What Procedures And Tests Diagnose Crohn’s Disease And Ulcerative Colitis
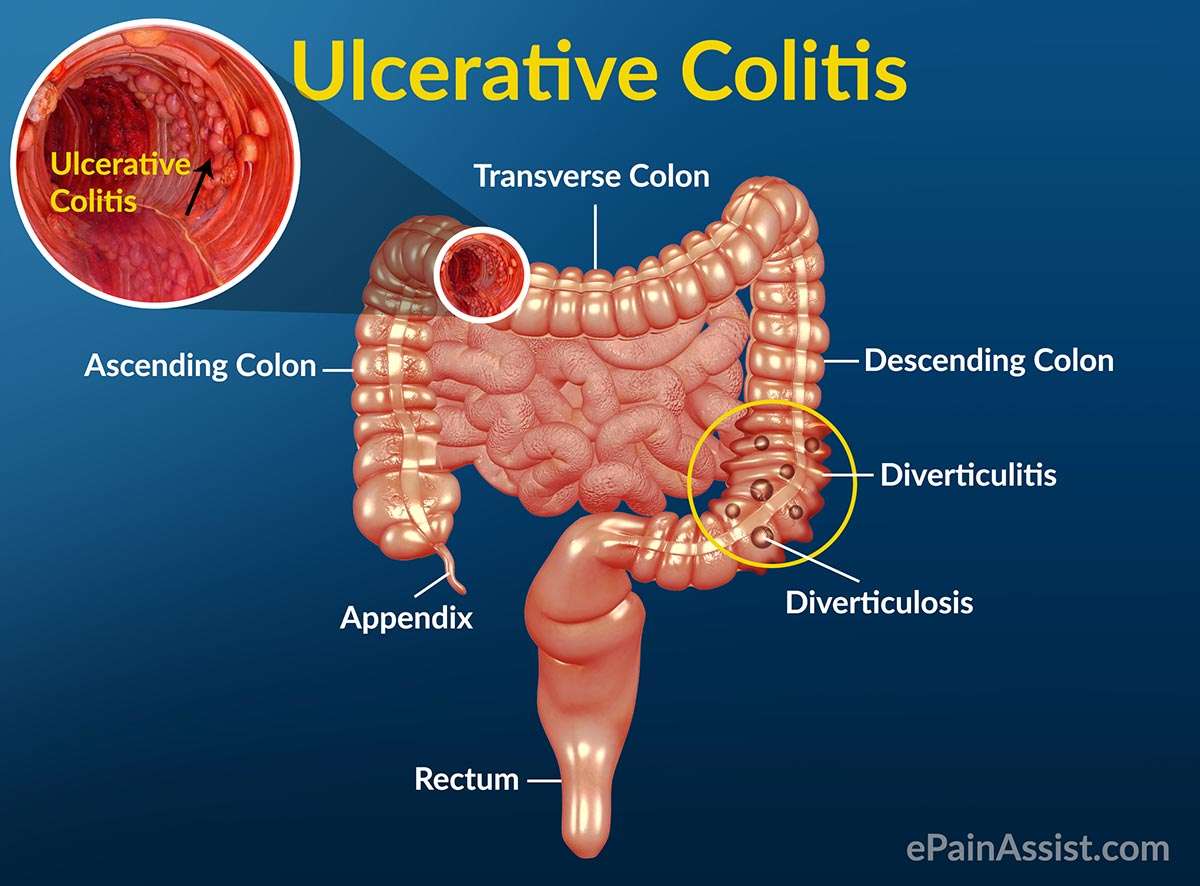
Doctors diagnose ulcerative colitis by endoscopy . During this procedure the doctor can see and take pictures of the patients abnormal gut mucosa , and the presence of continuous disease . Other blood tests and imaging tests like CT scan or MRI are used, but these tests are not definitive.
Doctors use the same procedures and tests to diagnose Crohns disease. However, they also use small bowel studies, colonoscopy, and upper GI endoscopy to identify the abnormal gut mucosa that usually occur in multiple areas anywhere in the intestinal tract. These areas are not continuous, but are separated by normal areas of intestinal mucosa that distinguish them from ulcerative colitis lesions.
As with Crohns disease, nutrition is important if you have ulcerative colitis because symptoms of diarrhea and bleeding can lead to dehydration, electrolyte imbalance, and loss of nutrients. It may be necessary to take nutritional supplements if your symptoms do not allow you to eat a nutritionally balanced diet. Talk to your health-care professional about what supplements to take.
Which Signs And Symptoms Of Ibd Vs Ibs Are Different
Signs and symptoms unique to inflammatory bowel disease include:
- Diarrhea that may be bloody
Stress can affect both conditions. In inflammatory bowel disease, stress can cause flare-ups of Crohns disease and ulcerative colitis. Stress may cause gastrointestinal symptoms of IBS to worsen, so you may be more aware of them. Stress also can trigger symptoms because of how they can affect your daily life.
About Irritable Bowel Syndrome
IBS is fairly common, with anywhere from 25-45 million Americans suffering from it. The basic cause isnt understood, but you suffer symptoms because your colon muscle contracts more readily than normal. Triggers for IBS include certain foods, stress, hormones, or other illnesses.
Symptoms of IBS may involve:
- Excess gas
- Harder or looser bowel movements than normal
- Pain or cramps in the abdomen, usually in the lower half
- Diarrhea, constipation, or alternating between the two
Rectal bleeding and black stool is not a symptom of IBS. You should seek immediate evaluation at our office if you experience possible blood in your stool.
Rest assured that IBS does not raise your risk of developing other serious issues of the digestive system, including colitis, Crohns disease, or cancer.
You May Like: Drugs To Treat Ulcerative Colitis
Complications Caused By Nutritional Deficiencies
Some of the complications of malnutrition include:
- Dehydration diarrhoea causes your body to lose fluid, which can lead to dehydration. Severe dehydration can damage your kidneys.
- Anaemia reduced iron in the diet combined with losing blood from the bowel can lead to anaemia .
- Weight loss reduced appetite and poor absorption of food nutrients can cause weight loss.
- Reduced growth inadequate nutrition during childhood and adolescence can impair a childs growth and physical development.
What Causes Ulcerative Colitis Vs Crohns Disease
Its not entirely known what causes ulcerative colitis or Crohns disease. However, experts believe it has something to do with genetic factors and environmental factors . Your gut microbiomethe bazillion bacteria that live in your digestive tractis thought to have influence as well. In fact, a 2020 study published in the journal Frontiers of Medicine, found that not only was the gut bacteria in people with IBD different from people without IBD, but it was also different between people with ulcerative colitis vs. people with Crohns disease.4
What is known is that something sets off your immune system to mistakenly attack healthy areas of your digestive tract, causing chronic inflammation.
This overreaction of the immune system can also affect areas outside of your digestive system and can include your skin, eyes, and other organs. This can occur with both ulcerative colitis and Crohns disease, but ulcerative colitis is more likely to affect the skin, eyes, and bones, while Crohns disease is more apt to affect the kidneys and gallstones.1
Read Also: What Is Good For Ulcers
Please Stop Apologizing To Me Because I Cant Eat
Im often asked what is the most difficult thing about having intestinal failure and being on TPN. Most people assume its not being able to eat and others assume that it must be the adjustments you have to make to your daily life. I have to agree that yes, those things are very difficult and Ive been angry and sad and everywhere in between about it. Some days are better than others.
But to me the most difficult thing about being on TPN is
Getting To A Diagnosis
Theres no doubt that IBD can significantly decrease quality of life, between uncomfortable symptoms and frequent bathroom visits. IBD can even lead to scar tissue and increase the risk of colon cancer.
If you experience any unusual symptoms, its important to call your doctor. You may be referred to a gastroenterologist for IBD testing, such as a colonoscopy, sigmoidoscopy, or a CT scan. Your doctor may also order blood and fecal testing. Diagnosing the specific form of IBD will lead to more effective therapies.
Commitment to daily treatment and lifestyle changes can help minimize symptoms, achieve remission, and avoid complications.
Regardless of your diagnosis, Healthlines free app, IBD Healthline, can connect you with people who understand. Meet others living with Crohns and ulcerative colitis through one-on-one messaging and live group discussions. Plus, youll have expert-approved information on managing IBD at your fingertips. Download the app for iPhone or Android.
Read Also: How To Know If You Have A Peptic Ulcer
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Overlap Between Ibd And Ibs
Although the two disorders have traditionally been seen as distinct in terms of both presentation and cause, some researchers are putting forth theories that perhaps the two diagnoses of IBS and IBD are actually at different ends of the same spectrum.
Some studies have shown that people who have IBS are at higher risk of eventually being diagnosed with IBD . One group of researchers found that this higher risk may be associated with having experienced infectious gastroenteritis .
-
Symptoms: pain plus constipation and/or diarrhea
-
Rarely leads to serious complications, surgery, or death
-
Symptoms: pain, diarrhea, bloody stool, fever, weight loss
-
Can lead to bowel perforation, infection, surgery, cancer, and death
You May Like: How Can I Get Rid Of Mouth Ulcers
Recommended Reading: Bleeding Ulcer Treatment At Home
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Also Check: Can Diverticulitis Cause Ulcerative Colitis
Is There A Difference Between Ulcerative Colitis And Colitis
Colitisthetheulcerative colitis
. Similarly, you may ask, is colitis and ulcerative colitis the same thing?
There are two: Crohn’s disease and ulcerative colitis. By the way, if you hear some people just say colitis, that’s not the same thing. It means inflammation of the colon. With ulcerative colitis, you have sores in the lining of your colon, as well as inflammation there.
Furthermore, which is worse Crohn’s disease or ulcerative colitis? Although both Crohn’s disease and ulcerative colitis are chronic diseases, UC may be considered worse, as people with extensive and severe UC may require surgery. People over age 50 that need surgery have increased mortality due to colitis-associated postoperative complications.
Keeping this in consideration, what is the main cause of colitis?
Colitis is a chronic digestive disease characterized by inflammation of the inner lining of the colon. Infection, loss of blood supply in the colon, Inflammatory Bowel Disease and invasion of the colon wall with collagen or lymphocytic white blood cells are all possible causes of an inflamed colon.
What does stool look like with colitis?
Symptoms of ulcerative colitis vary from person to person. But because this disease affects the colon and rectum, bowel problems such as bloody stools or diarrhea are a primary symptom. bloody stools that may be bright red, pink, or tarry. urgent bowel movements.
What Is The Difference Between Collagenous Colitis And Lymphocytic Colitis
Microscopic colitis is an inflammatory bowel disease that usually starts in the colon or rectum, although it is not the same condition as Crohns disease or ulcerative colitis. It gets its name from the fact that inflammation can only be seen under a microscope during an endoscopy.
There are two forms of microscopic colitis: collagenous colitis and lymphocytic colitis. Although the two forms share many similarities under the umbrella of microscopic colitis, there are a few key differences.
Recommended Reading: Symptoms Of Stomach Ulcers In Horses
What Are The Risk Factors Of Ulcerative Colitis
It is estimated that as many as one million Americans have IBD with that number evenly split between Crohns disease and ulcerative colitis. Males and females appear to be affected equally. The usual age of diagnosis with ulcerative colitis is in the mid-30s, although the disease can occur at any age. Men are more likely than women to be diagnosed with ulcerative colitis in their 50s and 60s. The incidence is greater in whites than non-whites, and a higher incidence is found in Jews than in non-Jews.
IBD tends to run in families. Studies have shown that up to 20 percent of patients with ulcerative colitis will have a close relative with either Crohns disease or ulcerative colitis. There is no way to predict which, if any, family members will develop ulcerative colitis.
Read Also: What Medicine Is Best For Stomach Ulcers
Diagnosing Colitis And Chronic Ulcerative Colitis
Your gastroenterologist may suspect colitis based on your medical history and a review of your symptoms. He or she will have you undergo a colonoscopy procedure using a colonoscope to view the colon and rectum, and may take a tissue sample to help determine the cause. Other tests and procedures include:
- BLOOD TESTSBlood tests are taken to determine both red and white blood cell counts. A low red blood cell count can indicate anemia, from bleeding within the colon and rectum. Elevated white blood cells, which fight infection, indicate inflammation within the colon and rectum.
- STOOL SAMPLEA stool sample may be taken to rule out a parasitic infection that can cause colitis.
- CT SCANIn addition to a colonoscopy, a CT scan can determine what areas of the rectum and colon are inflamed.
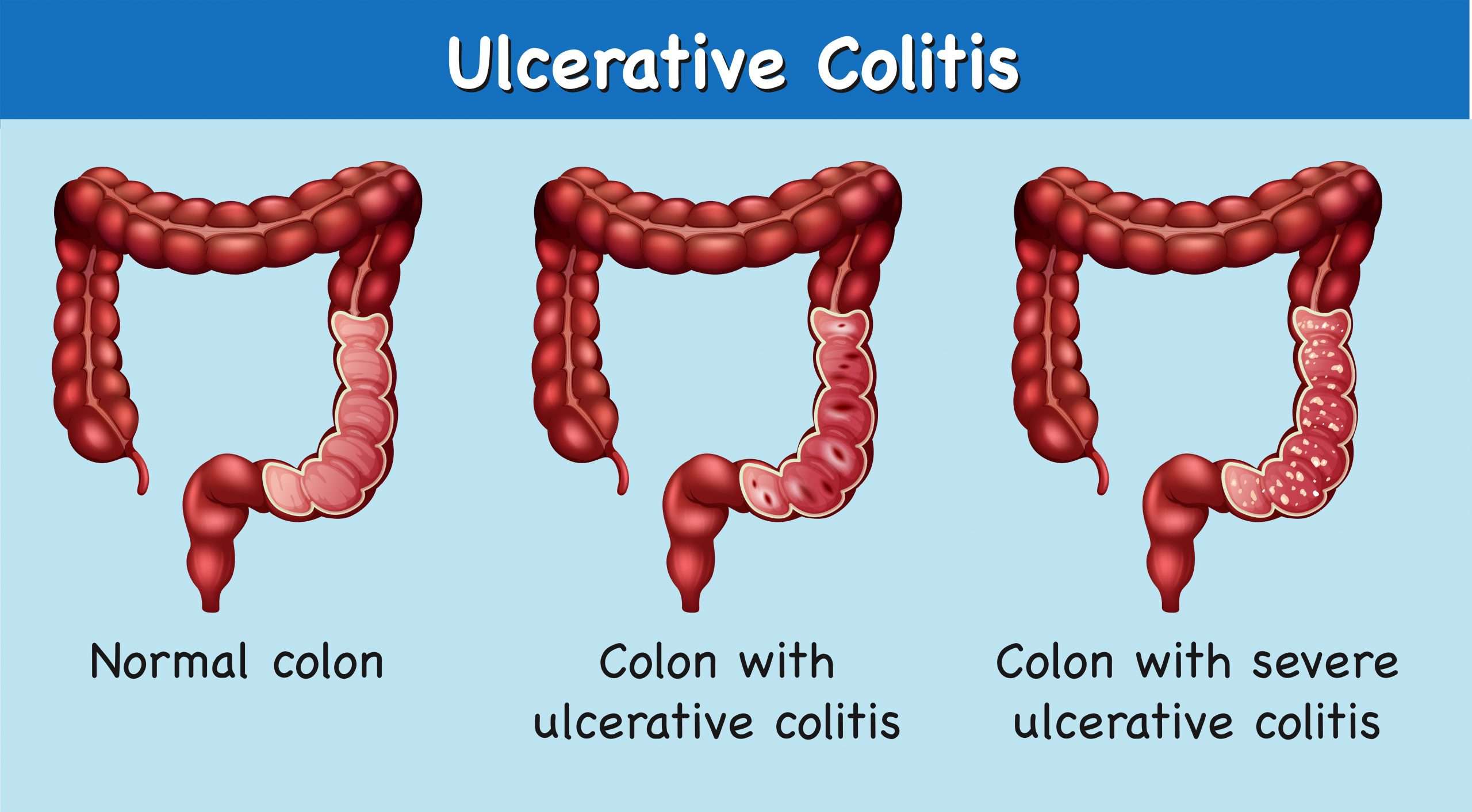
Classification of chronic ulcerative colitis
Gastroenterologists categorize chronic ulcerative colitis based on the location and extent of inflammation within the colon and rectum. For most patients, the affected area remains the same during the course of the disease.
Read Also: How To Diagnose Bleeding Ulcer
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
What Is Microscopic Colitis
Ulcerative colitis and Crohns disease involving the colon are two well-known types of inflammatory bowel disease however there are additional types of colitismicroscopic colitis and ischemic colitiseach with its own symptoms and treatment requirements.
About microscopic colitis | Diagnosis ||
Microscopic colitis, which includes collagenous colitis and lymphocytic colitis, is characterized by chronic watery diarrhea caused by inflammation in the colon. It is not related to ulcerative colitis or to Crohn’s disease, and there is no evidence to suggest that microscopic colitis carries the same increased risk for colon cancer as ulcerative colitis.
This condition is known as “microscopic” colitis because physicians usually can’t see the inflammation without a microscope. When looked at through an endoscopea camera mounted at the end of a long, flexible tube that’s inserted in the rectumeither during a colonoscopy or sigmoidoscopy, the colon appears entirely normal.
Read Also: Can I Eat Oatmeal With Ulcerative Colitis
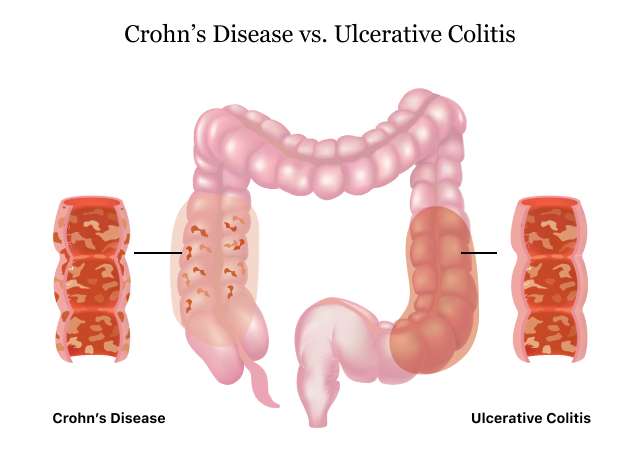
Symptomatic Differences Between Crohns Disease And Ulcerative Colitis
There are some subtle differences in symptoms of Crohns disease and ulcerative colitis. In Crohns disease rectal bleeding is less common, whereas in ulcerative colitis, bleeding from the rectum is much more common. In Crohns disease, continuous abdominal pain is more common and perianal problems such as fistulas, anal sores and skin tags, can occur. In contrast, people living with ulcerative colitis usually have intermittent pain coinciding with bowel movements. Perianal issues are uncommon in ulcerative colitis.
Clinical Trials Updates
Crohns Disease And Ulcerative Colitis Overview
Crohns disease and ulcerative colitis are the two most common forms of inflammatory bowel disease . Crohns disease and ulcerative colitis can be treated, but there is no cure. UC and Crohns are separate diseases, but they both involve chronic inflammation of the digestive tract. People with IBD may have long periods of good health known as remission and periods of active symptoms known as relapses or flares. Symptoms vary among people with Crohns disease and ulcerative colitis, but most experience abdominal pain and cramping, diarrhea, nausea, vomiting, and fatigue.
Crohns disease and ulcerative colitis are not fatal, and on average, people with IBD have similar lifespans as people without either condition.
Both Crohns disease and ulcerative colitis are immune-mediated diseases, meaning the bodys immune response does not work as it should. In IBD, the immune system has an abnormal response, causing chronic inflammation and damage in the gastrointestinal tract. Read more about the causesof IBD.
You May Like: How Do You Heal Leg Ulcers
Vitamin And Mineral Supplements For Ibd
A person with IBD who eats a healthy, varied diet does not usually need to take vitamin supplements. But if they have a dietary deficiency, they may need tablets or occasional vitamin B12 injections. For example, a person on a low-fibre diet may need extra vitamin C and folic acid because they dont eat enough fruit and vegetables.A person with Crohns disease who experiences steatorrhoea may need calcium and magnesium supplements. Most children with IBD should take supplements to help them grow and develop normally.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Recommended Reading: Will An Ulcer Cause Diarrhea