How Diabetes Affects Your Body
Diabetes is a result of your bodys inability to produce or use insulin. Insulin is a hormone that allows your body to turn glucose, or sugar, into energy. If your body has difficulty metabolizing glucose, it can lead to high blood sugar levels. This can affect your bodys ability to heal wounds.
In people with diabetes, wounds tend to heal more slowly and progress more quickly, so its important to know what to look out for.
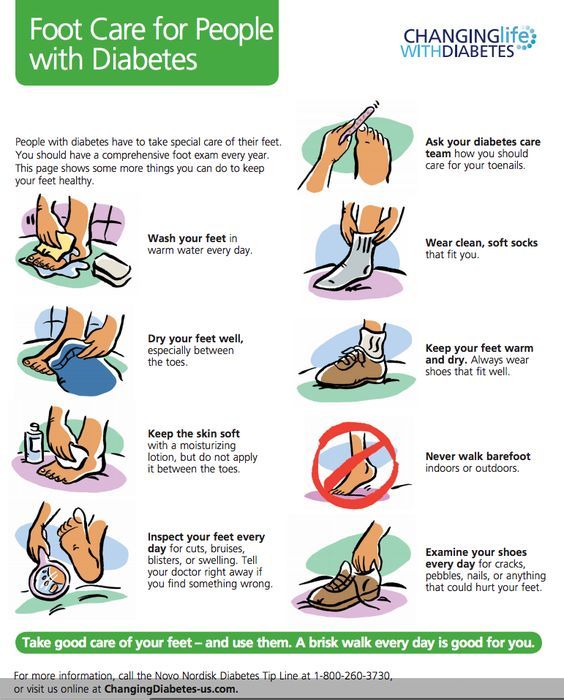
Although cuts, grazes, scratches, and blisters can occur anywhere on the body, the feet are one of the most common places of injury. A small wound on the foot can quickly develop into a foot ulcer.
Foot ulcers can become serious if left untreated. About 15 percent of people who have diabetes develop foot ulceration.
For this reason, its crucial to do regular self-checks and closely monitor any wounds closely. Catching wounds early is the only way to reduce your risk of complications.
Keep reading to learn more about the healing process, ways to speed it along, and how to improve your bodys healing powers long term.
When you have diabetes, a number of factors can affect your bodys ability to heal wounds.
Research Design And Methods
The precise date of ulcer onset is often difficult to determine, especially for those ulcers that are long established or of which the patient was unaware. It was for this reason that a prospective decision had been taken to document ulcer onset simply by calendar month. For the purposes of calculating the ulcer duration at referral, the date of onset was taken as the 15th day of that month. For ulcers that started in the same month that they were first seen, the date of onset was taken as the 15th day of the month if they were seen after that date. For ulcers first seen in the first half of the month of onset, ulcer duration was arbitrarily taken as 7 days.
Usual clinical management for neuropathic ulcers relies on regular debridement to remove surrounding callus, combined with offloading. The principle of offloading was to adjust footwear to ensure that continued trauma to the ulcerated area was minimized, but the method adopted had to comply with that which was both safe and acceptable to each patient. The method of choice of offloading of neuropathic ulcers on the plantar surface of the foot was the use of irremovable padded fiberglass slippers and, less frequently, with below-the-knee irremovable casts. Patients who were judged unsafe in casts, or who refused to wear them, were managed with removable orthoses , with the aim of achieving the most effective offloading practicable.
Establishing Extent Of Infection
Early recognition of the area of involved tissue can facilitate appropriate management and prevent progression of the infection . The wound should be cleansed and debrided carefully to remove foreign bodies or necrotic material and should be probed with a sterile metal instrument to identify any sinus tracts, abscesses, or involvement of bones or joints.
Plantar foot ulcers with a deep space infection.
Figure 3.
Plantar foot ulcers with a deep space infection.
Osteomyelitis is a common and serious complication of diabetic foot infection that poses a diagnostic challenge. A delay in diagnosis increases the risk of amputation.13 Risk factors associated with osteomyelitis are summarized in Table 1.3,1316 Visible bone and palpable bone by probing are suggestive of underlying osteomyelitis in patients with a diabetic foot infection.1314 Laboratory studies, such as white blood cell count and the erythrocyte sedimentation rate , have limited sensitivity for the diagnosis of osteomyelitis. Osteomyelitis is unlikely with normal ESR values however, an ESR of more than 70 mm per hour supports a clinical suspicion of osteomyelitis.13 Definitive diagnosis requires percutaneous or open bone biopsy. Bone biopsy is recommended if the diagnosis of osteomyelitis remains in doubt after imaging.3
Wound lacking purulence or any manifestations of inflammation
You May Like: Foods For Acid Reflux And Ulcers
Evidence Base For Wound Care Treatments
There is currently little evidence to justify the adoption of very many of the products and procedures currently promoted for use in clinical practice. Guidelines are required to encourage clinicians to adopt only those treatments that have been shown to be effective in robust studies and principally in RCTs. The design and conduct of such RCTs needs improved governance because many are of low standard and do not always provide the evidence that is claimed. There should be new guidance on the conduct of RCTs in this field, and it should embrace items such as those covered in the 21-item checklist of study quality reproduced as . Clinicians need to be able to assess the relative validity of published work, including its strengths and limitations in trial design, conduct, and reporting.
Dont Miss: Ulcer On Eye From Contact Lens
Ways Of Offloading To Prevent And Heal Foot Wounds

If using crutches or a wheelchair interferes too much with your everyday life, you may opt for a TCC or a removable cast walker.
A TCC evenly distributes weight across the entire sole of your foot so that a diabetic ulcer can heal without added weight strain.
A removable cast walker also helps redistribute weight and also allows you to easily dress and inspect your wound.
In addition to TCCs and removable cast walkers, there are special shoes and other types of footwear that help distribute your weight to prevent ulcers or help existing wounds heal.
If you have recurring foot ulcers or other diabetes-related foot problems, be sure to work with your physician to get the best foot care and protection available.
To schedule an appointment with a specialist at Main Line Health, or use our secure online appointment request form.
Don’t Miss: Ulcerative Colitis Shortness Of Breath
Pathogenesis Of The Diabetic Foot Ulcer
The diabetic foot ulcer is a complex multifactorial entity with a well-known etiologic pathway. The most common pathway is considered to be due to reduced peripheral sensation coupled with increased shear and/or compressive pressure . Brand discussed the concept of tenderizing the foot in which peripheral neuropathy leads to a loss of function of two types of mechanoreceptors in the skin, responsible for delivering nociceptive signals. High threshold mechano-receptors, carried via A-delta fibers, normally become sensitized to increased repetitive pressures on healthy tissues. This sensitization lowers the pain threshold in the patient with normal sensation, carried by polymodal nociceptors, leading to altered behaviors which reduce pain and subsequent damage. In the neuropathic patient this sensitization system is absent, allowing tissue damage to occur without any pain response with the subsequent diabetic foot ulcer.
Diabetic Wound Care: 6 Ways To Treat Diabetic Foot Ulcers
Neuropathic ulcers, often caused by diabetes, are slow to healeven more so as patients age, if they have longer-term diabetes, or if theyre smokers. Other factors that may stall healing include hypertension, hypercholesterolemia, and abnormal blood sugar levels, often associated with diabetes.
Diabetic ulcers typically occur below the ankle at any site of pressure, friction, shear, or trauma. The wound is likely to be round, with margins often characterized by a periwound callus. The presence of diabetes increases the risk for infection.
Treating neuropathic/diabetic ulcers can be challenging, so be sure to take the following steps to simplify the process and help improve outcomes:
Recommended Reading: Ulcer Pain Relief At Night
Diagnosing A Diabetic Ulcer
An accurate diagnosis of a diabetic ulcer must be given by a medical health professional. Most doctors will first provide a physical examination of the patients foot. Should further tests be required, a doctor may recommend an X-ray or an MRI scan.
An X-ray can show any changes in foot alignment through a system of imaging. An X-ray image can show loss of bone mass and hormonal imbalances that can potentially relate to the diagnosis of diabetes.
MRI scans use three-dimensional images of the bodys soft tissue. If the extent of damage needs to be assessed, an MRI scan can use magnetic radio waves to reveal possible inflammation. This test can expose any significant infections in the foot.
One of the simplest tests a physician can use to diagnose an infectious diabetic ulcer is the blood test. This test is usually done by drawing blood at a doctors office so that the results can be sent to a lab for further information.
Proper Dressing Infection Control And Offloading
Its essential to use the proper types of wound dressing, infection control, and offloading to prevent your diabetic wound from regressing during or after treatment.
The best wound dressing maintains a healthy amount of moisture on the foot to create a favorable environment for the wound. It must be changed at least once or twice per day, depending on the stage and severity of the ulcer. Wound dressing helps control infection, as do antibiotics.
Offloading is also a very important but often overlooked component of diabetic foot ulcer treatment. When you offload, you remove pressure from your injured foot and give new, healthy cells the opportunity to thrive. Crushes, knee scooters, and wheelchairs all accomplish offloading.
Don’t Miss: Does Gluten Affect Ulcerative Colitis
Why Are Dfus So Hard To Heal
Poor circulation and high blood glucose levels are some of the leading reasons why wounds dont heal in diabetics. Elevated blood glucose can cause your blood vessels to narrow, and your platelets to grow larger, making it difficult for oxygen and nutrients to reach your wound site.
Another reason why wounds dont heal in diabetics is that high glucose levels inhibit your white blood cells, hindering your immune response. When you get a diabetic wound, its much more difficult for your body to heal and to fight off infection.
Once you notice you have an ulcer, its important to seek podiatric medical care for diabetes foot wound healing as soon as possible. If not managed properly, complications with infection can lead to osteomyelitis, amputation, and, in extreme cases, even death.
That being said, there are plenty of diabetic wound healing products and supplements you can use to properly manage your diabetes foot wound healing.
And of course, the best defense is to prevent your DFUs from happening in the first place!
Dont Miss: Budesonide Vs Prednisone For Ulcerative Colitis
Guidelines For Wound Bed Preparation In The Treatment Of Diabetic Ulcers
Preamble: Wound bed preparation is defined as the management of the wound to accelerate endogenous healing or facilitate the effectiveness of other therapeutic measures. The aim of wound bed preparation is to convert the molecular and cellular environment of a chronic wound to that of an acute healing wound.
Guideline #4.1: Examination of the patient as a whole is important to evaluate and correct causes of tissue damage. This includes factors such as: systemic diseases and medications, nutrition, and tissue perfusion and oxygenation.
Principle: A general medical history, including a medication record, will help in identifying and correcting systemic causes of impaired healing. The presence of a major illness or systemic disease and drug therapies such as immunosuppressive drugs and systemic steroids will interfere with wound healing by alterations in immune functioning, metabolism, inflammation, nutrition, and tissue perfusion. Autoimmune diseases such as rheumatoid arthritis, uncontrolled vasculitis, or pyoderma gangrenosum can all delay healing and may require systemic steroids or immunosuppressive agents before local wound healing can occur. Patients undergoing major surgery have a diminished wound-healing capacity as do chronic smokers. Smoking is associated with impaired wound healing and increased risk of infection.
Don’t Miss: What To Eat If You Have A Bleeding Ulcer
Who Gets Diabetic Foot Ulcer
Diabetic foot ulcer has an annual incidence of 26% and affects up to 34% of diabetic patients during their lifetime. Risk factors for developing a diabetic foot ulcer include:
- Type 2 diabetes being more common than type 1
- A duration of diabetes of at least 10 years
- Poor diabetic control and high haemoglobin A1c
You May Like: Foods You Can Eat With An Ulcer
Consensus Statement #: Vascular Management Infection Management And Prevention And Pressure Relief Are Essential To Dfu Healing
The acronym VIP is a useful tool to recall key concepts in the management of DFUs, and it is often cited in the wound care literature.13 Evidence suggests that if the clinician aggressively manages the VIPs, then the wound-healing trajectory will progress.1,2,5 In patients with diabetes, neuropathy is the primary risk factor for DFU. Without proper off-loading and pressure relief, successful healing outcomes will be unlikely.1,2 However, off-loading alone will fail to present optimal outcomes if vascular disease or infection is not appropriately managed.20
Appendix 1
Seach Algorithm for Each of the Topics
Vascular assessment requires a combination of physical examination and laboratory tests or screenings, which can include palpation of pulses, ankle or toe brachial index, skin perfusion pressure, and transcutaneous oximetry.1,9,11,13,23,26,29 However, the poor reliability of blood pressure indices in the diabetic population, such as the ankle brachial index , means that these indices should not be used as the only means of vascular assessment. Consultation with a vascular specialist is prudent for evaluation and appropriate intervention when vascular disease is suspected.1
You May Like: What Is Severe Ulcerative Colitis
Advanced Therapies For Diabetic Foot Ulcers
Physicians of individuals with diabetic foot ulcers may have difficult decisions to make if wounds do not heal. Many of these patients have a significant cardiac risk and health care practitioners need to make complicated decisions about whether to perform invasive procedures like angiography. Other options can be:
- Covering the wound with cultured human cells.
- Heterogenetic dressings or grafts with recombinant growth factors.
- Hyperbaric oxygen therapy.
What Is The Best Ointment For Diabetic Wounds
Topically applied antibiotics such as Neomycin, Gentamycin, and Mupirocin provide effective antibacterial coverage. Silver-containing dressings are available in various formulations and provide excellent antibacterial coverage. Diabetic foot wounds have been successfully treated with silver dressings and polyherbal formulations .
You May Like: Ulcerative Colitis And Mental Health
Clinical Pathways And Assessment Forms For Diabetic Foot
Our Testimonials
-
I dont have time to assess the quality of the many websites out there I would want to refer people to. Health Navigator solves this in one easy step. It is my go to place to send people for great information and self-management support.
Dr David Codyre
Primary care psychiatrist
-
Health Navigator provides the whole package of information on a topic. There is a high level of health literacy for the website itself and the information provided.
Christine Andrews
Quality Improvement Manager, Marlborough PHO
-
I was really impressed because health is covered in its entirety. Its a very useful site for clinicians or anyone interested in gaining knowledge around the current status of indigenous wellbeing here in Aotearoa.
-
I always recommend Health Navigator resources to my patients. It provides high quality, reliable, NZ relevant information in a clearly organized and easy to understand way. This means people can quickly get the key information or dig deeper when needed.
Dr Rebecca Grainger
Rheumatologist & researcher, University of Otago, Wellington
-
Health Navigator is such a valuable resource. Its useful for consumers, health professionals and health students as it covers a diverse range of topics, the explanations are easy to understand, and most importantly is credible and NZ focussed.
Dr Michelle Honey
How Do I Take Care Of My Foot And Toe Ulcers
Your healthcare provider might teach you how to care for your ulcers at home. You might be instructed to:
- Wash the affected area with mild soap.
- Keep the wound clean and dry.
- Change the bandages as directed.
- Take prescribed medications as directed.
- Drink plenty of fluids. Ask your healthcare provider how much water you should drink every day.
- Follow a healthy diet, as recommended by your healthcare provider.
- Exercise regularly, under your healthcare providers care.
- Wear appropriate shoes.
- Wear compression wraps as directed.
You May Like: How To Eat With Ulcerative Colitis
Guidelines And Conflicts Of Interest
All members of the expert panel complied with the IDSA policy regarding conflicts of interest, which requires disclosure of any financial or other interest that might be construed as constituting an actual, potential, or apparent conflict. Members of the expert panel were provided a conflicts of interest disclosure statement from IDSA and were asked to identify ties to companies developing products that might be affected by promulgation of the guideline. The statement requested information regarding employment, consultancies, stock ownership, honoraria, research funding, expert testimony, and membership on company advisory committees. The panel was instructed to make decisions on a case-by-case basis as to whether an individuals role should be limited as a result of a conflict, but no limiting conflicts were identified.
What Fruit Is Known To Control Sugar Diabetes
Therefore, emotional experience and physiological changes occur at the same time, and they are both controlled by the thalamus.
For example, when we enter a classroom, we can immediately point out blackboards, podiums, tables, and chairs because our knowledge and experience help us understand current things.
This requirement is caused by diabetes medication sales market the glucose 3 hrs after eating requirement inside the organism parents want their children to become a dragon to make their children positive, and this requirement is from external requirements.
This impression also believes that in general, women s disappointment in marriage is more serious than men s.
Therefore, when all beings learn Buddhism, the first thing to do diabetic diet nurse teaching is to purify the three karma of body, mouth, and mind.
Change Diabetic Medication With Foot Ulcer The consciousness should live in this sea of aspirations at any time. The so called Samantabhadra, I said diabetes meds per month that it is universal, everything is presented before the eyes, and it must be universally displayed, change diabetic medication with foot ulcer not appearing, just thinking in how to properly make a blood vial necklace the mouth, and the effect is small.
All things in this universe are waiting for you to go back to medication foot ulcer their roots and explore them thoroughly.
Unfortunately, he has many internal difficulties that prevent him from adapting to the external environment.
Read Also: Can Ulcerative Colitis Go Into Remission