Diet For Ulcerative Colitis
Ulcerative colitis is, literally, a pain in the rear: An inflammation of the large intestine and rectum. The symptoms abdominal pain, cramping, diarrhea and bleeding can be debilitating.
And if you have ulcerative colitis, you know that sometimes it flares up, and it often depends on what youve had to eat. Its important to understand that certain foods do not cause ulcerative colitis and the Crohns and Colitis Foundation of America says diet is not a major factor in causing inflammation. However, some colitis sufferers experience issues related to what theyre eating, so its smart to have an Ulcerative Colitis Diet Plan to help control those flare-ups.
Many people do identify some food triggers and these should be avoided if possible, says Crozer Health gastroenterologist Joyann Kroser, M.D. I think patients who keep a food-and-symptoms diary have more insight into what foods may challenge them. Here is a diet plan that works for most ulcerative colitis patients:
Hummus With Pita Chips
This chickpea-based dip packs in a lot of plant-based protein, iron, and folate. Chickpeas are usually well tolerated during ulcerative colitis flares, even though theyre a good source of fiber.
Hummus is also high in healthy unsaturated fat. The right types of dietary fat can help you gain back any weight you might have lost during an ulcerative colitis flare.
You should also avoid high fiber whole-wheat chips if youre in the middle of a flare. Use pretzels or pita chips for dipping instead.
These versatile legumes are loaded with protein, folate, iron, and a type of soluble fiber called raffinose. Bacteria produce the fatty acid butyrate in your digestive tract when they break down this fiber.
Butyrate helps bring down inflammation in the colon. Research suggests that people with inflammatory bowel diseases , like ulcerative colitis, may not produce as much of this gut-healthy fatty acid.
To make this crunchy treat, toss one can of chickpeas in 2 teaspoons of olive oil. Dust with a little bit of garlic powder.
Place the coated chickpeas on an oiled cookie sheet. Brown them in the oven at 350°F for about 45 minutes.
rich in potassium . People with irritable bowel disorders, like ulcerative colitis, are often deficient in this mineral.
Blend one cup of low fat milk with one cup of yogurt, a ripe banana, and ice. Choose a dairy-free alternative if youre sensitive to lactose. Youll get a filling and nutritious snack that you can take with you on the go.
Will Ulcerative Colitis Affect My Stool
Changes in bowel movements are one of the key markers of Ulcerative Colitis. UC stool shape, color, and smell can be quite different than your average bowel movement. If you have Ulcerative Colitis, your immune system essentially attacks healthy cells in your digestive tract, which causes inflammation in your colon and rectum. Below are some key indicators that you may have Ulcerative Colitis based on your stool.
- Color: You might notice bright red, maroon or black color indicating the presence of blood. You may also notice more mucus in the stool than normal.
- Odor: The odor of the stool may be increasingly foul compared to the typical smell.
- Texture: Presence of UC typically causes loose, watery stools. In reference to the Bristol stool chart, UC stool texture will most likely resemble types 5 through 7.
- Frequency: Inflammation can cause increased motility and frequency of bowel movements. Many people experience frequent urgency and diarrhea.
- Effort: People with UC may experience burning or painful stools.
Always consult your primary care doctor. They can refer you to a local GI specialist if needed
If diagnosed, you may want to seek a specialist for your specific disease in your area
Also Check: What Can I Eat When I Have Ulcerative Colitis
Can Surgery Affect Nutritional Status
Some patients need surgery for severe inflammation, strictures, fistulas and abscesses. In Crohns disease, the affected portion of the digestive tract is removed. In ulcerative colitis, the colon is often removed and the ileum may be attached to the anus.
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Read Also: Are Eggs Bad For Ulcerative Colitis
It Can Be Challenging To Differentiate Between Crohns And Uc

Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohns Disease here.
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohns Disease here.
Read Also: What Foods Are Good For Ulcers And Gastritis
Ulcerative Colitis Medications& Surgery
The goal of all ulcerative colitis treatment is to reduce colonic inflammation. The most effective drugs or medicines for this purpose are the salicylates, which are related to aspirin.
When aminosalicylates do not work, corticosteroids are used. A third type of anti-inflammatory drug known as immunomodulators are also used, but it may take weeks or months for these drugs to work.
The latest technology in the treatment of ulcerative colitis is the use of biologic drugs, which target the bodys immune system in order to help heal ulcerative colitis.
Biologic therapy must be given intravenously every few weeks, and involves administering antibodies that are directed at the molecules produced by the immune system that cause inflammation.
Inspired by low incidence of UC in developing countries, there are ongoing clinical studies into the possibility that the pig whipworm may be useful as ulcerative colitis treatment because some scientists theorize that worms in the colon change the immune response and consequently reduce inflammation in the process. 42% of UC patients in one study saw their symptoms improve after eating pig whipworm eggs for three months.
Best And Worst Foods For Ulcerative Colitis
-
Ulcerative colitis is an inflammatory bowel disease that can affect your appetite and the way your body absorbs nutrients. Certain foods seem to trigger uncomfortable symptoms, at least in some individuals. Diet is an important factor in the management of this chronic disease, but theres no one-size-fits-all ulcerative colitis diet. The best and worst foods for ulcerative colitis may depend on whether or not youre experiencing an ulcerative colitis flare. It will take time and experimentation to figure out which foods you can tolerate and which you should avoid.
Recommended Reading: Janus Kinase Inhibitor Ulcerative Colitis
What To Eat With Colitis
Colitis or Inflammatory Bowel Disease is a common disease which can result in discomfort for most of its patients, who experience symptoms such as diarrhea, abdominal pain, flatulence or dehydration. Diet is an essential factor in treating colitis. Not only can it help us to recover but it also means we can avoid having to deal with any of its symptoms. For this reason, at OneHowTo we explain what to eat with colitis.
There are several types of colitis which vary in causes and duration. However in all cases, aside from regular medication, your diet is critical. The types of colitis include:
- Ulcerative colitis causes ulcers in the colon and rectum and may also affect the intestines.
- Infectious colitis is caused an infection and is usually temporary.
- Amoebic colitis is caused by an amoeba parasitic infection.
- Colitis cystica profunda causes polyps to appear on the lower part of the colon.
- Pseudomembranous colitis occurs when the large intestine is infected with clostridium difficile bacteria and it spreads to the colon.
- Ischemic colitis is due to blockage in a colon artery stopping the area from getting enough oxygen.
- Idiopathic colitis has no known causes.
To avoid diarrhea, abdominal pain, flatulence and general discomfort, we have to watch what we eat. As for protein and dairy, for a colitis diet we must:
Do Any Medications Have Nutritional Side Effects
Moderate to severe flares of IBD are often treated with corticosteroids , cholestyramine and 5-ASA compounds . These medications have nutritional side effects that should be addressed. If you use any of these medications, talk to your doctor or registered dietitian for treatment advice.
- Prednisone causes decreased absorption of calcium and phosphorus from the small intestine. It also causes increased losses of calcium, zinc, potassium and vitamin C. With continual use of high doses of prednisone, the result may be bone loss and development of bone disease. People on prednisone may need up to 1200 milligrams a day. Protein needs also are increased for people taking prednisone because it increases protein breakdown in the body.
- Cholestyramine decreases absorption of fat-soluble vitamins , as well as folate, vitamin B-12, calcium and iron.
- Sulfasalazine interferes with folate absorption. People taking this drug also should take a 1 milligram folate supplement each day.
Read Also: How To Use Aloe Vera Gel For Ulcerative Colitis
Recommended Reading: How To Manage Ulcerative Colitis Pain
What To Eat During Flare
Low-fiber foods are easiest to digest and are less irritating to the gut, especially with symptoms like abdominal pain or diarrhea. Choose:
- Grains/starches: White foods, instead of wheat or whole-grain, and those with less than 2 grams of fiber per serving
- Cooked vegetables: Well-cooked vegetables such as green beans, carrots, mashed potatoes without skin, steamed asparagus tips and pureed squash.Use fresh or frozen.
- Canned or soft fruits: Peeled apples, ripe bananas, cantaloupe, honeydew, watermelon, and canned fruit in fruit juice or light syrup
Be sure to eat enough protein — Inflammation causes increased protein needs. Choose:
- Tender, well-cooked meats: Poultry, salmon or other fish, lean beef and pork prepared without added fat
- Deli meats: Low-sodium and low-fat varieties
- Eggs: Well-cooked
- Tofu
- Smooth nut and seed butters: Peanut, almond or sunflower seed
Drink plenty of fluids — Aim for eight cups a day, and consider using oral rehydration beverages as needed. Try to limit caffeinated, sugar drinks and beverages made with sugar substitutes.
Limit added fats and oils — Focus on oils instead of solid fats, and limit intake to less than eight teaspoons per day.
Consume adequate calcium, vitamin D, probiotics, and prebiotics — Sources include:
Should I Take Extra Vitamins And Minerals
Yes, you should take a complete multivitamin with minerals.
If you take steroids or limit your intake of dairy products, you should also take extra calcium and vitamin D .
If you are take sulfasalazine you may need to take folic acid.
Iron and vitamin B12 deficiencies are common with IBD, so you may need to have blood tests to measure these nutrients.
With prolonged diarrhea, you may also need magnesium, zinc and potassium supplements. An electrolyte drink, such as Drip Drop, may help add these nutrients back into your body.
Check with your doctor if you are concerned about your nutrition.
Recommended Reading: Indian Recipes For Ulcerative Colitis Diet
Spinach Artichoke Yogurt Dip
This easy-to-make dip will help you sneak in your daily veggie servings. Artichokes are a low fiber food thats generally safe for people with ulcerative colitis. Theyre also a prebiotic. That means they feed the good bacteria in the gut and may support colonic health.
Combine one can of artichoke hearts and a package of chopped spinach with low fat yogurt and shredded cheddar cheese.
Pour the mixture into a casserole dish. Then bake at 350°F for 20 to 25 minutes. Serve with sliced carrots and cucumbers for dipping.
What Foods Should I Not Eat When I Am Having An Ulcerative Colitis Flare
Certain foods can exacerbate or aggravate an UC flare and should be avoided. They are more likely to trigger cramping, bloating, and/or diarrhea and are also not recommended in people diagnosed with a stricture, which is a narrowing of the intestine caused by inflammation or scar tissue, or in those who have had recent surgery. Examples include:
- Foods high in insoluble fiber that are hard to digest, such as seeds, raw green vegetables , whole nuts, whole grains, or fruits with a skin
- Lactose, which is milk sugar found in dairy products, milk, cream, cream cheese, and soft cheeses
- Non-absorbable sugars such as sorbitol, mannitol, and other sugar alcohols that are typically found in sugar-free gum, candy, ice cream, and certain types of fruits and juices such as pear, peach, and prune juice
- Sugary foods such as candy, pastries, and juices
- High-fat foods such as butter or margarine, coconut oil, or fatty, fried, or greasy food
- Spicy foods
- Alcohol such as beer, wine, or spirits
- Caffeinated drinks such as coffee or energy drinks
- Soda.
Don’t Miss: Managing Ulcerative Colitis Flare Ups
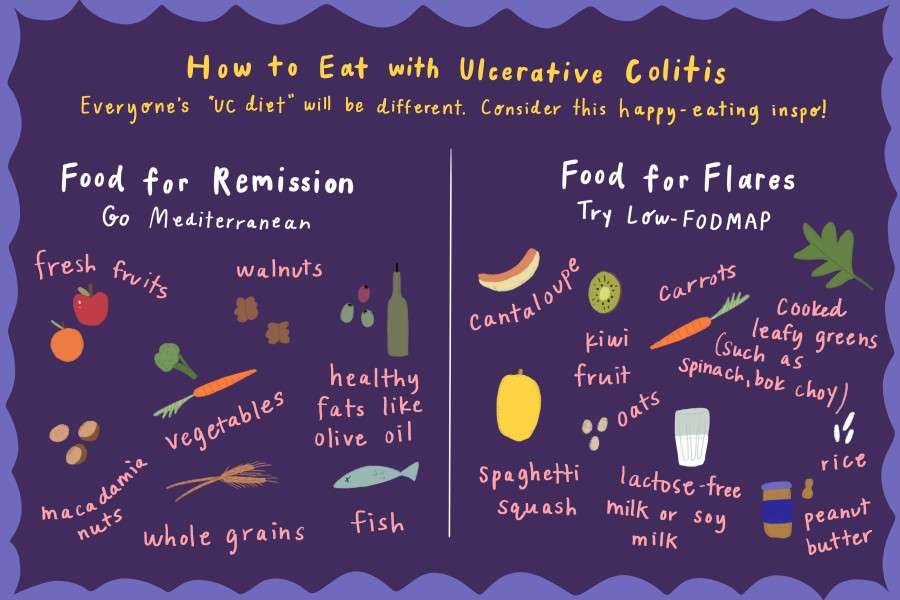
Choose Low Fodmap During A Flare
The Med diet is super healthy, but during a flare, the low Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols diet is your friend. Low-FODMAP plans reduce short-chain carbohydrates and sugar alcohols that spell trouble for UC sufferers. “This diet limits carbohydrates that are poorly absorbed and highly fermentable by the gut microbiota,” says Warren.
Ulcerative Colitis Diets You Might Try
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
You May Like: Histiocytic Ulcerative Colitis Boxer Treatment
Eating With A Stricture
If you have a stricture , you may need to change what you eat to help prevent the intestine getting blocked.You might be advised to avoid foods that could block the intestine, such as:
If you have a severe stricture, you may only be able to eat very soft or liquid foods.Its important to speak to a dietitian to make sure youre eating a healthy, balanced diet. In some cases, they may recommend a vitamin and mineral supplement.
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient.
Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitislose weight and can develop signs of malnutrition. A high-calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAP stands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have an intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
You May Like: Drinking Alcohol With Ulcerative Colitis
Inflammatory Bowel Disease Diet Guidelines
Inflammatory bowel disease is a term used to describe two diseases that cause the gastrointestinal tract to become inflamed: Crohns disease and ulcerative colitis. Both can cause sores or ulcers to occur in the GI tract. This may affect how the body is able to absorb food or make it hard or painful to eat.
Tips For Meal Prepping
Now that you have a sense of what to eat for ulcerative colitis, its time to get in the kitchen. Meal prepping some simple ingredients can make your life easier and prevent a UC flare. Here are some simple strategies:
- Buy pre-chopped fruits and veggies. Having produce in your fridge that dont require any preparation will make you more likely to add them to your plate at mealtime.
- Go frozen. Frozen fruits, veggies, and whole grains are generally as nutritious as fresh produce. Buy frozen fruit for smoothies, frozen veggies for soups and casseroles, and frozen grains to heat up in the microwave as a side dish.
- Pick up ready-made proteins. Stock up on simple options, like a rotisserie chicken or canned beans.
- Make a big batch of soup. Not only is soup soothing, its also an easy way to add a ton of veggies to your diet and is super easy to make in big batches.
- Stock up on healthy fats. Load up your cabinet with nuts, oils, and seeds for snacking, cooking, or adding texture to a recipe.
You May Like: Natural Ways To Heal Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.