Favorite Ulcerative Colitis Blogger
Sam Cleasby created her blog in 2013 to raise awareness of IBD and her struggles with self-esteem. Cleasby also has a radio show on BBC Radio Sheffield where she shares about modern family life, including relationships, disability, nutrition, and kids. You can subscribe to her blog via email or follow her on or .
This book by A. Hillary Steinhart, MD, provides dietary strategies and recipes to help manage inflammatory bowel disease. The head of the combined division of gastroenterology for Mount Sinai Hospital and the University Health Network in Torontos Mount Sinai Hospital, Dr. Steinhart worked with the clinical dietitian Julie Cepo to offer well-researched dietary advice for people to maintain health during flare-ups as well as periods of remission. The book is packed with 150 recipes, from risotto to stew, to help anyone with IBD eat well and prevent malnutrition.
Doctors assured Danielle Walker that her diet was not a factor in her ulcerative colitis flares. But after years of suffering and multiple hospitalizations, Walker realized she needed to make dietary changes. At the two-year remission mark, the mom, wife, and self-trained chef began blogging about her experience and sharing recipes to help others struggling with IBD. You can buy Walkers cookbooks on her website, which is loaded with nutritional resources including a blog and videos.
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Other Complications Of Crohn’s Disease
There are also intestinal manifestations of Crohn’s disease that occur outside the intestines, some of which may be debilitating. These include arthritis, inflammation of the eye that can impair vision, skin diseases that vary from mild to severe , gallstones, and loss of bone due to nutritional deficiencies. Most of these complications are believed to be due to inflammation outside of the intestine.
You May Like: Do Stomach Ulcers Cause Nausea
Common Warning Signs Of Ulcers
Ulcers are a common medical issue that affects about one in ten people in America. They occur when acid in the digestive tract eats away at the inner surface of the esophagus, stomach or small intestine. The acid can create a painful open sore that may bleed. You can get them anywhere on your body for any reason, but the most common form of ulcers occur in your stomach.
Although there is no single cause for an ulcer, many factors can increase your risk of stomach ulcers including painkillers, excessive drinking of alcohol and smoking tobacco. Luckily, ulcers are easy to treat once you recognize the symptoms of them. Here are five common signs of a stomach ulcer:
Abdominal Pain: A burning sensation may occur in your stomach. The pain will come and go in waves and is often accompanied by bloating. Many may confuse this feeling with acid reflux or other similar diseases. If the abdominal pain starts after you eat, keeps you up at night, and lasts a prolonged period it might be an ulcer.
Nausea: Due to the imbalance in your digestive system, mild to severe nausea may occur, either first thing in the morning on an empty stomach, or after eating. Because of nausea that will occur, rapid weight loss also comes in conjunction with it as well.
Bloating: A feeling of heaviness and fullness can occur in the stomach, usually the same feeling you get after drinking a full glass of water.
Who Is At Risk For Colorectal Cancer
Every one of us is at risk for colorectal cancer. Although the exact cause for the development of precancerous colon polyps that lead to colorectal cancer is not known, there are some factors that increase a persons risk of developing colorectal polyps and cancer. These risk factors include:
- Age: The risk of developing colorectal polyps and cancer increases as we age. Colorectal cancer is more common in people over the age of 50, however, younger adults can also develop colorectal cancer.
- Other medical conditions: Medical conditions and inherited conditions can increase your chances of developing colorectal cancer.
- Lifestyle factors: You may be at increased risk for developing colorectal cancer if you drink alcohol, use tobacco, dont get enough exercise, and/or if you are overweight. Smoking increases the risk of precancerous polyps and colorectal cancer. A diet high in fat and calories and low in fiber, fruits and vegetables has been linked to a greater risk of developing colorectal cancer. Many lifestyle factors that increase the risk of colorectal cancer can be modified to lessen that risk.
Dont Miss: Bone Broth And Ulcerative Colitis
Don’t Miss: Can Ulcers Cause Heart Palpitations
What Chemotherapy Agents Are Used To Treat Colorectal Cancer
5-Fluorouracil, or 5-FU , has been the first-line chemotherapy drug, along with the vitamin leucovorin, for advanced colorectal cancers for many years. 5-FU is often given intravenously but is also available in an oral form as capecitabine .
Two other intravenous chemotherapy drugs irinotecan and oxaliplatin also are used for the treatment of advanced colorectal cancers. Oxaliplatin is given, along with 5-FU and leucovorin, for advanced colorectal cancers, while irinotecan is used alone or in combination with 5-FU/leucovorin for patients with metastatic colorectal cancer .
Newer treatments for metastatic colorectal cancer include monoclonal antibodies and immunotherapy.
Monoclonal antibodies are created in a lab to find and destroy a particular target in this case, colorectal cancer cells. Because of their precision, the idea is that treating a tumor with a monoclonal antibody will be more specific than chemotherapy drugs, and therefore have fewer side effects.
How To Reduce Your Risk
Here are a few other things you can do to lower your chances of developing colorectal cancer and improve your odds of finding it early if you develop it:
- Ask your doctor about taking medications such as sulfasalazine , vedolizumab , or mesalamine . These drugs help manage UC, and they may help lower your risk for colorectal cancer.
- Take your medications as your doctor prescribed to keep your UC inflammation well managed.
- See your gastroenterologist for check-ups at least once a year.
- Let your doctor know if any of your family members had colorectal cancer or have recently been diagnosed.
- Eat more fruits, vegetables, and whole grains such as brown rice or wheat bread.
- Limit red meat, such as burgers, steaks, and pork. Also limit processed meats, such as hot dogs, bacon, and sausage. Theyve been linked to colorectal cancer risk.
- Avoid alcohol or limit yourself to no more than one drink a day.
- Try to walk, ride a bike, or do other exercises on most days of the week.
Along with getting regular screenings, look for these symptoms of colorectal cancer and report them to your doctor right away:
- a change in your bowel movements
- blood in your stool
Also Check: What Do You Do If You Have An Ulcer
Black Or Dark Colored Stool
If you think you may have an ulcer, a good way to tell is to look at your stool. If you notice that when you use the restroom your stool is extremely dark in color, or even black, chances are you are right about what is ailing you. If this is the case, you should absolutely go to the hospital immediately.
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
You May Like: Best Treatment For Stomach Ulcers
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Outlook For People With Ulcerative Colitis
If you have UC, a doctor will need to monitor your condition, and youll need to carefully follow your treatment plan throughout your life.
The only true cure for UC is removal of the entire colon and rectum. Your doctor will usually begin with medical therapy unless you have a severe complication that requires surgery. Some people will eventually require surgery, but most do well with nonsurgical therapy and care.
Recommended Reading: Are Fermented Foods Good For Ulcerative Colitis
Symptoms Of Crohn’s Disease
The most common symptoms of Crohn’s disease are abdominal pain and diarrhea. Other signs of inflammation are often present, including fever and abdominal tenderness. Because symptoms can be worsened by eating, the intake of food is reduced, and this leads to loss of weight, and, less commonly, nutritional deficiencies. Slow, continuous loss of blood into the intestine that may not even be recognizable in the stool can lead to iron deficiency anemia.
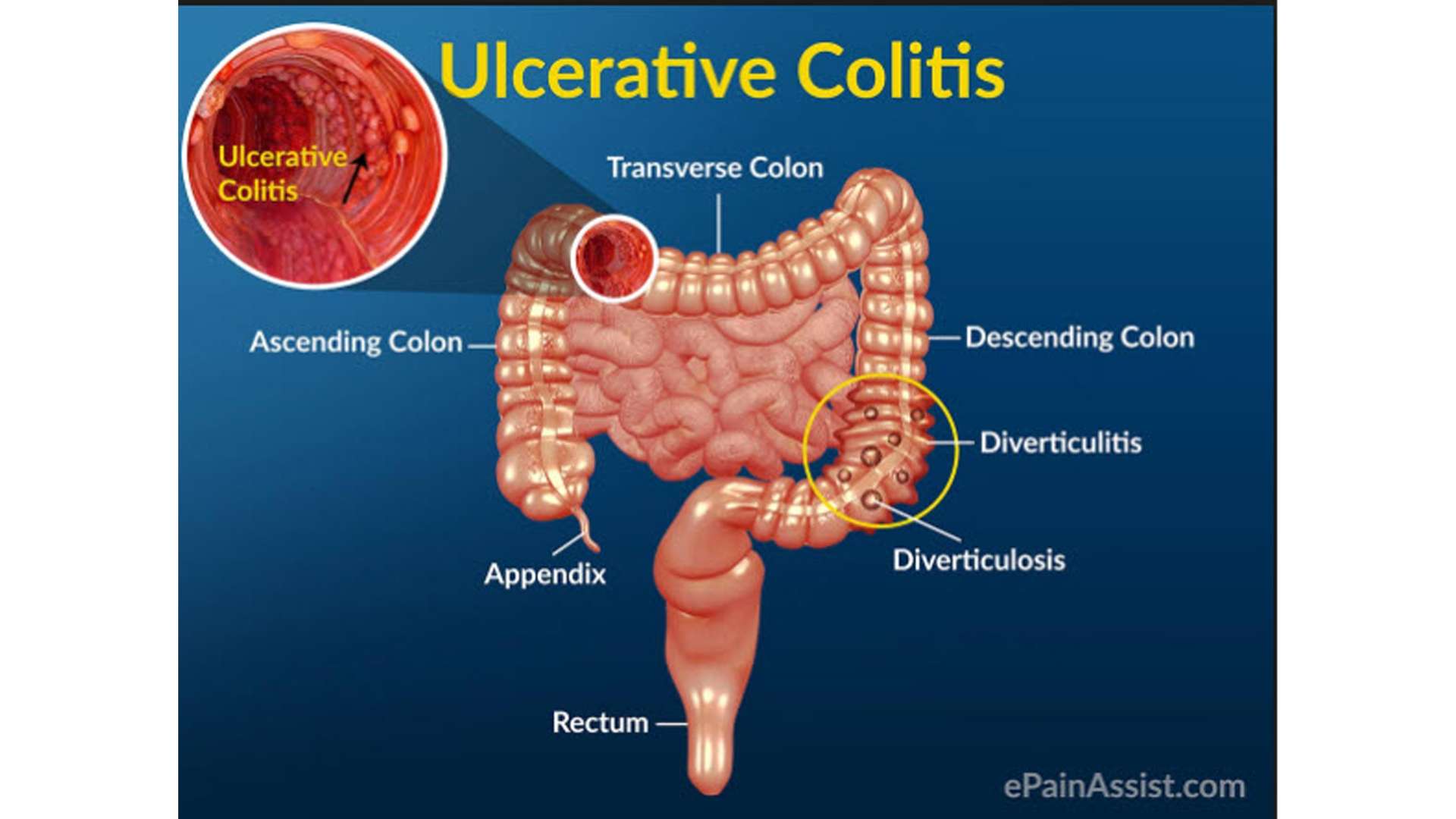
What Are The Causes And Risk Factors Of Ulcerative Colitis
Ulcerative colitis is believed to be caused by an abnormal response by your bodys immune system.
Your immune system is supposed to defend you against harmful invasive bacteria and viruses. But in some people, the immune system mistakenly attacks the bodys own tissue.
In ulcerative colitis, this may happen when the body mistakes food and helpful bacteria for harmful substances. It may also come about when the body doesn’t turn off its response to fighting an infection.
Experts believe that ulcerative colitis develops because of a combination of environmental factors and genetic predisposition.
Frontiers in ImmunologyFrontiers in Immunology
Fatty cold-water fish such as mackerel, tuna, salmon, sardines, and herring are rich sources of omega-3 fatty acids.
Editor’s Picks
Recommended Reading: Best Probiotic For Ulcerative Colitis
Diet Progression Following Flares For Ulcerative Colitis And Crohns Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
Meet New York Gastroenterology Associates
New York Gastroenterology Associates is a premier independent gastroenterology practice in New York City. NYGA consists of caring gastroenterologists practicing in office locations around New York City. Recognized for providing top-quality GI care, all of our physicians are board-certified and affiliated with Mount Sinai… Learn More »
Also Check: What Should You Eat When You Have Ulcerative Colitis
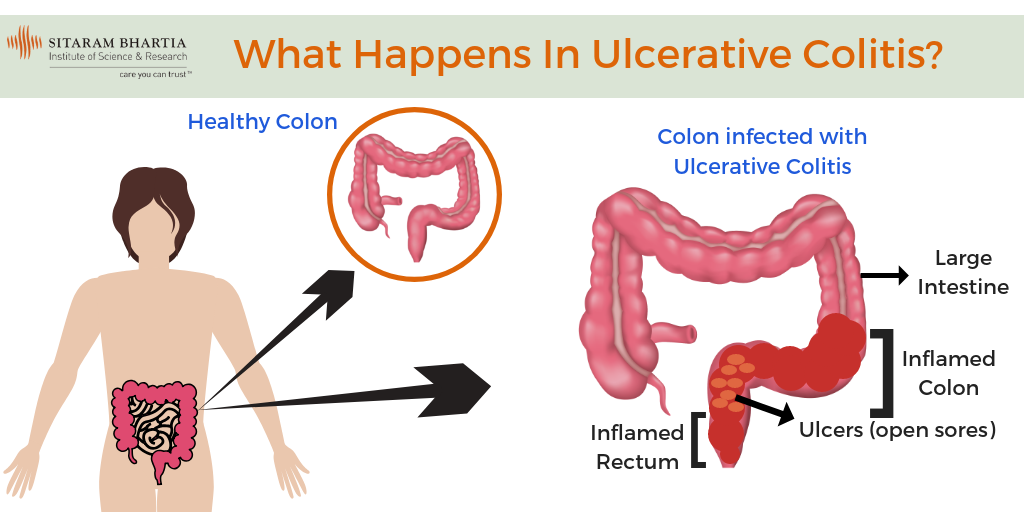
What Are The Most Common Ulcerative Colitis Symptoms
Early ulcerative colitis symptoms usually include things that could easily be overlooked. Dont be afraid to talk to a doctor if youre having any worries though, even if your symptoms seem mild. If symptoms are ongoing and start to feel more severe, like persistent pain in your abdomen or unintentional weight loss, you should seek medical treatment as soon as possible.
Here are some of the most common symptoms of ulcerative colitis to watch out for, per the NIDDK:
Okay, so this isnt the most pleasant one to start with, but it is actually the most common ulcerative colitis symptomits also a pretty good tip-off that something isnt quite right and that you should schedule an appointment with your doctor. Remember those ulcers we talked about earlier? Yeah, thats where the blood in your stool comes from, and you might also see mucus in there as well.
This is another pretty common symptom, and contrary to popular belief, those ulcers in the colon are not actually what causes the pain. Instead, its a combination of abdominal cramping and bowel distension that occurs due to the inflammation in the intestines, according to a 2013 study published in Inflammatory Bowel Diseases.1
With all thats going on in the digestive tract with ulcerative colitis, nausea can sometimes be an issue. This occurs more often when symptoms are severe, or if the inflammation affects more of the large intestine, according to the NIDDK.
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Don’t Miss: Turning Patients Every 2 Hours To Preventing Pressure Ulcers
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
You May Like: Does Apple Cider Vinegar Help Ulcerative Colitis
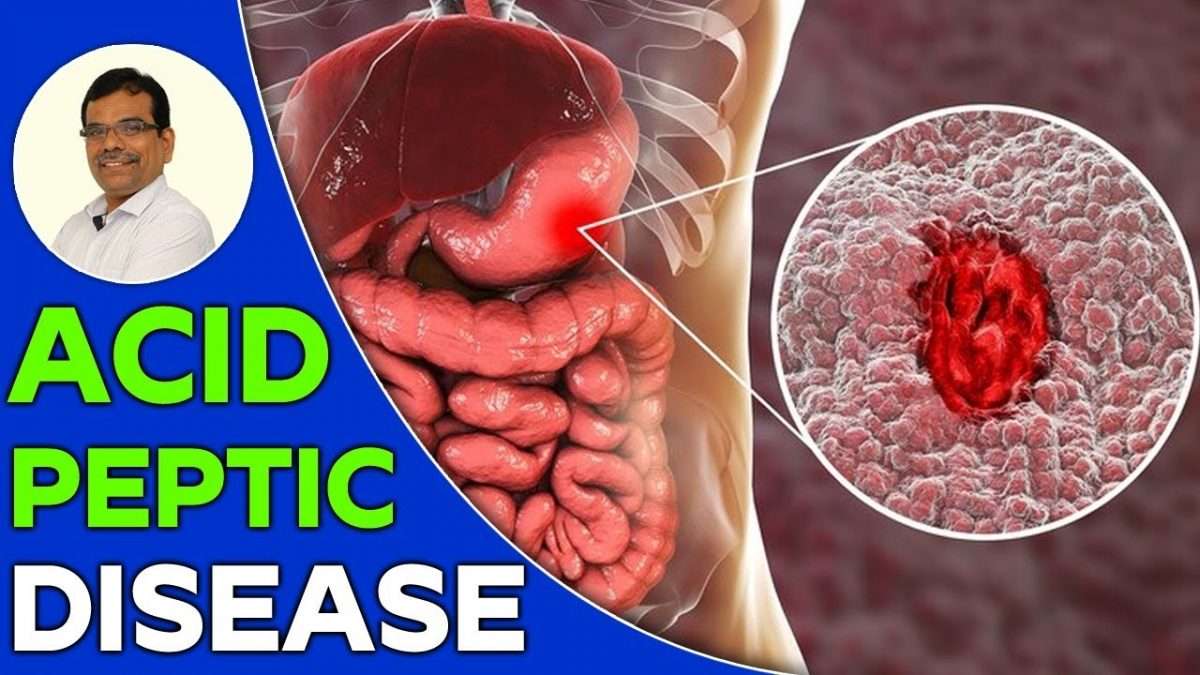
How Do Nsaids Cause A Peptic Ulcer
To understand how NSAIDs cause peptic ulcer disease, it is important to understand how NSAIDs work. Nonsteroidal anti-inflammatory drugs reduce pain, fever, and inflammation, or swelling.
Everyone has two enzymes that produce chemicals in your bodys cells that promote pain, inflammation, and fever. NSAIDs work by blocking or reducing the amount of these enzymes that your body makes. However, one of the enzymes also produces another type of chemical that protects the stomach lining from stomach acid and helps control bleeding. When NSAIDs block or reduce the amount of this enzyme in your body, they also increase your chance of developing a peptic ulcer.
Burning Pain In Your Abdomen
This may seem like a no-brainer but the most common sign that people experience when they have a stomach ulcer is a persistent burning pain in their abdomen. This sensation occurs when juices in the stomach used for digestion come into contact with the open sore. For the most part, the pain is felt from the breastbone to navel and is often worse at night than during the day. On the other hand, if you are someone who frequently skips meals, you may find that you experience this pain much throughout the daytime.
Don’t Miss: How To Calm Ulcerative Colitis Flare Up
When To Call Your Doctor
After your UC surgery, youll stay in the hospital for 3 to 7 days. This window of time allows your surgeon to monitor you for signs of complications.
Both ileostomies and pouch surgeries will require a 4- to 6-week recovery period.
During this time, youll meet regularly with your surgeon, doctor, and possibly an enterostomal therapist.
An enterostomal therapist is a specialized therapist who works directly with people whove had their colon removed.
Your care team will likely cover the following points with you to help improve your recovery:
- Eat well. Good nutrition can help your body heal and help you avoid post-operation health issues. Nutrition absorption can be an issue after these surgeries, so eating well will help you maintain healthy levels of nutrients.
- Hydrate. Hydration is important for your overall health but especially for your digestive health. Drink six to eight glasses per day at a minimum.
- Stay active. Work with a rehab therapist or a physical therapist to slowly recover your physical capabilities, and exercise when you can. Staying active is a great way to care for your overall health as you recover, but too much activity too soon could complicate your recovery.
- Manage stress. Anxiety or emotional stress can cause stomach issues, which can increase your risk for an accident.
Surgery is usually a last-resort option for UC, partly due to the fact that any surgery can pose risks and complications. Some of the risks of UC surgery include: