sided UC because it provides sufficient concentrations of active drug at the inflamed site. Moreover, systemic absorption is considerably low given that the therapeutic efficacy of mesalamine is topical in nature. Other advantages include a generally faster response and a less frequent dosing regimen.
You May Like: Causes Of Bleeding Ulcers In Stomach
You May Like: How To Prevent Ulcerative Colitis