Several Classes Of Drugs May Be Prescribed To Control Inflammation In Various Ways
- Anti-inflammatory medications: Your doctor may prescribe anti-inflammatory medications as a first step of treatment to reduce inflammation.
- Immune system suppressors: Since the intestinal lining becomes damaged due to the immune response, these drugs may be prescribed to target your immune system and reduce the inflammatory response.
Diagnosis Of Left Side Colitis
Diagnosing left side colitis correctly is the most important step to moving ahead in the treatment.
Endoscopy is performed by the doctors, in which a camera is used to create pictures of the inside of the colon. This helps the doctor to look for signs of inflammation inside the colon. These signs include redness, water retention, and irregularities.
Once the camera goes beyond the splenic flexure the signs of left side colitis disappear.
Ulcerative Colitis And Crohn’s Disease Pain Locations Are Usually Different
Ulcerative colitis and Crohn’s disease pain locations are different, even though both of these conditions are classified as inflammatory bowel diseases . Also, the nature and location of pain vary from one person to the next.
This article explores Crohn’s and ulcerative colitis pain locations and types, what pain in different parts of the abdomen may mean, and how Crohn’s and ulcerative colitis pain locations can help with a diagnosis.
Jessica Olah / Verywell
You May Like: Signs Of Ulcerative Colitis In Adults
Fibers Effect On The Oral Cavity: As Sticky Asglue
The human mouth is primarily intended to cutand chop flesh, not grind indigestible fibers. Unlike humans,cows have so-called hypsodont teeth, which extend very far abovethe gum line and grow continuously to accommodate a lifetime ofwear-and-tear from grinding fibrous grasses.
We arenât as luckyâour teeth are brachydont,and arenât intended for chewing fiber, otherwise, after a decadeor so, you simply wouldnât have any teeth left to argue thispoint with clarity. Thatâs why the fiber for humanconsumption is crushed, milled, or ground first, and requireslittle or no chewing. But even after processing, it affects theoral cavity with a menacing vengeance:
What Is Uc Cramping
Abdominal pain and cramping from UC is most commonly caused by the conditions inflammatory process, according to Christina Ha, MD, a gastroenterologist at Cedars-Sinai Medical Center in Los Angeles. Such inflammation usually starts at the rectum and moves throughout the large colon. The greater the inflammation, the more severe the pain.
Also Check: What Is Refractory Ulcerative Colitis
Risk Factors Of Ulcerative Colitis
- Age: While this disease can occur at any age, ulcerative colitis usually begins before the age of 30.
- Race or ethnicity: Although whites have the highest risk of the disease, it can occur in any race.
- Family history: Youre at a higher risk if you have a close relative, such as a parent, sibling or child with the disease.
- Isotretinoin use: Isotretinoin, formerly sold under the brand name Accutane, is a medication sometimes used to treat scarring cystic acne or acne that does not respond to other treatments. While there have been some connections between isotretinoin and ulcerative colitis, the reports are conflicting as to whether isotretinoin actually causes ulcerative colitis.
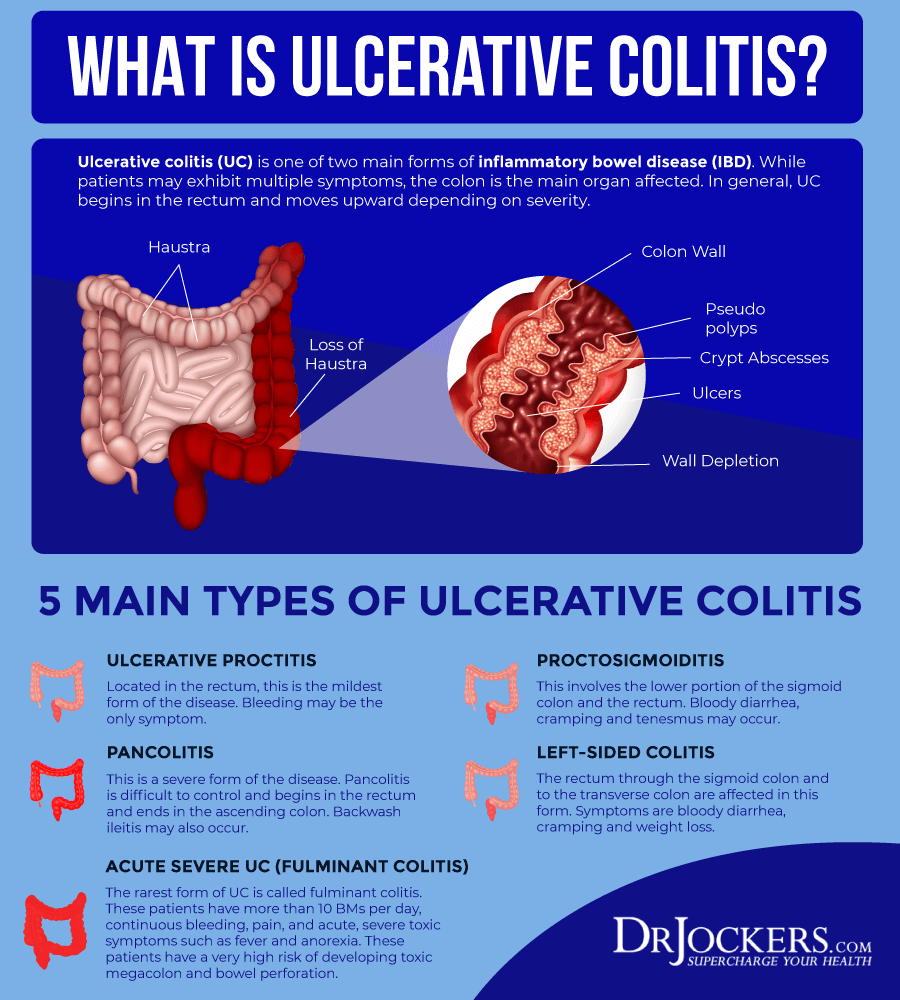
What Is Distal Ulcerative Colitis
Left-sided colitis is a form of ulcerative colitis that begins at the rectum and extends up to the left colon .
It is a life-long chronic condition which cannot currently be cured and is part of a group of conditions known as inflammatory bowel disease . UC causes inflammation of the gastrointestinal tract .
In UC small ulcers develop on the colons lining which produce pus and mucus. This can cause abdominal discomfort and frequent emptying of the colon .
Approximately 30% of people with UC are diagnosed with left-sided colitis.
You May Like: Natural Cures For Gastritis And Ulcers
Moderate Or Extensive Disease
Patients with inflammation proximal to the sigmoid colon or left-sided disease unresponsive to topical agents should receive an oral 5-ASA 5-Aminosalicylic Acid Several classes of drugs are helpful for inflammatory bowel disease . Details of their selection and use are discussed under each disorder . Details of their selection and use are discussed under each disorder . Details of their selection and use are discussed under each disorder or corticosteroid therapy as well as those who are corticosteroid-dependent. Moreover, a combination of immunomodulator and anti-TNF therapy Anti-TNF drugs Several classes of drugs are helpful for inflammatory bowel disease . Details of their selection and use are discussed under each disorder (see Crohn disease treatment and ulcerative colitis… read more is sometimes helpful. Finally, in some patients who fail to respond to corticosteroids, immunosuppressants, or biologics, a trial of the Janus kinase inhibitor tofacitinib, or a trial of sphingosine 1-phosphate receptor modulator ozanimod can be considered.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Also Check: If You Have An Ulcer Where Does It Hurt
The Consumers Guide To S1p Receptor Modulators For Ulcerative Colitis
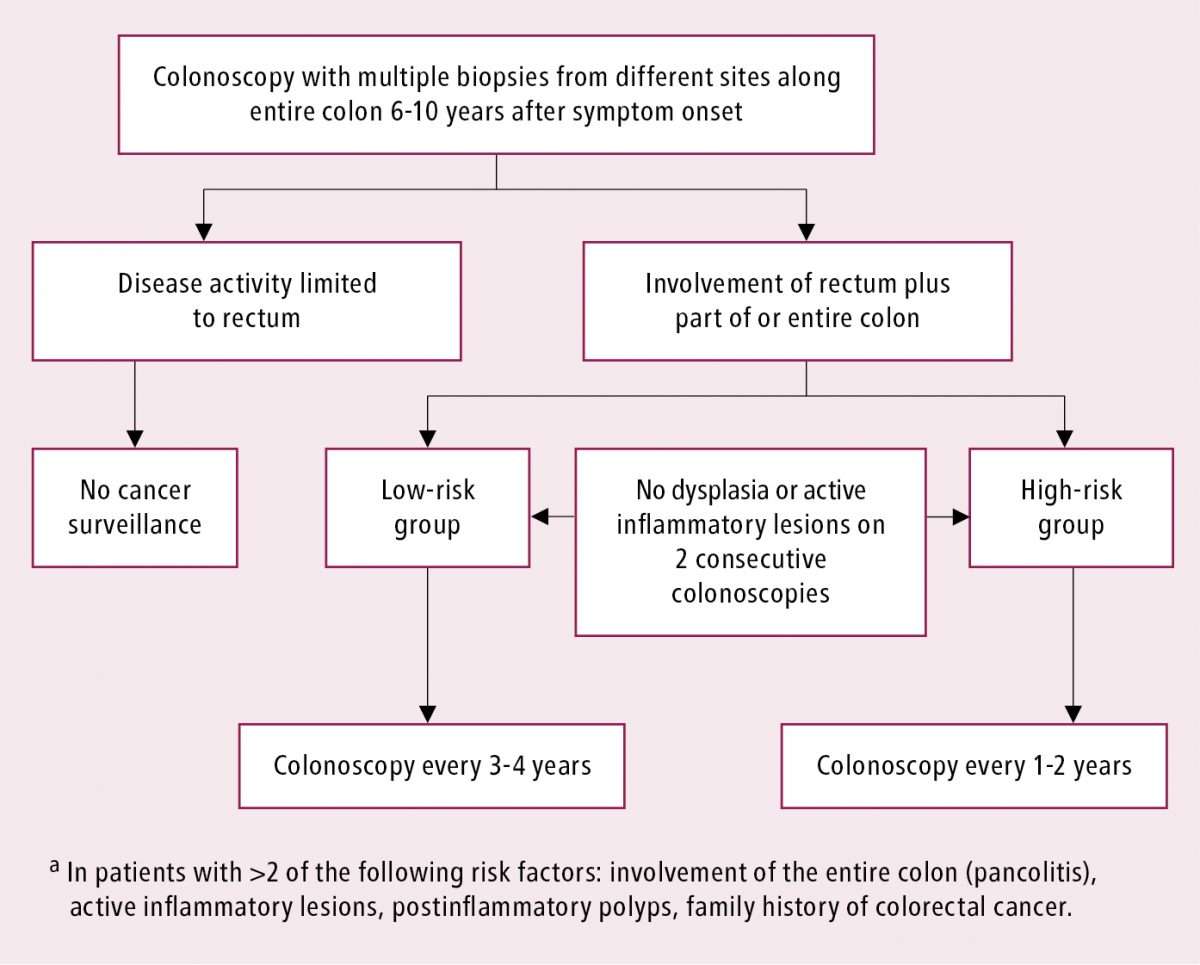
A colonoscopy can help doctors see how much ulceration and bleeding has occurred in the mucosa .
A similar but less intrusive procedure is a flexible sigmoidoscopy. This procedure uses a flexible tube with a light to view just the lower portion of the colon. A definitive diagnosis of ulcerative colitis is generally made using endoscopy that is, a colonoscopy or a sigmoidoscopy.
In addition to reported symptoms, lab tests, and endoscopy results, some people receive CT scans to assess inflammation in the colon, although the role of these scans is currently more limited in UC than in Crohns disease.
If the UC is in remission, the severity of the disease, which is determined using a rating system based on colonoscopy results, can help predict how likely it is to relapse within five years, according to a study published in August 2021 in the International Journal of Colorectal Disease.
Fibers Effect On The Stomach: The Luck Stopshere
The digestion of protein is the exclusiveprovenance of the stomach. When gastric digestion commences, thecontents of the stomach are churned inside, until itâscompleted .
Fiberâs specific propertiesâwater absorbency,expansion, stickiness âinterfere with digestionand may cause an array of gastric disorders. Fiber-relatedproblems become more pronounced with age because of theinevitable wear-and-tear on the internal organs. Insoluble fiberaffects the stomach particularly hard because it tends tocongregate and form lumps, and its rapid expansion fills thestomach with idle bulk.
You donât even need to consume that much fiberto feel its punch. For example, TV commercials for antacids arecommonly shot inside Mexican restaurants because beansâa mainstaple of Mexican cuisineâcommonly cause heartburn, even thougha 100 g serving of beans contains a paltry 4 to 5 g offiber. Just imagine the cumulative impact on the aging stomachof 30 to 40 grams of fiber consumed daily. Here are the mostprominent problems:
As you can see, the relationship between thestomach and the fiber is awkward at best, ruinous at worse.Well, what else would you expect when matching a primarydigestive organ with an indigestible substance?
Also Check: Ulcerative Colitis Skin Rash Pictures
What Are The Possible Complications Of Pancolitis
After you get a diagnosis like pancolitis, you might be curious about what your future might look like. Will your disease get worse? Could pancolitis cause serious long-term problems?
Pancolitis damages the colon, explains Dr. Kayal, which eventually can lead to a few complications like these:
-
Fulminant colitis, a more severe form of UC
-
Toxic megacolon, extreme inflammation in the colon
-
Severe bleeding
-
A hole called a perforation in the colon
Your risk for colorectal cancer also increases the longer you live with pancolitis. That’s because inflammation causes cells in your colon to change. In time, those cells could turn into cancer. However, before you panic about possible complications, you should know that there are good treatments available to prevent them.
What Is Left Side Colitis
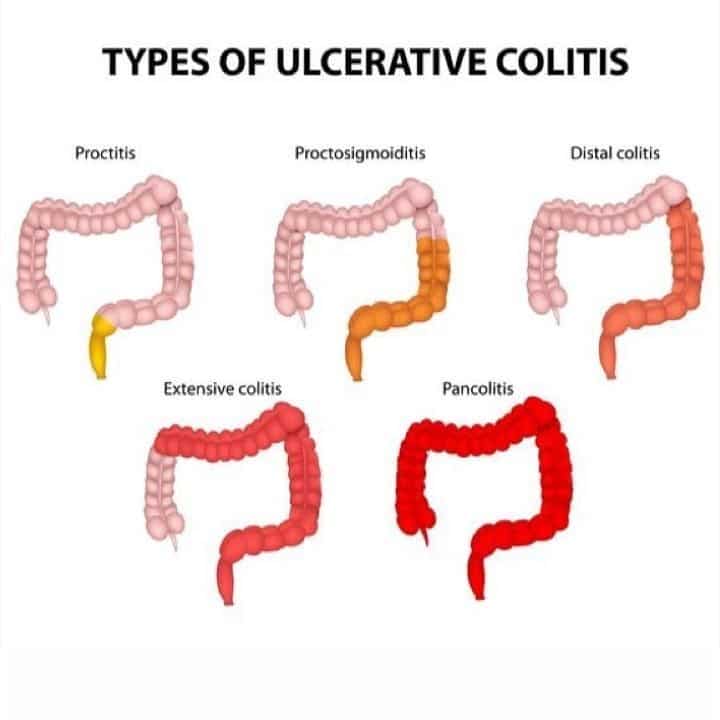
Ulcerative colitis is a condition in which the colon gets inflamed. Also known as distal ulcerative colitis, left sided colitis is a type of ulcerative colitis in which only the left side of the colon is inflamed. It is a chronic condition and a person experiences symptoms throughout life after being diagnosed with it.
The distal colon extends from the rectum up to the colon and stops at the splenic flexure, a point where the colon bends. Its inflammation leads to small ulcers in the lining of the colon which lead to mucous and pus and other symptoms.
Don’t Miss: Pressure Ulcer Interventions And Rationales
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Diagnosing And Treating Ulcerative Colitis
There are four ways to diagnose ulcerative colitis. It is usually treated through medications or surgery.
How ulcerative colitis is diagnosed:
- A review of the patients family history of UC
- Physical exam to check for swelling, listen for sounds in the abdomen, and check for tenderness or pain in the abdomen
- Lab tests of blood and stool that check for anemia, inflammation elsewhere in the body and other markers common to UC patients
- Use of an endoscope, a long, flexible tube with a camera, to look at the colon
: National Institutes of Health
Treatment options depend on the severity of the patients ulcerative colitis. Surgery may require removing the colon and rectum in the most severe cases.
Don’t Miss: Can You Eat Oatmeal With Ulcerative Colitis
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Also Check: Low Residue Diet For Ulcerative Colitis
Whole Psyllium Husk Psyllium Husk Powder And Psyllium Seed Powder Whats The Difference
Psyllium is typically processed into one of three forms: whole psyllium husk, psyllium husk powder, and psyllium seed powder. Although each supplement is derived from the same raw seeds, they will contain different amounts of soluble fiber which will change the products properties.
Supplements labeled as 100% whole psyllium husk, for example, will consist of only plantago ovata seed husks without any further processing. The husks are small, grain-like particles that are packed with roughly 70% soluble fiber.
When the whole husks are used in recipes, however, they will add a grainy texture that can be unpleasant. This is when psyllium husk powder can be helpful.
Because of its enhanced fiber content and superior texture, psyllium husk powder is the most widely used psyllium product, as a dietary supplement and as a gluten-free, keto-friendly culinary staple.
This is not to be confused with psyllium seed powder, which consists of the husk and seed ground together. This form of psyllium has a lower soluble fiber content and will not provide the same health benefits or properties as psyllium husk powder.
Also Check: Difference Between Ulcerative Colitis And Hemorrhoids
Medication Is Often Not Enough For Helping With Ulcerative Colitis Flareups Supplementing With Psyllium Husk Can Go A Long Way In Helping With Remission
Irritable bowel diseases are skyrocketing around the globe. There are about 1.6 million people in America alone who suffer from IBD. The most common form of IBD is a disease known as ulcerative colitis which is an autoimmune disease and a chronic inflammation of the larger intestine. The disease is characterized by bloating, abdominal pain, diarrhea and blood as a result of ulcers in the gut.
There is no known cure for the disease, but its symptoms are manageable with conventional anti-inflammatory medication like prednisone.
Medication is not enough to control and manage UC symptoms. Many chronic sufferers of the disease must cut back on milk, fried foods, spicy foods, certain kinds of seeds etc as they may exacerbate symptoms or take people out of remission.
Does Psyllium Husk Help with Ulcerative Colitis?
There are, however, some natural supplements that have shown much promise in treating IBDs, particularly ulcerative colitis. From our experience, the most effective natural supplement to help with UC is psyllium husk. Psyllium husk is a smooth insoluble form of fiber. It not only helps with constipation but it also helps with diarrhea. In this sense, psyllium husk acts as a colon cleans which may remove certain toxic and non-toxic elements that may be contributing to your flare-up.
Not only does it help prolong remission, but it also has a healing effect on the colon by repairing the protective lining system in the colon which also reduces flare-ups.
What Are The Symptoms Of Pancolitis
No matter which type of ulcerative colitis you have, you can expect some diarrhea. “When the whole colon is involved, most of the time people have frequent diarrhea, with or without blood,” says Russell Cohen, M.D., a professor of medicine and director of the Inflammatory Bowel Disease Center at the University of Chicago Pritzker School of Medicine.
Finding blood in the toilet when you poop can be scary. The bleeding comes from sores called ulcers that pancolitis inflammation creates in the lining of your colon. The closer to your rectum those sores are, the more the blood will look bright red. Blood that comes from higher up in your digestive tract is darkerusually brown or black. Bleeding can be alarming, but it’s one of the symptoms that UC drugs were designed to treat.
Other pancolitis symptoms are the same ones that people have with any , including:
How severe your diarrhea and other symptoms get depends, in part, on how much of your colon is inflamed. “People who have more of their colon involved may be at risk for more severe disease,” explains Dr. Kayal.
Read Also: Side Effects Of Ulcerative Colitis
Preparing For An Appointment
Symptoms of ulcerative colitis may first prompt you to visit your primary health care provider. Your provider may recommend you see a specialist who treats digestive diseases .
Because appointments can be brief, and there’s often a lot of information to discuss, it’s a good idea to be well prepared. Here’s some information to help you get ready, and what to expect.
Causes Of Ulcerative Colitis
The cause of ulcerative colitis is unknown. Researchers believed that stress was a possible cause, but they no longer believe that this is a viable explanantion. However, stress can aggravate symptoms. There are now two possibilities for the cause of ulcerative colitis.
- Immune system: some scientists believe that a virus or bacterium may trigger ulcerative colitis. The digestive tract becomes inflamed when the immune system tries to fight off the invading pathogen. It is also possible that inflammation may stem from an autoimmune reaction.
- Hereditary: youre more likely to develop ulcerative colitis if you have a parent or sibling with this disease. However, most people who have ulcerative colitis do not have a family history of ulcerative colitis.
Read Also: How Did I Get Ulcerative Colitis
How To Treat Pain
There are various treatment options for UC, and the best approach for a person will depend on the severity of their symptoms. Over-the-counter medications can sometimes help relieve the pain that UC can cause. However, severe cases require stronger pain relievers.
Medications for the treatment of UC include:
Symptoms Of Chronic Ulcerative Colitis
Symptoms vary among patients depending upon where in the colon and rectum inflammation resides as well as its intensity. Inflammation may affect a small portion of the colon and rectum or, in worse cases, engulf the entire large intestine.
Patients with chronic ulcerative colitis are at risk of: anemia, from bleeding within the colon and rectum bone disorders, including osteoporosis, because nutrients are not being absorbed by the intestines and skin and eye disorders, common among patients with immune system diseases, such as rheumatoid arthritis. Patients with chronic ulcerative colitis also are at a higher risk of developing primary sclerosing cholangitis, a disorder of the bile ducts in the liver, and colon cancer.
Signs and symptoms of chronic ulcerative colitis can include:
- Persistent diarrhea or loose stools
Also Check: How Serious Is A Stomach Ulcer
Don’t Miss: How Can I Tell If I Have An Ulcer