What Is The Prognosis For A Person With Colitis
Patients with infectious diarrhea tend to get better relatively quickly with supportive care. Most infections will resolve with or without specific treatment and often do not require antibiotics. Those decisions depend on the patients diagnosis.
Patients with inflammatory bowel disease probably will require lifelong treatment to help control their symptoms. The goal, as with any long-term illness, is to allow the patient to live a normal life with minimal symptoms from the disease.
Patients with ischemic colitis need to minimize their risk factors for progressive narrowing of the arteries. These are the same risks as for heart disease and require the same treatment approach, including controlling high blood pressure, diabetes, high cholesterol, and smoking cessation. Patients with severe ischemia that leads to a dead colon require surgery to remove the gangrenous segment.
Also Check: Zinc Oxide For Stage 2 Pressure Ulcer
How Do You Calm A Colitis Flare Up
Read Also: What To Use For Stomach Ulcer
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
You May Like: Is Alcohol Bad For Ulcerative Colitis
You May Like: How To Help Ulcerative Colitis
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Inclusion Criteria And Exclusion Criteria
All IBD patients included in the study had biopsy-proven CD or UC. IBD patients were eligible to be included in the study if the clinician who saw them at the time of inclusion determined that they currently had inactive disease. The status of disease for IBD patients was then confirmed using IBD clinical indices: CDAI < 150 or UCAI < 4 for inactive disease. Patients were excluded from the study if they reported active disease in the 3 months prior to the enrollment. Patients were also excluded from the trial if they were on biologic medications for maintenance, as the periodic dosing of these medications could be a confounder in this 1-week trial. All participants included in the study had been on a stable dose of their IBD medications for at least 3 months and were not taking NSAIDs for at least 4 weeks prior to beginning the study. Patients were included as healthy controls if they had no established diagnosis of GI disease and were required to complete a questionnaire marking no on a list of common GI diseases and symptoms. Finally, subjects with any history of alcohol or drug abuse, either IBD patients or controls, were excluded from participation in the trial.
Also Check: What Makes An Ulcer Worse
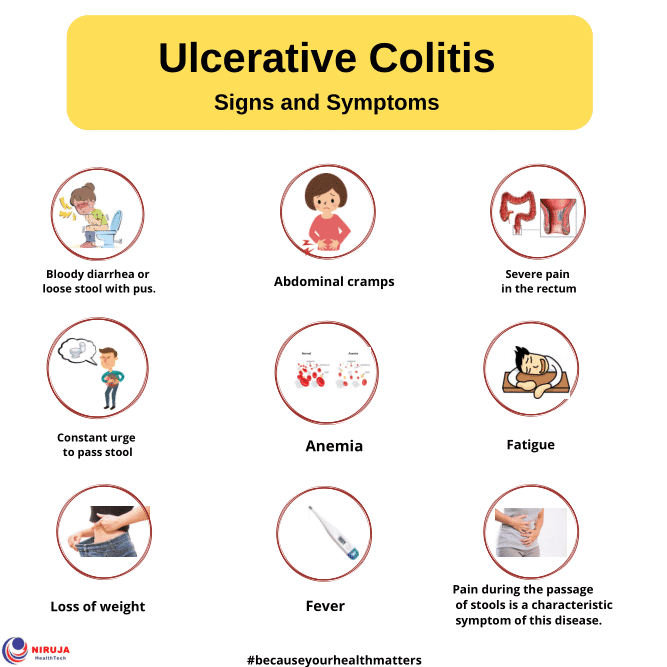
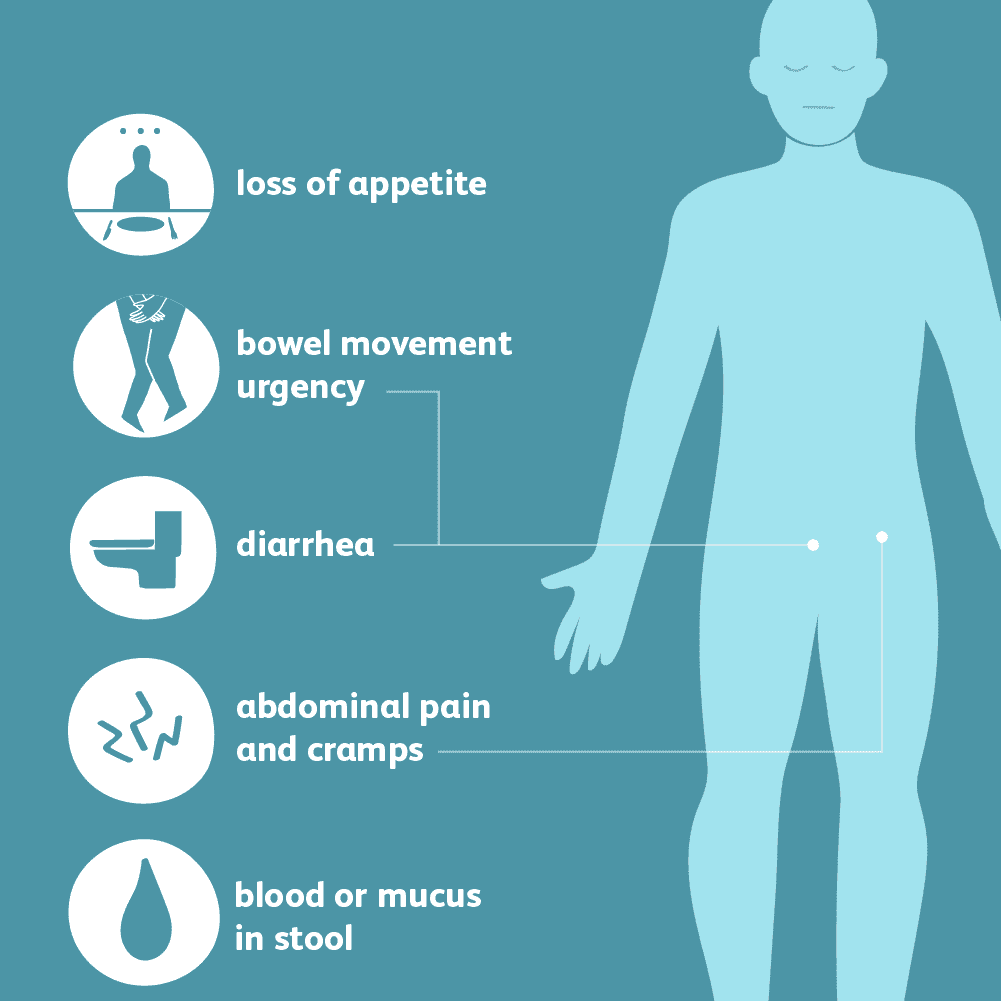
Symptoms Of Ulcerative Colitis
The exact symptoms that people will experience will depend on where the inflammation occurs but can involve:
* Rectal bleed* Anemia is a lack of healthy red blood cells and it is caused by rectal bleeding.* An urgent need to defecate* Rectal pain* Loss of fluids and nutrients from the body.* Children with UC may fail to develop normally* Skin lesions* Rectal Tenesmus means that the individual feels unable to empty their bowels when they are defecating.* Abdominal cramps* Feeling tired all the time
Those individuals who have fulminant colitis can experience:
* Extreme abdominal pain* Excessive bleeding from the anus* Severe diarrhea
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohns disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
Also Check: How To Treat Stomach Ulcers Naturally
Work With Your Doctor To Understand Uc Severity
Its important for you and your doctor to understand how severe your symptoms are. Beyond that, tests and procedures may be done to evaluate your disease activity and get an even better understanding of whats really happening inside your bodyand the inflammation thats occurringgetting you to the treatment plan thats right for you.
What Is The Correlation Between Caffeine And Colitis
Generally speaking, some individuals with UC, such as you, may choose to limit their intake of caffeine due to causing or worsening of IBD symptoms. Others, on the other hand, may even choose to avoid it all together due to unwanted side effects.
For instance, say you were to accidentally fall down on an uneven pavement and scratch your elbow. This part of your body is now agitated and inflamed. With time, the scratch will begin to heal, as long as you take good care of it. Now say that you were to fall down again a few days later, on the exact same elbow at the exact same spot of your injury. Naturally, you will feel a lot of pain. In the case of ulcerative colitis or Crohns disease, this is the same effect that caffeine can have on the body. The lower gastrointestinal tract is already injured or rather irritated. So by frequently drinking caffeine, you continuously irritate the large intestine. By simply making a few dietary changes such as eliminating caffeine, you can help alleviate your symptoms.
If, however, you are concerned about triggering symptoms of UC, then consult with your doctor about whether skipping coffee altogether or finding a satisfying alternative is right for you. In any case, making necessary dietary changes can do wonders for your health in terms of easing your symptoms and preventing recurrence.
Recommended Reading: How Severe Is Ulcerative Colitis
Ibds And Alcohol: What To Drink And What Not To Drink
People think that if you have an Inflammatory Bowel Disease like Crohns Disease or Ulcerative Colitis that you shouldnt take a sip of alcohol. In a perfect world that might be the case. In reality, most of our social interactions revolve around some form of drinking. Not having a drink isnt always an option.
I get it, you want to have fun with your friends, feel like you fit in, and there is nothing wrong with that. Im writing this article because like you Im a human being. I enjoy having a drink and I want you to be able to do the same. Pretending that someone with an IBD will never have a drink is completely naive!
The key is learning what you can do to minimize or eliminate negative side effects.
Symptom No : Abdominal Cramps
Solution: Try to pinpoint your triggers. Stomach cramps are often caused by gas or spasms in the gut. Common culprits include foods high in fiber or fat, which can impact gas production, says , an assistant professor of medicine at the University of Minnesota Medical School in Minneapolis and director of their inflammatory bowel disease program. Foods that are high in insoluble fiber especially cruciferous vegetables, such as broccoli and cauliflower can be particularly hard to digest, according to the Crohns & Colitis Foundation.
Medications, such as a recent course of antibiotics or nonsteroidal anti-inflammatory medications ibuprofen, naproxen, aspirin can also trigger abdominal pain, he says.
Also Check: Can Alcohol Cause Stomach Ulcers
Recommended Reading: Azulfidine Dosage For Ulcerative Colitis
What Can You Do About Flare
Your situation will depend on your triggers and how your flare-ups present themselves. But first off, its crucial to listen to your docs advice and take any medication as prescribed. This can help reduce your symptoms and the risk of potentially serious complications.
To make those flare-ups feel less sh*tty, here are a few options you can try:
- taking over-the-counter pain relievers
- using a heated pad to reduce pain in your belly
- using antibacterial wet wipes on your butt to reduce your risk of infection and prevent irritation
- taking antidiarrheal meds to, well, put a pause on diarrhea
- using a medicinal mouthwash to manage sores
- using perianal cleaning products when you shower
- engaging in regular self-care, including exercising, getting enough sleep, and giving yourself time to de-stress
You May Like: What Happens In Ulcerative Colitis
Alcohol Vs Ulcerative Colitis Meds
Taking ulcerative colitis meds in sufficient quantities increases the risk of a heart failure. Additionally, people under the influence of ulcerative colitis meds and alcohol may have difficulty forming new memories. With alcohol vs ulcerative colitis meds in an individuals system they become confused and do not understand their environment. Due to the synergistic properties of ulcerative colitis meds when mixed with alcohol it can lead to confusion, anxiety, depression and other mental disorders. Chronic use of ulcerative colitis meds and alcohol can lead to permanent changes in the brain. Stopping Alcohol Consumption can cause alcohol withdrawals while stopping ulcerative colitis meds can also cause withdrawals.
Also Check: Ulcerative Proctitis Vs Ulcerative Colitis
Also Check: Can Ulcerative Colitis Cause Weight Gain
My Experience Of Drinking Alcohol With Ulcerative Colitis
Given that I suffer from migraines as well as IBD, alcohol always makes things worse for me. I stopped drinking any kind of alcohol when I was about 24. When I was younger, on the nights I would drink with my friends, I stuck to clear liquids . I found them to affect my ostomy and intestines the least.
The heavy, regular beer never sat well with me. Basically, I kind of went by the rule the less alcohol in my system that will get me where I want to be, the better which is why I was never someone who sipped on cocktails and really enjoyed the flavor. Thinking back, I probably would have had better luck if I did the latter but, we all live and learn.
Youre Ignoring How Stressed You Really Are
Drs. Bloomfeld and Yun agree: When asked, people with UC often report experiencing stress before a flare. A study published in March 2019 in the Journal of Crohns and Colitis followed 417 people with IBD, which includes UC, and found that experiencing a stressful life event or new stressors in the previous three months was commonly linked to a flare-up.
Stress can trigger inflammation in the gut, worsening the symptoms of UC, according to a study published in 2019 in Frontiers in Pediatrics. Plus, stress can interfere with your usual routine, leading to poor sleep and medication and eating habits.
At Yuns clinic, a psychologist teaches relaxation exercises to people with UC. Learning techniques such as meditation or yoga may help you manage stress.
Recommended Reading: What Are The Symptoms Of Gastric Ulcer
Interactions With Other Drugs And Medications
Several medications prescribed for gastrointestinal conditions may react unfavorably with alcoholic drinks. In addition, medications put a strain on the liver’s ability to rid the body of toxins, and alcohol can increase that straining. See the table below that lists drugs commonly used to treat IBD or related conditions and the possible effects when mixed with alcohol.
Which Drinks Are Safe For People With Crohns
If you drink one particular type of alcohol and it doesnt cause flare-ups, then guess what? That one is safe for you.
A study from 2007 that involved 32 people examined the effects of these bevvies:
Out of the above booze varieties, the vodka and beer caused abdominal pain in a significant number of peeps with Crohns. The authors attributed this to the higher sugar concentrations .
Ultimately, this study is pretty old, and a sample of 20 people is teeny-tiny. Another 2011 study looked at 21 participants with Crohns who drank wine during a remission period . The researchers found that wine could make folks guts leakier, which might feed into future flare-ups.
But two small studies are hardly an indicator that everyone with Crohns will react the same way. If your fave booze is causing GI problems, try switching to another. If you dont experience any symptoms after the switch, then that type of alcohol was the Crohns troublemaker.
And if the next type also triggers flare-ups, maybe the trigger is alcohol in general. Living with Crohns has a painful learning curve. But once you understand your bodys relationship with triggers, small lifestyle adjustments can help you stay in remission longer.
Read Also: How To Heal Peptic Ulcer
Risk Of Flares And Complications
The consumption of red wine, in particular, has been linked to long-term risks of IBD relapse and flare-ups in people with otherwise inactive symptoms. Why? Because red wine can contribute to leaky intestines in people with Crohns.
Chronic alcohol use may potentially lead to liver disease and GI tract damage. Alcohol can also cause other complications that may already be common in people with Crohns, including:
Is Caffeine Okay To Consume With Colitis
In the United States alone, more than 1 million individuals suffer from an inflammatory bowel disease such as ulcerative colitis and Crohns disease. Such diseases interfere with the bodys ability to absorb the nutrients it requires, thereby leading to deficiencies. If you are suffering from ulcerative colitis , then you are already familiar with symptoms such as stomach pain, ongoing diarrhea, and bloody stools. While there is no known cure for UC, knowing what foods to eat and what beverages to drink can greatly affect your symptoms. Moreover, there are many effective treatments that can help keep the inflammation under control.
Due to the fact that UC is a type of inflammatory bowel disease, it is best to be aware of any trigger foods that could aggravate your gastrointestinal tract. With UC, you lose a lot of water through diarrhea. If you do not replace these lost fluids in your body, you are at risk of dehydration. However, it is not simply about drinking plenty of fluids, but rather drinking the right types of beverages. Water is a must, while beverages such as coffee, tea, and others containing caffeine act as diuretics, which lead to water loss.
Have a question about
Read Also: Medications To Treat Ulcerative Colitis
What You Can Do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if theres anything you need to do in advance, such as restrict your diet.
- Write down any symptoms youre experiencing, including any that may seem unrelated to the reason for which you made the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, including over-the-counter medications and any vitamins or supplements that youre taking.
- Take a family member or friend along. Sometimes it can be difficult to remember everything during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your provider.
Preparing a list of questions beforehand may help you make the most of your visit. List your questions from most important to least important in case time runs out. For inflammatory bowel disease, some basic questions to ask include:
- Whats causing these symptoms?
Common Medications Used To Treat Uc
The first course of action in treating UC is often amino salicylates. Also referred to as 5-ASAs, the NHS reports that these medications lower colon inflammation and allow your GI tract to heal. If 5-ASAs don’t improve your symptoms, the NHS recommends adding a short-term dose of corticosteroids. Medical professionals at The Crohn’s & Colitis Foundation explain that these drugs work by restraining your immune system. However, long-term use of corticosteroids can cause your body to reduce or stop making its cortisol, making it difficult for you to stop taking them without relapsing.
According to Healthline, many doctors turn to immunomodulators when 5-ASAs and corticosteroids fail to improve your situation. Also called immunosuppressants, these drugs target your body’s immune response and reduce inflammation. However, though studies show they’re effective, these drugs are prescribed off-label when given for the treatment of UC. Additionally, it can take several months for you to feel relief.
Medical professionals at The Crohn’s & Colitis Foundation state that the next step for those with symptoms that don’t respond to immunomodulators is to try biologics. Made out of organic material, these medications work by stopping the proteins responsible for inflammation. For those that other medications have failed or who need fast symptom relief, doctors prescribe Janus kinase inhibitors, which work by blocking inflammation signals given off by your immune system .
Also Check: Medication To Treat Stomach Ulcers