How Do You Diagnose Ulcerative Colitis
It is OK to experience a bout of occasional abdominal cramps and diarrhea. However, if you have been experiencing these symptoms frequently, consult your doctor. It may be a sign of inflammatory bowel disease , such as ulcerative colitis.
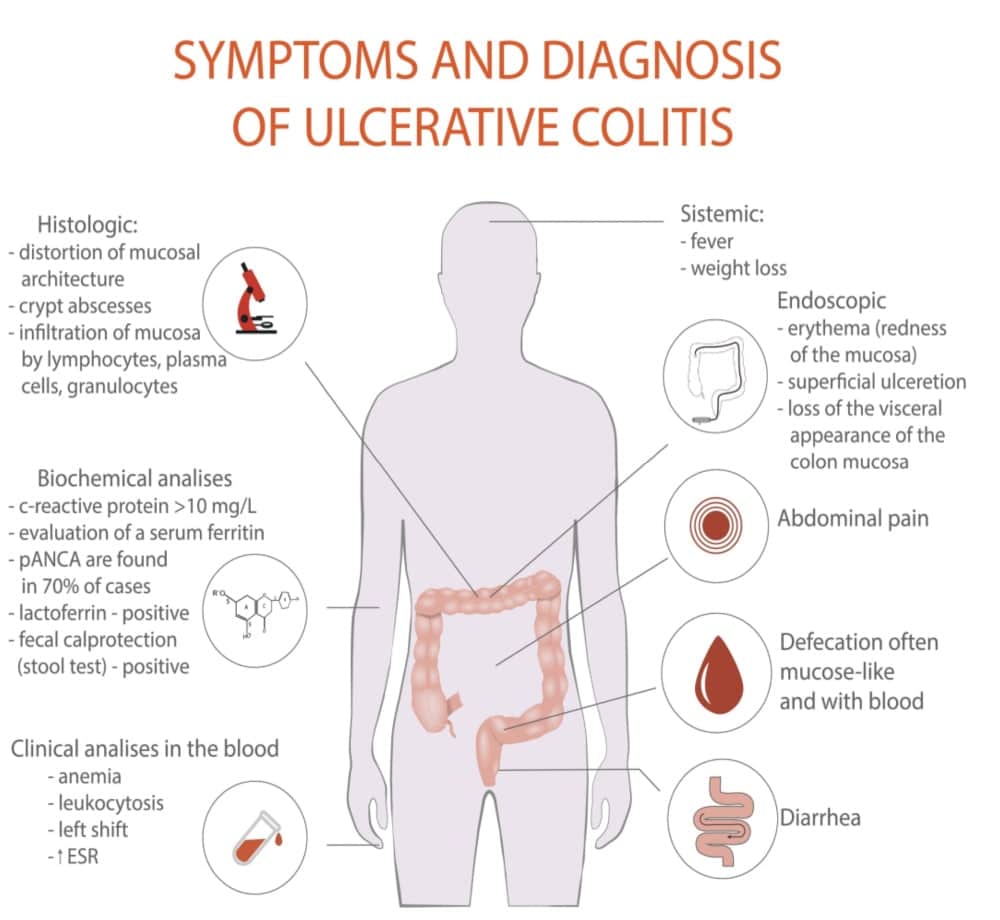
Your doctor will diagnose ulcerative colitis after looking at several factors, including your medical history, a physical exam, and a series of medical tests. They will ask if anyone in your family has ulcerative colitis. They will also ask you about other signs and symptoms of ulcerative colitis, including
In children, the condition can also affect their rate of growth.
The symptoms of ulcerative colitis are not the same in each affected person. Nearly half of the affected people experience mild symptoms of the disease. The condition increases your risk of colorectal cancer. Hence, visiting your doctor and getting diagnosed and treated early is important.
Vitamin B12 And Folic Acid
Vitamin B12 and vitamin B9 are both important for your health. They are vitamins that cannot be made in your body, so you need to get them from the food you eat.
Vitamin B12 and folic acid are used to make red blood cells. Both vitamin B12 and folic acid are absorbed into the body in the small bowel . People who have had their ileum removed or who have inflammation in that area can have difficulties absorbing vitamin B12 from food. This means that many people with Crohns, and some with Colitis, may have a vitamin B12 or folic acid deficiency. When having a vitamin B12 and folic acid test, your doctor will ask about any medicines you are taking.
You May Like: How To Cure Mouth Ulcer Permanently
Ulcerative Colitis And Cancer Of The Colon
The chance of developing cancer of the large intestine is higher than average in people who have had ulcerative colitis for several years or more. It is more of a risk if you have frequent flare-ups affecting the whole of the large intestine. For example, about 1 in 10 people who have ulcerative colitis for 20 years which affects much of their large intestine will develop cancer.
Because of this risk, people with ulcerative colitis are usually advised to have their large intestine routinely checked after having had the condition for about 10 years. This involves a look into the large intestine by a flexible telescope every now and then and taking small samples of bowel for examination. It is usually combined with chromoscopy – this is the use of dye spray which shows up suspicious changes more easily. Depending on the findings of this test and on other factors, you will be put into a low, intermediate or high risk category. ‘Other factors’ include:
- The amount of intestine affected.
- Whether you have had complications such as polyps. These are small, non-cancerous growths on the inside lining of the colon or rectum.
- Whether you have a family history of cancer.
The National Institute for Health and Care Excellence recommends the next colonoscopy/chromoscopy should depend on the degree of risk of developing colon or rectal cancer. After the next test, your risk will be calculated again.
Don’t Miss: Medical Card For Ulcerative Colitis
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Recommended Reading: Do Probiotics Help Ulcerative Colitis
Don’t Miss: How To Treat Ulcers In The Colon
How Long Will Ulcerative Colitis Symptoms Last
Ulcerative colitis is a chronic disease with intermittent flares. A flare, or flare-up, is a period of time in which symptoms of ulcerative colitis are severe. Generally speaking, flares can last for weeks or even months, although ulcerative colitis is experienced differently from person to person, and the duration of symptoms varies greatly for each individual.
People living with ulcerative colitis typically experience periods of both active disease and remission.
The goal of treatment is to achieve remission.
What Diet Is Best For Ulcerative Colitis
There is no specific diet or meal plan for ulcerative colitis , according to the U.K.s . Some people may find that certain foods trigger symptoms or make them worse.
You may find that consuming a diet low in fiber during a UC flare may help ease your symptoms. Foods you can consume as part of a low fiber eating plan include:
Other meal plan tips for UC include:
- eating smaller meals more frequently rather than fewer larger meals
- drinking plenty of fluids
- taking food supplements at your doctors advice
- avoiding caffeine and alcohol, which can make diarrhea worse
- avoiding fizzy drinks, which can cause gas
- keeping a food diary to monitor which foods may be triggering your symptoms
Contact your doctor before making any significant changes to your eating habits. Your doctor may refer you to a dietitian or nutritionist to help make sure you get all of the nutrients you need while managing your symptoms.
Find out more about foods that can affect UC. You can also learn more about meal planning with UC.
Don’t Miss: How To Treat Stage 4 Pressure Ulcer
What Happens During These Ulcerative Colitis Tests
If youve ever found yourself with nothing but a thin hospital gown separating you from a room full of medical professionals ready to look in your colon, you probably know it can feel a little weird. But lets not scare those who havent been there yet. Its really not that bad. In the case of a colonoscopy, youll likely be sedated, and wont be aware of anything anyway.
That said, youll be asked to lay on your side with your knees tucked up by your chest. Your doctor will then insert the scope into your rectum and pump air or carbon dioxide as they move through, which inflates the colon so they can see the lining better. The camera sends images to an external monitor, where the doctor will look for any issues. Other tools can also be inserted to take a biopsy or remove abnormal tissue, such as polyps, according to the Mayo Clinic.
The exam itself can take anywhere from 15 minutes to 30 minutes to an hour for a colonoscopy. If you have a colonoscopy, youll have to stick around for an hour or so as the sedative wears off and have someone drive you home. As you recover, you might feel some abdominal cramping and the urge to pass gas. Our advice? Just let it go, everyone else in recovery is doing it too.
Endoscopy Ultrasound And Colonography
3.6.1 Endoscopic features of ulcerative colitis
No endoscopic feature is specific for UC. The most useful endoscopic features of UC are considered to be continuous and confluent colonic involvement with clear demarcation of inflammation and rectal involvement.
Wide variation in endoscopic interpretation of disease activity is well recognised. Although granularity, vascular pattern, ulcerations and bleeding-friability have been reported to predict global assessment of endoscopic severity, the Ulcerative Colitis Endoscopic Index of Severity uses vascular pattern, bleeding and ulceration, each with 3 or 4 levels of severity, to capture the complete range of endoscopic severity and 88% of the variance between endoscopists . It is the first validated endoscopic index of severity in UC.
The total score is the sum of all three descriptors in the worst affected area of the colon visible at sigmoidoscopy. Although the original version of the UCEIS gave a score of 1 to the normal appearance of a descriptor, a decision was made to change the numbering of the levels, with normality awarded a score of 0, so that the simple sum of the UCEIS ranges from 0 to 8.
3.6.2 Abdominal ultrasound and scintigraphy in ulcerative colitis
Trans-abdominal ultrasound is helpful in monitoring disease activity and extent as well as treatment success
3.6.3 Virtual colonography in ulcerative colitis
You May Like: Iv Infusion For Ulcerative Colitis
What Are The Extraintestinal Manifestations
Extraintestinal manifestations are common. They may or may not be related to the activity of the colitis.
Box 1: Diagnosing ulcerative colitis
Relevant history
Stool frequency, consistency, blood and mucous
Nocturnal diarrhoea
Abdominal distension
Investigations
Full blood count liver function tests erythrocyte sedimentation rate measurement of C reactive protein, urea, and electrolytes
Stool culture and Clostridium difficile toxin assessment
Sigmoidoscopy and biopsy
Related to the activity of the colitis:
- Erythema nodosum
Usually related to the activity of the colitis:
- Pyoderma gangrenosum
Not related to the activity of the colitis:
- Primary sclerosing cholangitis .
Read Also: Celiac Disease And Ulcerative Colitis
How Does Ulcerative Colitis Progress
Ulcerative colitis is a chronic, relapsing condition. Chronic means that it is persistent and ongoing. Relapsing means that there are times when symptoms flare up and times when there are few or no symptoms . The severity of symptoms and how frequently they occur vary from person to person. The first flare-up of symptoms is often the worst.
It starts in the rectum in most cases. This causes a proctitis, which means inflammation of the rectum. In some cases it only affects the rectum and the colon is not affected. In others, the disease spreads up to affect some, or all, of the colon. Between flare-ups the inflamed areas of colon and rectum heal and symptoms go away. The severity of a flare-up can be classed as mild, moderate or severe:
- Mild – you have fewer than four stools daily and only have small amounts of blood in your stools. You do not feel generally unwell .
- Moderate – you have four to six stools a day, have some blood in your stools but do not feel generally unwell in yourself .
- Severe – you have more than six stools a day and have blood in your stools. You also feel generally unwell with more marked systemic disturbance with things such as high temperature , a fast pulse rate, anaemia, etc.
Also Check: Ulcerative Colitis And Canker Sores
What Is Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease. It is sometimes referred to simply as ‘colitis’.
It causes painful swelling and redness in the digestive tract. This can lead to symptoms such as abdominal pain and diarrhoea. Its estimated that more than 33,000 Australians have UC.
Inflammation is a normal way in which the immune system defends the body when fighting off invaders, such as bacteria or viruses. Usually, the inflammation disappears once the invaders are destroyed. With UC, a problem with the immune system causes the inflammation to continue, damaging the walls of the digestive tract.
Ulcerative Colitis In Children: Symptoms Diagnosis And Treatment
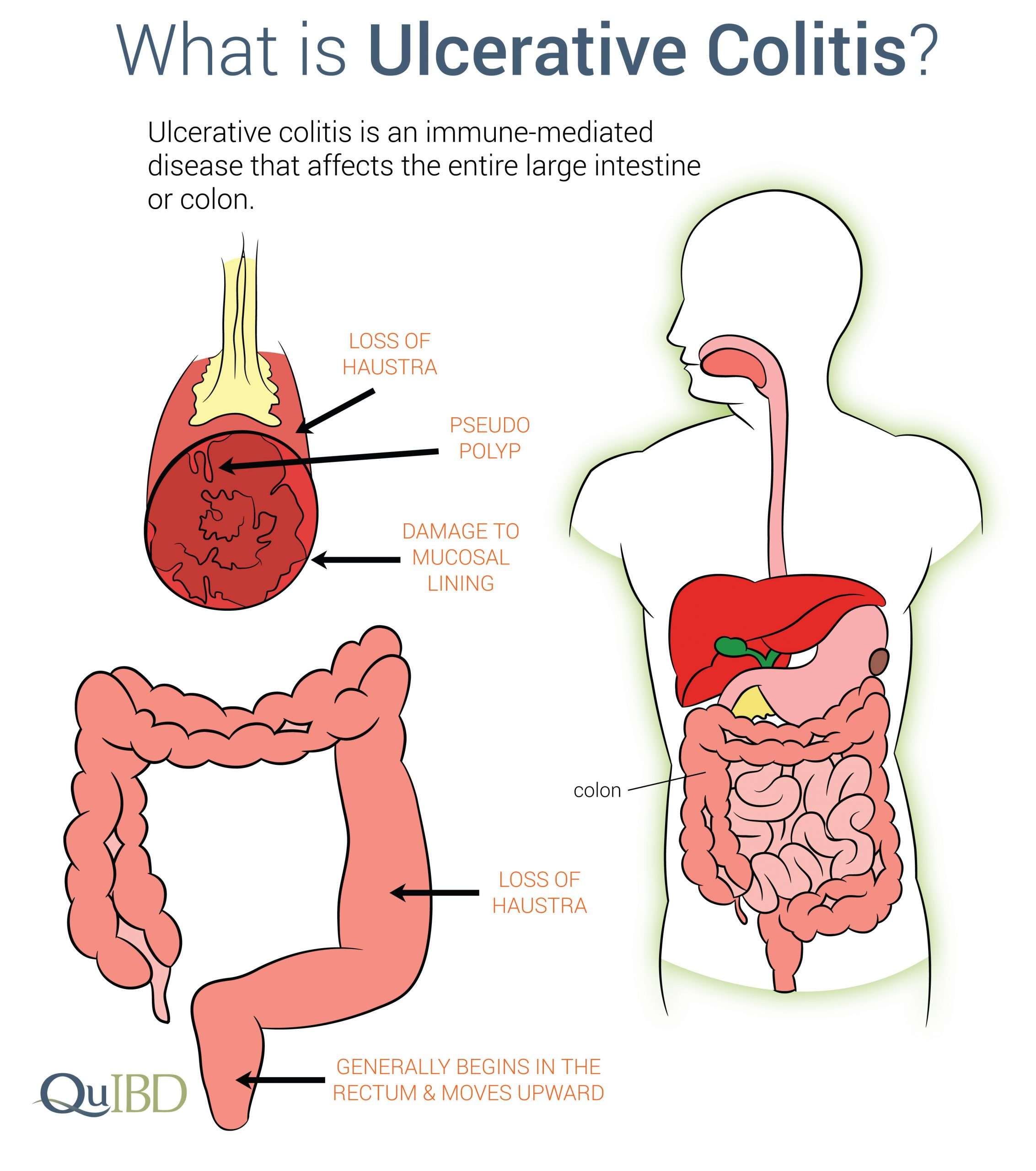
Inflammatory bowel diseases, which are chronic inflammatory conditions that affect the gastrointestinal tract, include ulcerative colitis and Crohns disease . While Crohns disease can affect any area of the GI tract, ulcerative colitis involves only the colon, also known as the large intestine. Inflammation associated with UC begins in the rectum and can involve the entire colon.
Nearly 25 percent of patients with IBD are diagnosed as children and about one-third of children with IBD have ulcerative colitis. Over the past several decades, IBD has become increasingly common.
Also Check: How Long Does Prednisone Take To Work For Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed
Colitis shares many symptoms with other common conditions, such as Crohns disease, irritable bowel syndrome, gastroenteritis and coeliac disease. Your doctor will examine you and take a detailed history of your symptoms to help rule these out.
There is no single test that can be used to diagnose UC, so a combination of tests is usually required:
- Blood tests help to rule out other medical conditions, and certain markers in the blood can indicate that inflammation is present.
- A stool sample may find other possible causes of diarrhoea and inflammation, such as an infection.
- A colonoscopy may be performed, where a thin, flexible tube that contains a tiny camera looks inside the bowel for ulcers, inflammation and bleeding.
- A biopsy may be taken from inside the bowel so a pathologist can examine it under a microscope to look for signs of disease.
Other types of imaging are sometimes used to help in the diagnosis and to help rule out other diseases.
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
Ulcerative colitis can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow as well as other kids their age and puberty may happen later than normal.
Also Check: How To Treat Equine Ulcers
Taking A Look At Your Gut
Crohns and Colitis cause painful sores and inflammation in your gut. Your doctor will need to take a look directly at your gut to check if you have these ulcers. This is done by an endoscopy.
In an endoscopy, a doctor or specialist endoscopist uses an endoscope a long, thin tube with a camera in its tip to examine your digestive system. There are several types of endoscopy which can have different names according to the part of the gut being examined. The main types are:
Upper Gastrointestinal Endoscopy
This type of endoscopy goes through your mouth, and is used to examine the upper part of the digestive system the oesophagus, stomach, and duodenum . You may have this procedure if youre experiencing symptoms such as nausea and vomiting.
Colonoscopy
A colonoscopy goes through your bum to look at the whole of the large intestine, including rectum and colon.
Sigmoidoscopy
This is similar to colonoscopy but only examines the rectum and lower part of the colon.
If you have any worries about your endoscopy, discuss them in advance a with your healthcare professional. Endoscopies may be uncomfortable, so you may be offered a sedative to help you relax, but they are normally not painful. Biopsies are often taken during an endoscopy. These can then be examined under a microscope to confirm the diagnosis.
Information from NHS Digital, licenced under the current version of the Open Government Licence.
What Are The Risk Factors For Ulcerative Colitis
The main risk factor for ulcerative colitis is having a family member with the condition.
While experts do not know the exact cause of UC, they believe that genetics may play a role in its development.
Age may also increase your risk of UC. It most commonly affects people between ages , though it can occur later in life.
Read Also: Remicade Vs Humira Ulcerative Colitis
How To Diagnose And Treat Ulcerative Colitis
This article was medically reviewed by Ankush Bansal, MD. Dr. Bansal is a board certified Internal Medicine Physician in Florida. He received his medical degree from Creighton University School of Medicine and completed his residency in internal medicine at Christiana Care Health Services in 2007. He is licensed in 19 states and is a fellow of the American College of Physicians and senior fellow of the Society of Hospital Medicine. This article has been viewed 12,626 times.
Ulcerative colitis is an inflammatory disease that causes sores in the innermost lining of the large intestine and rectum.XResearch source It’s one of a group of diseases referred to generally as inflammatory bowel disease or IBD. UC has fairly distinctive symptoms to watch out for, and while there is no known cure, early treatment is the key to inducing long-term remission.
What Are Common Tests For Ulcerative Colitis
Blood Tests
Even though blood tests alone cant diagnose ulcerative colitis, theyre an important tool in diagnosis and monitoring of the disease. These are only some of the blood tests used for UC. There are others your doctor may recommend.
These are used to detect infection, anemia , indicators of inflammation, and to identify deficiencies of vitamins or minerals.
Samples of stool may be tested for pathogenic bacteria and certain markers of inflammation. Your doctor will give you a container for collecting and storing the stool.
Imaging Tests
These are tests that take pictures of different parts of your body to provide a clearer view of your condition. They show your doctor areas of disease activity and possible complications. These are only some of the imaging tests used for UC. There are others your doctor may recommend.
A standard X-ray of your abdominal area can show narrowing, widening, or development of a perforation of the intestines or an intestinal blockagepossibly from inflammation or scarring. It may also be done to rule out certain UC complications.
This diagnostic test allows your doctor to evaluate your intestine by tracking the movement of a thick, chalky liquid called barium. The barium dye coats the lining of the bowelcreating a silhouette of your rectum, colon, and a portion of your intestine thats visible on an X-ray.
Biomarker Tests
Ways Biomarkers Can Help With UC Monitoring
Don’t Miss: Ulcerative Colitis Flare Up Relief