How To Cope With Ulcerative Colitis Treatment Side Effects
According to Medscape, ulcerative colitis is an inflammatory bowel disease that causes sores to appear in your large intestine. Experts at The Crohn’s & Colitis Foundation explain that UC is believed to result from your immune system continuing to fight off an infection that’s already been handled. Since there are no bacteria or viruses to fight, the white blood cells attack your colon, causing ulcers filled with pus. When the mucus is released, it causes inflammation, which in turn creates the need to poop more frequently.
There are three types of UC . One kind is ulcerative proctitis, which affects a small part of your rectum. Next, left-sided colitis affects your rectum and the section of your colon directly attached to it. Finally, you get diagnosed with extensive colitis when the inflammation affects your entire colon.
Several factors increase the likelihood of you developing UC. While most cases get discovered in patients aged 15 to 30, anyone can be diagnosed at any age. However, the medical professionals at Cleveland Clinic state that your chances increase by nearly 20% if a close family member has the disease, especially if you’re Jewish. Additionally, those who consume a high-fat diet or take NSAIDs like Advil or Motrin have a higher chance of developing UC.
Practical Advice For What To Eat On An Ulcerative Colitis Diet
Many organizations post food shopping lists for Ulcerative Colitis Disease. These resources are a good starting point. Download a list and make it your own. Mark off your trigger food and add foods that you can safely eat.
Plan ahead and enhance your weekly menus with MealPro Ulcerative Colitis meal delivery service. These anti-inflammatory meals are designed to eliminate known trigger foods and reduce flares.
Roasted salmon: This meal is full of flavor while providing healthy omega-3s with a portion of asparagus and yellow bell peppers. Roasted potatoes round out the meal for a satisfying choice in carbs.
Turmeric Turkey: Lean turkey seasoned with the anti-inflammatory spice turmeric. Served with fresh green beans and bake yams. Rice is the foundation of this meal.
So, can Ulcerative Colitis symptoms change the way you eat? Yes. Although it is possible to adjust the foods you eat to improve and enhance your quality of life.
I Have Heard That Fiber Is Good For Ulcerative Colitis What Does Onpoint Say
-
We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well
-
If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently
Recommended Reading: What Is Best Medicine For Ulcer
Don’t Miss: What Is The Difference Between Ulcerative Colitis And Ibs
Carbonated Beverages May Increase Abdominal Pain
Fizzy drinks may cause gas or bloating in some people, possibly leading to increased abdominal discomfort. Many soft drinks or carbonated energy drinks also contain caffeine, which can stimulate the intestines and worsen diarrhea, according to Mayo Clinic. Drinking sugary soft drinks can contribute to obesity as well, which raises the risk of heart disease and other health problems.
An analysis of drinks published in May 2019 in the journal Medicine found that a high intake of soft drinks was associated with an increased risk of developing Crohns disease, while a high intake of tea was associated with a lower risk of the inflammatory bowel disease. For a refreshing beverage, choose fruit-infused water or herbal iced teas.
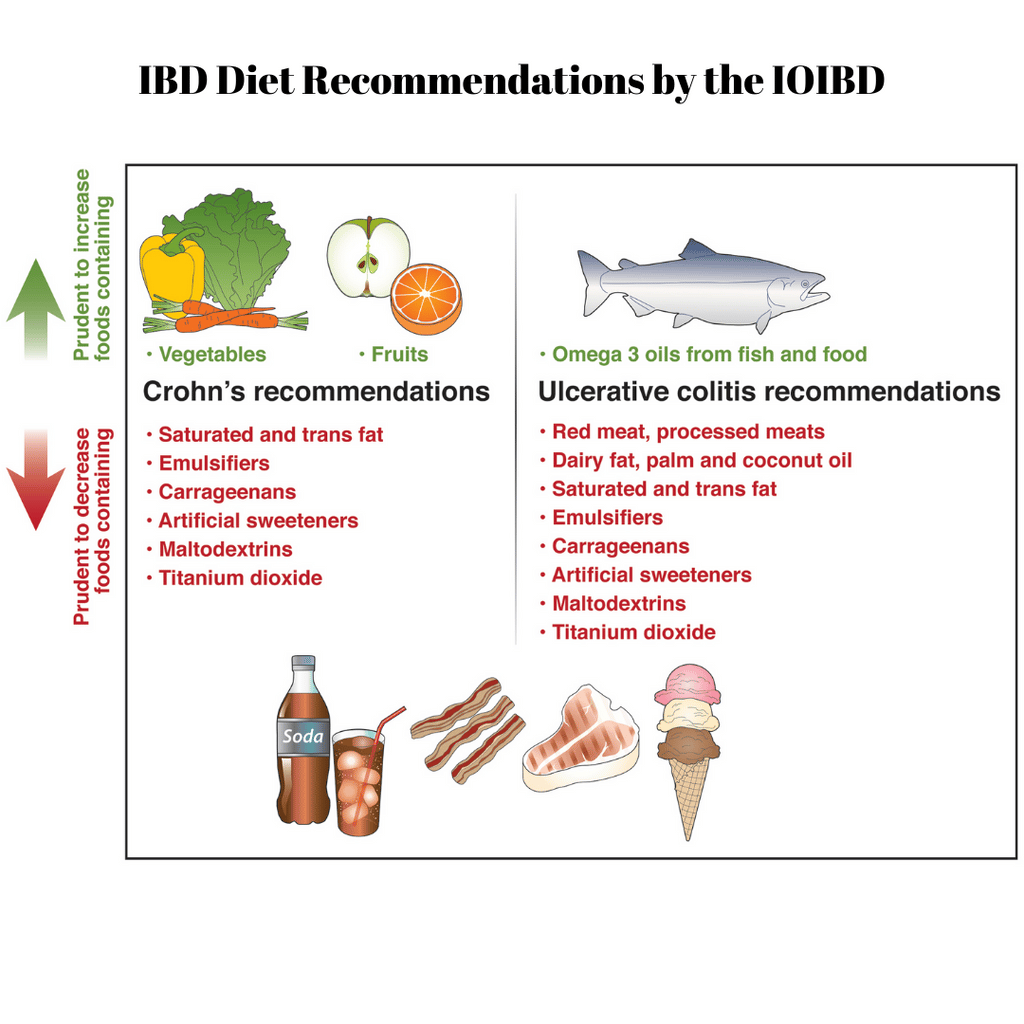
Diet Recommendations For Ulcerative Colitis Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages.
- Try incorporating more omega-3 fatty acids in your diet. These fats may have an anti-inflammatory effect. They are found in fish, including salmon, mackerel, herring and sardines.
- Patients often find that smaller, more frequent meals are better tolerated. This eating pattern can help increase the amount of nutrition you receive in a day.
- Consider taking nutritional supplements if appetite is poor and solid foods are not tolerated well .
Dont Miss: How Do Stomach Ulcers Heal
Also Check: Medications Used For Ulcerative Colitis
Youre Ignoring How Stressed You Really Are
Drs. Bloomfeld and Yun agree: When asked, people with UC often report experiencing stress before a flare. A study published in March 2019 in the Journal of Crohns and Colitis followed 417 people with IBD, which includes UC, and found that experiencing a stressful life event or new stressors in the previous three months was commonly linked to a flare-up.
Stress can trigger inflammation in the gut, worsening the symptoms of UC, according to a study published in 2019 in Frontiers in Pediatrics. Plus, stress can interfere with your usual routine, leading to poor sleep and medication and eating habits.
At Yuns clinic, a psychologist teaches relaxation exercises to people with UC. Learning techniques such as meditation or yoga may help you manage stress.
What Causes Ulcerative Colitis
The cause of ulcerative colitis is unknown but it is believed to be caused by a combination of several factors including an overactive immune system, genetics, and the environment.
- Overactive immune system: It is believed that in ulcerative colitis, the immune system is triggered to mistakenly attack the inner lining of the large intestine, causing inflammation and symptoms of ulcerative colitis.
- Genetics: Ulcerative colitiscan run in families. The genetic link is not entirely clear but studies show that up to 20% of people with ulcerative colitis have a close family member with the disease.
- Environment: Certain environmental factors including taking certain medications , and eating a high fat diet may slightly increase the risk of developing ulcerative colitis.
Physical or emotional stress, and certain foods do not cause ulcerative colitis, however, they may trigger symptoms in a person who has ulcerative colitis.
Don’t Miss: Best Cranberry Juice For Ulcers
How Long Do Flare
UC is a condition that is unique to every individual. Some people experience flare-ups that last a few days, while others experience flare-ups that last weeks. Likewise, individuals may go from a mild flare-up to a severe one and then back again.
If a person is experiencing a severe flare-up that persists, they should speak with a doctor. The doctor will help them get their symptoms under control and improve their quality of life.
Herbal Remedies And Supplements
There are lots of supplements that claim to treat Crohns and Colitis. But there isnt enough evidence to recommend any herbal remedies or supplements. This is because its difficult to know whether the supplement is directly affecting a persons Crohns or Colitis or whether something else is causing a change in symptoms. Also, everyone is different so what helps one person may not help another.Some people find that some herbal remedies, such as aloe vera or curcumin , help them manage their symptoms when they use them together with their prescribed medicines. There have been reports of cannabidiol , an ingredient in cannabis, helping with symptoms like diarrhoea, pain and loss of appetite. But we dont know enough about how it works or how much is a safe amount to take. It isnt currently recommended and isnt available on prescription for people with Crohns or Colitis.There have been claims in the media about the benefits of kefir a fermented milk drink that contains probiotics. But there isnt any medical evidence to show that it helps people with Crohns or Colitis.If you want to take herbal remedies, its important to speak to your IBD team or dietitian first. Dont stop taking your prescribed medicine without talking to your IBD team, even if your symptoms improve.
I think it is so important to remember that the relationship with food and IBD is so different for everyone!
Don’t Miss: Is Soy Milk Good For Ulcerative Colitis
Spinach Artichoke Yogurt Dip
This easy-to-make dip will help you sneak in your daily veggie servings. Artichokes are a low fiber food thats generally safe for people with ulcerative colitis. Theyre also a prebiotic. That means they feed the good bacteria in the gut and may support colonic health.
Combine one can of artichoke hearts and a package of chopped spinach with low fat yogurt and shredded cheddar cheese.
Pour the mixture into a casserole dish. Then bake at 350°F for 20 to 25 minutes. Serve with sliced carrots and cucumbers for dipping.
Ulcerative Colitis Diet: Food Preparation And Meal Planning
While the idea of an elimination diet or restricting your intake of fiber, fat or other trigger foods may seem daunting, meal planning and preparing your food ahead of time can take some of the stress out of eating in a flare up. If your appetite is impacted as well, you can batch cook and eat what you want of a larger pre-prepared meal when you feel like eating, rather than preparing yourself a whole new meal from scratch.
The Crohns and Colitis Foundation indicates that rates of depression and anxiety are higher in those with IBD, so anything that can reduce stress for those with ulcerative colitis might be helpful for managing mental health. As such, pre-planned meals based around particular dietary needs can make the day-to-day experience of ulcerative colitis slightly less stressful, and may make the experience of a flare up more bearable.
This article is for informational purposes only and is not meant to offer medical advice.
Read Also: How Dangerous Is Ulcerative Colitis
Common Supplements Recommended For Ibd Patients
Your healthcare provider may recommend that you take vitamin or mineral supplements, especially if you are experiencing nutritional deficiencies. We can help you learn about supplements that are commonly recommended for IBD patients.
This information can help you learn which vitamins and minerals are important to maintain your nutrition, along with the various foods you may want to try as part of your IBD-friendly diet.
Your body is unique. What works for one patient, will not work for everyone. Check with your healthcare providers before starting any supplements, as you will need proper dosing.
What Are Some High
Whole-grain breads, cereals, and pasta, whole vegetables and vegetable sauces, whole fruits, including canned fruits, yogurt, pudding, ice cream, or cream-based soups with nuts or pieces of fruits or vegetables, tough or coarse meats with gristle and luncheon meats or cheese with seeds, peanut butter, salad dressings with seeds or pieces of fruits or vegetables, seeds or nuts, coconut, jam, marmalade.
Read Also: Can You Donate Blood If You Have Ulcerative Colitis
You May Like: Manuka Honey For Leg Ulcers
Lcerative Colitis Diet Plan
Following an Ulcerative Colitis diet plan is a bit more complicated than something like an IBS plan. The ideal diet for UC patients will vary depending on their symptom severity. For example, during flare-ups, youll want to be gentle on your intestines, eating low-fiber foods. However, when you arent having flare-ups, its healthier and more protective to feed your gut bacteria the fiber it needs.
There is a delicate balance that UC patients need to maintain, and its often a fine line with much back-and-forth from week to week. Your best option is to keep a food journal and log all of your symptoms each day. This way, you can find what works best for you. If you have any questions about how to create a food journal or about other treatments to minimize your UC symptoms, get in touch with the colorectal experts at the Colorectal Clinic of Tampa Bay.
Choose Low Fodmap During A Flare
The Med diet is super healthy, but during a flare, the low Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols diet is your friend. Low-FODMAP plans reduce short-chain carbohydrates and sugar alcohols that spell trouble for UC sufferers. This diet limits carbohydrates that are poorly absorbed and highly fermentable by the gut microbiota, says Warren.
Read Also: Ulcerative Colitis And Menstrual Cycle
What Foods Should I Avoid If I Have Ulcerative Colitis
While no single diet has been proven to treat the intestinal inflammation that causes ulcerative colitis, avoiding some foods may help alleviate symptoms during a flare-up. Trigger foods are not the same for everyone, so it is important to track what you eat and identify your own troublesome foods.
Avoid these foods during an ulcerative colitis flare-up, as they can be potential trigger foods:
- Foods high in insoluble fiber: whole grain foods , fruits with skin and seeds, some raw green vegetables, broccoli, cabbage, brussel sprouts, nuts, seeds, beans, lentils and peas
- Dairy products: milk, cream cheese and soft cheeses
- Non-absorbable sugars: sugar alcohols such as sorbitol and mannitol, which are found in sugar-free foods like gum, candy and ice cream
- High-sugar foods: pastries, candy, chocolate and juices
- High-fat foods: butter, margarine and cream, as well as greasy foods such as pizza and fried foods
- Alcoholic and caffeinated beverages: beer, wine, liquor, soda and coffee. Elimination of alcohol may not be required, but it should be consumed in moderation.
What Foods Can I Eat When I Am Having An Ulcerative Colitis Flare
Certain foods are less likely to make your UC symptoms worse and can also help to reduce inflammation. These foods help settle your stomach and ensure you receive enough vitamins and minerals during an UC flare and include:
- Low-fiber fruits such as bananas, cantaloupe, honeydew melon, and cooked or canned fruits
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Refined grains, found in sourdough, potato or gluten-free bread, white pasta, white rice, mashed potatoes, and oatmeal
- Fully cooked, de-seeded, skinless, non-cruciferous vegetables such as asparagus tips, cucumbers, potatoes, and squash
- Homemade protein shakes or oral supplements
- Use olive oil instead of other oils or fats
- Herbal or green tea.
Also Check: Best Medicine For Ulcerative Colitis
Should I Take Extra Vitamins And Minerals
Yes, you should take a complete multivitamin with minerals.
If you take steroids or limit your intake of dairy products, you should also take extra calcium and vitamin D .
If you are take sulfasalazine you may need to take folic acid.
Iron and vitamin B12 deficiencies are common with IBD, so you may need to have blood tests to measure these nutrients.
With prolonged diarrhea, you may also need magnesium, zinc and potassium supplements. An electrolyte drink, such as Drip Drop, may help add these nutrients back into your body.
Check with your doctor if you are concerned about your nutrition.
How Can I Make My Colitis Worse
Also Check: Can Ulcers Cause Heart Palpitations
Tips For Preparing Nutritious Foods For Uc
Its one thing to know which foods are nutritious for you, but another to safely consume them. As one MyCrohnsAndColitisTeam member put it, The hard part is getting your nutritional requirements in with limited choices. Practicing meal planning and preparation techniques can be helpful to ensure adequate nutrition.
Members often share creative ways theyve found to incorporate nutritious foods into their diet safely. I made some pureed green sauce with greens, anchovies, garlic, and EVOO to add to roasted veggies and soups, said one. I have a Nutri Ninja. It purees my fruits and veggies, so I eat lots of smoothies with almond milk and Activia yogurt added, shared another.
It may also be helpful to purchase meal replacements, such as protein shakes, to keep your weight up. One member had a tip for weight gain: I increase the recipes that use lots of natural fats olive oil, coconut oil, coconut cream, avocado and I might increase my red meat. All of those make me feel super healthy.
During a flare, ulcerative colitis symptoms become more severe, and certain foods can worsen them further.
Following these guidelines can keep you away from the most common food triggers during UC flares:
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Don’t Miss: Can You Donate Blood If You Have Ulcerative Colitis