Take Some Deep Breaths To Calm Your Gut
Breathing deeply can help reduce UC gut pain and cramping, says Sara Kinsinger, PhD, director of behavioral medicine for the digestive health program at Loyola University Health System in Maywood, Illinois.
Deep breathing elicits a parasympathetic relaxation response that physiologically helps the body relax by increasing blood flow and oxygen to the gut, she says.
Experiment with different deep breathing techniques, including diaphragmatic breathing and alternate nostril breathing, to learn what helps you relax.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Ulcerative Colitis Questions To Ask Your Doctor
Whether youâre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
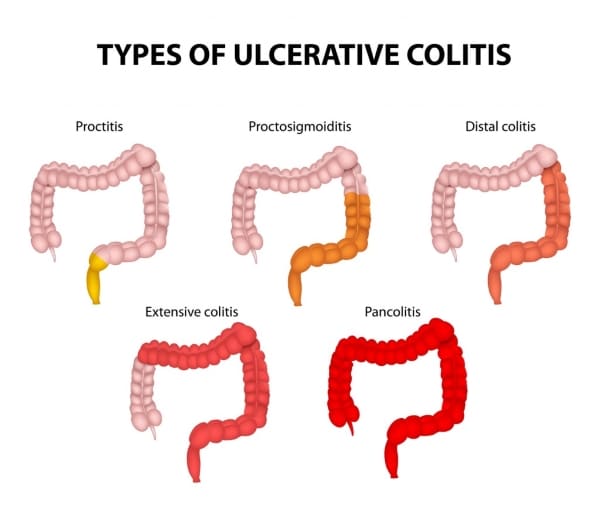
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
Recommended Reading: What Should You Not Eat If You Have An Ulcer
Also Check: Ulcerative Colitis How To Treat
How Crohns Disease Affects Your Body
What Is Crohns Disease? Crohns disease is an autoimmune disorder that affects ones entire gastrointestinal tract . Crohns disease can be quite chronic and because it is an inflammatory condition, it tends to lead to more severe problems and complications in the body. Crohns disease is a type of inflammatory
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
You May Like: Can You Cure Ulcerative Colitis Naturally
When Youre In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
Also Check: New Meds For Ulcerative Colitis
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you havent been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If youve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you cant contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
You May Like: Off Loading Shoe For Heel Ulcer
Prognosis For Ulcerative Colitis
Ulcerative colitis is usually chronic, with repeated flare-ups and remissions . In about 10% of people, an initial attack progresses rapidly and results in serious complications. Another 10% of people recover completely after a single attack. The remaining people have some degree of recurring disease.
People who have disease only in their rectum have the best prognosis. Severe complications are unlikely. However, in about 20 to 30% of people, the disease eventually spreads to the large intestine . In people who have proctitis that has not spread, surgery is rarely required, cancer rates are not increased, and life expectancy is normal.
Talk To People You Trust About What Youre Going Through
If you can feel yourself going into a flare-up, or youre already in one, talk to the people you love about whats happening. Tell them what youre going through and how your flare is affecting you.
Not only will it make you feel better to talk to someone about whats happening, but it also allows those closest to you to gain an understanding, which means theyll be able to offer help and support in the most appropriate way.
Tell them about your symptoms and what you need from the people you love, and be honest with them. Dont hold back. Your aim is to make it through this flare and to get back on track, and you need as much support as possible so tell them how they can best give that to you.
Tell them if youd find it helpful for them to call you to check up on you.
Tell them if youd just like them to listen and not to advise.
Tell them if support to you is simply understanding when youre not well enough to leave the house, and youd just prefer to sleep without being made to feel guilty.
Recommended Reading: How Do Ulcers Feel Like
Read Also: How To Calm Ulcerative Colitis Flare Up
Get Regular Exercise To Reduce Uc Inflammation
Snider says exercise is useful in managing many of the complications associated with ulcerative colitis, including decreased bone density, a weakened immune system, emotional health problems, stress, and weight gain.
Try to engage in a moderate-intensity exercise like swimming or biking, three or four days per week, he says. A review published in August 2016 in Pharmacological Reports noted that moderate exercise releases protective myokines such as irisin from working skeletal muscles, which promotes healing and helps with inflammatory bowel disease inflammation.
Snider also strongly recommends yoga as a natural treatment for ulcerative colitis, as it promotes relaxation and targets the digestive system, flooding the area with oxygen and nutrition for healing. Find what type and frequency of exercise works for you and take it slow: Too much exercise can cause mild systemic inflammation.
Research indicates that stress plays a role in inflammatory bowel diseases such as ulcerative colitis. Researchers analyzed data on 2,007 adults in a Swiss IBD study and found a relationship between depression and anxiety and disease symptoms. The results were published in June 2016 in Clinical Gastroenterology and Hepatology.
Counteract stress with relaxation techniques such as meditation, deep breathing, and progressive muscle relaxation to help your body relax.
Eat These Foods To Avoid A Flare Up Of Ulcerative Colitis
The Heal Your Gut Cookbook: Nutrient-Dense Recipes for Intestinal Health Using the GAPS Diet by Hilary Boynton contains more than 200 easy, straightforward recipes that restore the balance between beneficial and pathogenic intestinal bacteria. These recipes contains foods that are natural remedies for painful ulcerative colitis symptoms by sealing the gut through the elimination of grains, processed foods, and refined sugars.
Gut and Psychology Syndrome refers to disorders, including ADD/ADHD, autism, addictions, depression, and obsessive-compulsive disorder, stemming from or exacerbated by leaky gut and dysbiosis. GAPS also refers to chronic gut-related physical conditions, including celiac disease, rheumatoid arthritis, diabetes type one, and Crohns disease, as well as asthma, eczema, allergies, and thyroid disorders.
Read Also: How Do I Know If I Have A Peptic Ulcer
When To Call The Doctor
- Cramps or pain in your lower stomach area
- Bloody diarrhea, often with mucus or pus
- Diarrhea that cannot be controlled with diet changes and drugs
- Rectal bleeding, drainage, or sores
- Fever that lasts more than 2 or 3 days, or a fever higher than 100.4°F without an explanation
- Nausea and vomiting that lasts more than a day
- Skin sores or lesions that do not heal
- Joint pain that keeps you from doing your everyday activities
- A feeling of having little warning before you need to have a bowel movement
- A need to wake up from sleeping to have a bowel movement
- Failure to gain weight, a concern for a growing infant or child
- Side effects from any drugs prescribed for your condition
What Should I Eat During An Ulcerative Colitis Flare
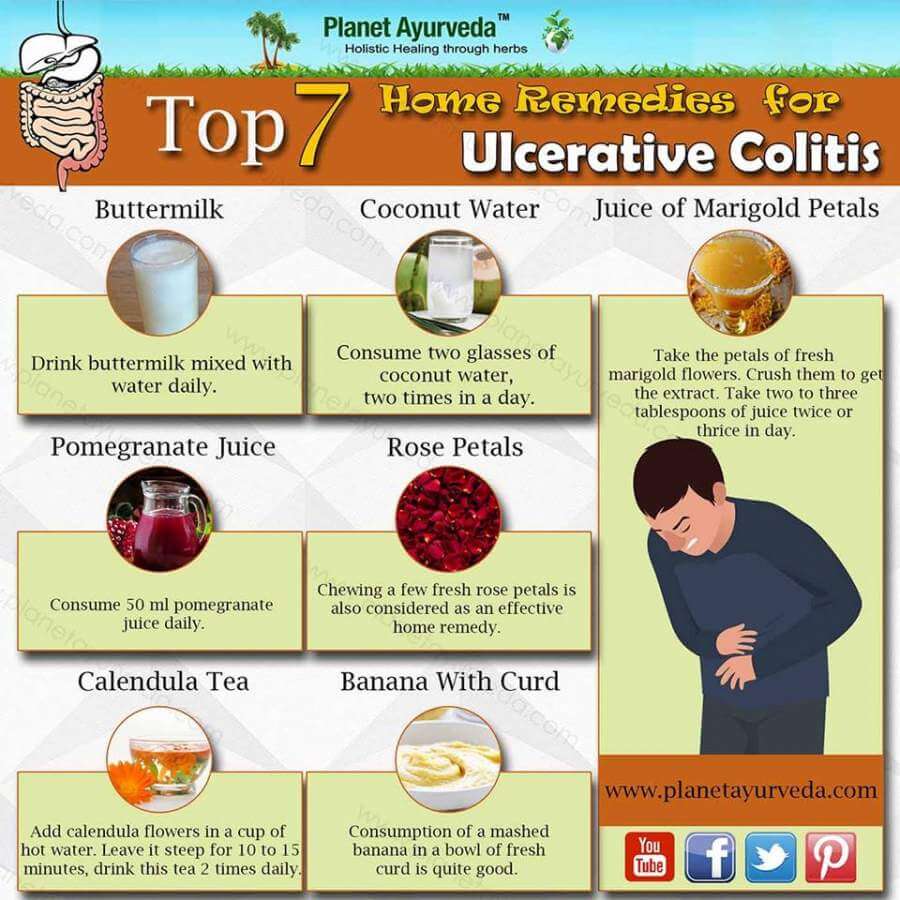
There is no specific type of diet that has been proven to relieve symptoms in people with ulcerative colitis. However, you may find that particular foods make symptoms worse.
It is important to identify and limit any foods that lead to worsening of your symptoms. Keeping a food journal may help you track how your diet relates to your symptoms.
Some suggestions that may help during a flare-up include:
- Reduce dairy products containing lactose
- Avoid high-fat foods
- What remedies help during an ulcerative colitis flare-up?
In addition to taking medication as prescribed and eating a well balanced diet, maintaining a healthy lifestyle can be beneficial for managing ulcerative colitis. Regular exercise and mindfulness strategies have been shown to improve overall health and quality of life.
Arastéh, K., Baenkler, H. W., Bieber, C., Brandt, R., & Chatterjee, T. T. . Duale Reihe Innere Medizin. Georg Thieme Verlag.
Dignass, A., PreiÃ, J. C., Aust, D. E., Autschbach, F., Ballauff, A., Barretton, G., â¦& Jantschek, G. . Aktualisierte Leitlinie zur Diagnostik und Therapie der Colitis ulcerosa 2011Ergebnisse einer Evidenzbasierten Konsensuskonferenz. Zeitschrift für Gastroenterologie, 49, 1276-1341.
Elizabeth Oliver, PhD
Recommended Reading: Best Mattress For Pressure Ulcers
Check Out Some Relatable Situations And How To Deal With Them
Everyday struggles can come with having ulcerative colitis like socializing or traveling. But the best way to navigate life with UC is to seek an effective treatment plan. Beyond that, its helpful to maintain a hopeful outlook, healthy lifestyle, and strong support networkand strive to lead a full life.
Easing Symptoms During A Flare
The below suggestions can also help ease symptoms or help keep your body healthy during a flare-up.
Drink water: In UC, the large intestine can have a hard time absorbing water and salt, which can contribute to diarrhea and dehydration. Drinking plenty of water or an electrolyte replacement drink can help avoid dehydration if youâre experiencing a flare.
Eat plain, easy-to-digest foods: During a UC flare, itâs common to lose your appetite. To keep your energy levels up and avoid malnutrition and weight loss, itâs important to continue to fuel your body with food. Unfortunately, fruits and vegetables, particularly when raw, are bothersome for many people with UC. Avoid fatty and greasy foods as well. Your doctor may also suggest meal replacement drinks if youâre losing weight from UC flare-ups.
Get some exercise: If youâre experiencing symptoms like stomach pain and diarrhea, exercise may sound like the last thing you want to do. But in addition to the well-known mood and health-boosting benefits of exercise, a workout can also have specific benefits for UC symptoms. Uncontrolled inflammation in the intestinal tract leads to UC symptoms. Exercise has an anti-inflammatory effect that can help these symptoms.
Read Also: Best Natural Remedies For Stomach Ulcers
Read Also: How Do You Know If You Have A Bleeding Ulcer
Managing Ulcerative Colitis Flares: The Most Important Step
The key to managing an ulcerative colitis flare is to get a confirmed diagnosis and begin treatment as soon as possible. But doing so can be tricky, because people with the condition may attribute their symptoms to other GI problems, says Oriana Mazorra Damas, MD, an assistant professor of gastroenterology at the University of Miami Miller School of Medicine in Miami.
The goal for remission is to feel well enough that you forget that you have the condition for most of the day in other words, you experience few, if any, symptoms, Dr. Damas explains.
Rapid Bowel Movements After Eating
The concern among participants that eating anything results in the need to have a bowel movement has also been supported during a flare.
I dont eat breakfast because I know within so many minutes of eating that I will need to go the bathroom.
When Ive got a flareup going, I mean, its always, I eat, and then half an hour later Im in the bathroom.
Recommended Reading: Are Mouth Ulcers A Sign Of Hiv
Also Check: What Are The Signs Of Having A Stomach Ulcer
Living With Ulcerative Colitis Symptoms
Your ulcerative colitis symptoms will likely come and go, with longer periods in between flares when you may not experience any discomfort at all. Those periods are called remission, and they can span months or even years. Because there is not yet a cure for ulcerative colitis, your symptoms will eventually return.
Ulcerative colitis is an unpredictable disease, and the length of periods of remission between flares can make it difficult for doctors to evaluate whether your course of treatment has been effective or not.
Passing Pus Or Mucus In Stool
People with UC may often pass mucus or pus in their stool, according to the National Library of Medicine. This can occur alongside diarrhea or bloody stool.
It is important to be aware of any changes in your stool. Contact a doctor if you frequently pass blood, mucus, or pus in your stool.
Find out more about UC stool symptoms.
Also Check: How Do You Say Ulcerative Colitis
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Foods To Eat During An Ulcerative Colitis Flare
Avoiding certain foods is only half the battle. Heres how to get the nutrients you need during an ulcerative colitis flare.
Jeff Wasserman/Stocksy
If you have ulcerative colitis, you may already know which foods worsen your flares. But figuring out what to include in your diet is equally important, because the right foods will provide you with key nutrients without aggravating your symptoms.
Most experts recommend that you limit your fiber intake when youre having an ulcerative colitis flare. A general rule is to replace high-fiber foods, such as nuts, seeds, and raw fruits and vegetables, with more easily digestible fare. Here are eight foods to eat during an ulcerative colitis flare and the reasons they can help.
1. Applesauce: Since your gastrointestinalsystem is experiencing a lot of irritation during a flare, you may want to stick to soft, easily digestible foods like applesauce. Be sure to choose an unsweetened variety though, because added sugar can cause more inflammation. You can also make your own sugar-free applesauce by cooking peeled, sliced apples with some water and then pureeing the mixture.
3. Cooked vegetables: Soft, cooked veggies like carrots and spinach can provide important nutrients, such as vitamins A and K. Just make sure the vegetablesare thoroughly cooked until they can be mashed with a fork, Szeles says so that any potentially irritating fiber is broken down.
Additional reporting by Nina Wasserman
Recommended Reading: What Is Best Medicine For Ulcer
What Is A Uc Flare
A UC flare is an acute worsening of the symptoms of bowel inflammation. Flares may occur weeks, months, or even years apart, with different levels of severity.
Medication, your lifestyle, diet, and other factors may contribute to flare-ups. In the same way, taking all prescribed medications, eating balanced meals, and avoiding known triggers can often help prevent flares.
Ulcerative colitis symptoms change based on the severity of a flare-up and the location of inflammation in the intestine. Symptoms often include:
- moderate to severe abdominal pain or cramps
- persistent bowel movements
Many Disease Activity Indices Exist For Ulcerative Colitis But None Have Been Developed With Formal Patient Input
There is no consensus gold standard for the evaluation of disease activity in ulcerative colitis. This is illustrated in numerous recent clinical trials, in which investigators measured several different indices of disease activity, as no one index is considered sufficient. There are many indices for the measurement of ulcerative colitis disease activity, including Truelove and Witts classification of mild, moderate, and severe disease the St Marks Index, which empirically added endoscopy in 1978 simplified versions of the St Marks Index, including the Ulcerative Colitis Disease Activity Index and the Mayo Score and noninvasive versions, including the Seo Index and the Simple Clinical Colitis Activity Index .
The diversity of indices suggests that none of these has proven satisfactory, and none was developed with patient input. In addition, it has never been established that any of these indices actually measures all of the important symptoms of ulcerative colitis.
Ulcerative colitis lacks a validated measurement instrument such as the Crohns Disease Activity Index in Crohns disease . Furthermore, the indices that do exist for ulcerative colitis were not constructed in a patient-centered manner to attempt to capture the symptoms experienced by patients. Therefore, our study group aimed to investigate through focus groups that what symptoms does patients with ulcerative colitis experience during their disease process.
Read Also: How To Ease Stomach Ulcer Pain
Don’t Miss: Foods To Avoid With Ulcerative Colitis