Check Out Some Relatable Situations And How To Deal With Them
Everyday struggles can come with having ulcerative colitis like socializing or traveling. But the best way to navigate life with UC is to seek an effective treatment plan. Beyond that, its helpful to maintain a hopeful outlook, healthy lifestyle, and strong support networkand strive to lead a full life.
What Is Ulcerative Colitis
This chronic inflammatory bowel disease causes unpredictable diarrhea and pain in the abdomen. Other common symptoms include: urgent and frequent bowel movements, bloody stool, abdominal pain, nausea and vomiting, and weight loss. You may have periods with no symptoms, and then suddenly, the pain and trips to the bathroom return.
Sometimes remission can last for weeks, months, or even years.
Once you receive a confirmed diagnosis by Digestive Health Services, proper treatment can begin which should give you some relief from this condition.
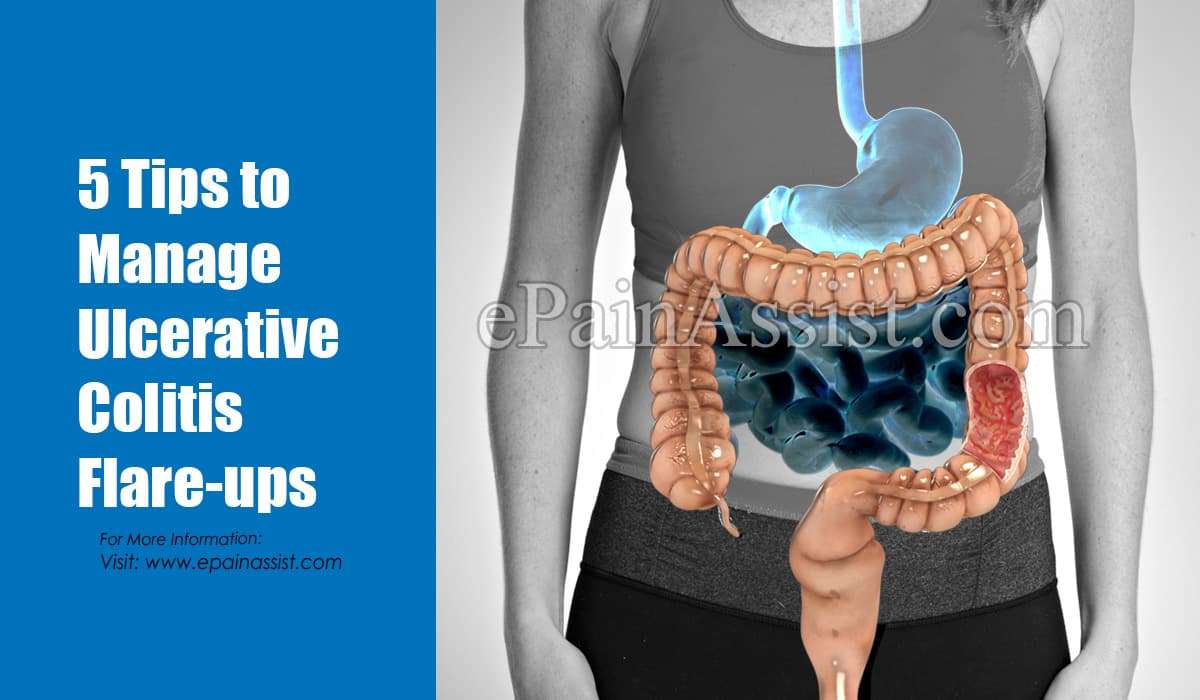
Tips For Managing Ulcerative Colitis Symptoms
- Consult your healthcare provider or dietitian before making any changes to your diet
- Eat a well-balanced nutrient rich diet
- Eat more frequently. Eat five to six smaller meals over the course of a day
- Stay hydrated by drinking water and fluids with salt like broth, tomato juice or rehydration solutions
- Drink slowly and avoid using a straw because these may cause gas due to taking in air
- Use a food diary to record the foods you eat and how these impact your symptoms
- Avoid your specific trigger foods
- Use simple cooking methods boil, steam, grill, poach, broil or saute
Also Check: What Are The 4 Stages Of Pressure Ulcers
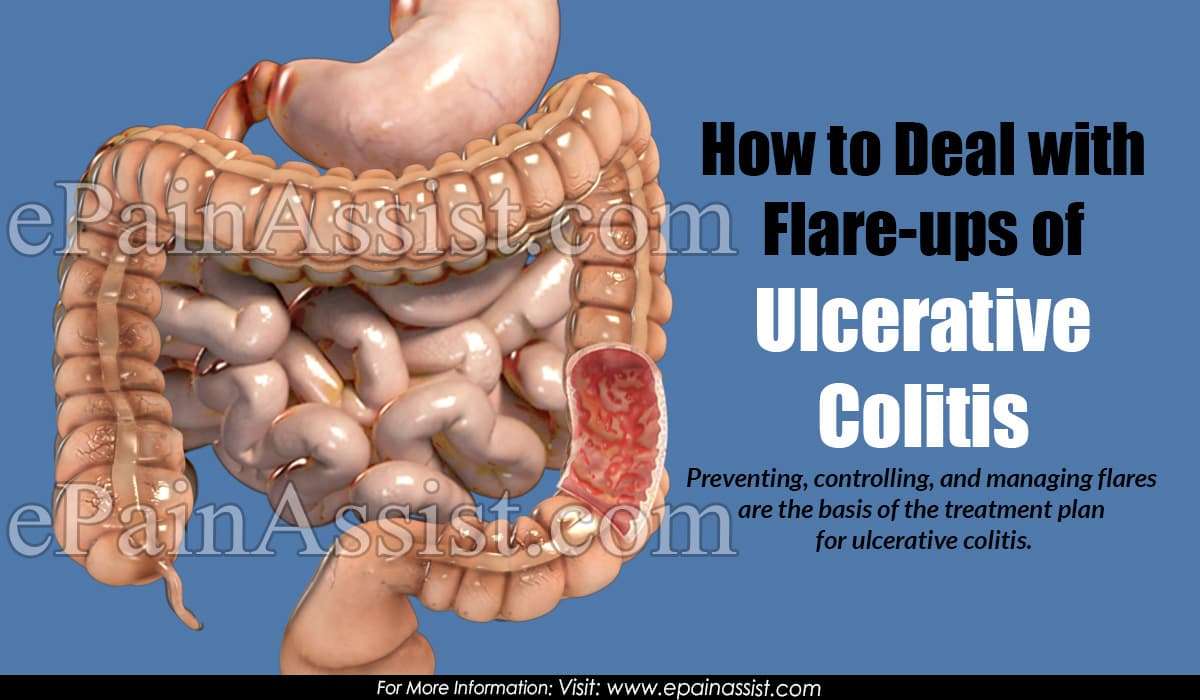
How To Calm An Ulcerative Colitis Flare
This article was co-authored by Peter Gardner, MD. Peter W. Gardner, MD is a board certified physician who has practiced Gastroenterology and Hepatology for over 30 years. He specializes in diseases of the digestive system and liver. Dr. Gardner earned his Bachelors degree from the University of North Carolina and attended Georgetown Medical School. He completed his residency in Internal Medicine and then his fellowship in Gastroenterology at the University of Connecticut. He is a previous Chief of Gastroenterology at Stamford Hospital and remains on the staff. He is also on the staff of Greenwich Hospital and New York Presbyterian Hospital. Dr. Gardner is an Approved Consultant in Internal Medicine and Gastroenterology with the American Board of Internal Medicine.There are 8 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 9,951 times.
Find Ways To Chill Out
All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
You May Like: What Is Good For Mouth Ulcers
Make Sure Youre Getting Enough Probiotics And Prebiotics
Whether you take probiotics tablets, eat fermented vegetables or other fermented products, or take kefir, I personally try to intake something with probiotics and prebiotics at least a few times a week. My personal favourite is a kefir smoothie its an excellent combination of probiotics and prebiotics! Learn more about how to choose the right probiotics here.
Make Less Stress A Priority
Another way to help prevent a flare or intercept one thats already begun? Destress. Theres a lot of research on the role of stress in this condition, Dr. Farhadi says. Like a recent study in Frontiers in Pediatrics where researchers found that stress might promote relapses in inflammatory bowel disease . In a stressful moment, have in mind that all measures to manage stress are very important, he says. He recommends finding your own best way to manage stress. The next slides offer a few options to try.
Don’t Miss: What Is The First Sign Of Stomach Ulcer
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with ulcerative colitis and their loved ones. On MyCrohnsAndColitisTeam, more than 138,000 members come together to ask questions, give advice, and share their stories with others who understand life with ulcerative colitis.
Are you living with ulcerative colitis pain? What has helped you to manage it? Share your experience in the comments below, or start a conversation by posting on your Activities page.
You May Like: Low Dose Naltrexone Ulcerative Colitis
Alternative Treatments For Managing Ulcerative Colitis Flare
Some people with ulcerative colitis feel better when they are on fish oil, probiotics, and herbal supplements. Alternative treatments such as acupuncture also work for some.
Some studies have investigated the impact of various formulations of cannabis on inflammation in IBD. Formulations of cannabis products can include CBD only, CBD with THC at various percentages, and THC alone. Cannabis was found to be effective in reducing symptoms of IBD, such as diarrhea and abdominal pain, but not in controlling inflammation associated with IBD.
Read MyCrohnsAndColitisTeams interview with Dr. Kinnucan to find out more about CBD oil and cannabis for IBD here.
Don’t Miss: How To Treat Sacral Pressure Ulcer
Common Triggers Of Ulcerative Colitis Flare
The symptoms of ulcerative colitis flare-up are not pleasant and often force people to retreat socially. They fear being too far away from a washroom. How long do colitis flare-ups last? Ulcerative colitis flare-up duration can be a few days or several weeks. Sometimes, it depends on the trigger.
Here are some common triggers of the disease:
- Hormone fluctuations during pregnancy
- Caffeine
- Stress
Understanding the triggers and knowing how to stop a colitis flare-up gives those who are diagnosed with the disease the confidence to enjoy normal activities, including a full social life.
Understand That Flares Happen
UC flare prevention didnt work? That happens, says Rudolph A. Bedford, M.D., a gastroenterologist at Providence Saint Johns Health Center in Santa Monica, CA. Sometimes, quite frankly, youre going to flare no matter what we do, and no matter whats happening, he points out. UC is an autoimmune disease, meaning the bodys immune system is attacking the large intestine. We dont know all the reasons why this happens, so sometimes flares can surprise us at any time, for seemingly no cause. Making peace with this can be helpful, as well as being proactive about seeking treatment to relieve symptoms.
Also Check: What Foods Should I Avoid With A Stomach Ulcer
How Long Do Flare
UC is a condition that is unique to every individual. Some people experience flare-ups that last a few days, while others experience flare-ups that last weeks. Likewise, individuals may go from a mild flare-up to a severe one and then back again.
If a person is experiencing a severe flare-up that persists, they should speak with a doctor. The doctor will help them get their symptoms under control and improve their quality of life.
He Had Recurring Pain For Nearly A Decade
- Read in app
The pain woke the 52-year-old physician from a dead sleep. It was as if all the muscles in his right leg, from those in the buttock down his thigh to the very bottom of his calf, were on fire. He shifted slightly to see if he could find a more comfortable position. There was a jag of pain, and he almost cried out. He glanced at the clock: 4 a.m. In just three hours he would have to get up. He had a full day of patients to see. Massage didnt help. He couldnt get comfortable lying flat, so finally he moved to the living room, to a recliner. Only then, and only by lying completely still, did he manage to get the pain to abate. He drifted off, but never for long. The searing pain in his leg and buttock slowly eased, and by the time his alarm went off, he could stand and walk though his muscles still ached and he had to baby his right leg, causing a limp.
Between patients, he arranged to see his own doctor. Hed had pain off and on in his buttocks, one side or the other, for more than a year. The pain was in the middle of each cheek and was worse when he was sitting and at the end of the day. Walking to and from his car on the way home was brutal. And then, as mysteriously as it came, it would disappear only to come back a week or two later.
Read Also: Can I Eat Eggs With Ulcerative Colitis
Ways To Manage Symptoms And Flares Of Ulcerative Colitis
A flare of ulcerative colitis can be painful and embarrassing not only for you, but for those around you. Once you have one flare, are you going to have more? That anxiety can make you feel even worse and trigger one. Lets investigate 6 ways to manage symptoms and flares of ulcerative colitis.
Stress Anxiety And Depression
As with many chronic health conditions, UC can take a toll on mental health. This stress can, in turn, worsen UC symptoms and lead to flares. Studies have found that stress triggers a series of reactions in the body that suppress the immune system, causing inflammation of the intestines. Additionally, stressful emotions, such as anxiety and depression, have been found to cause abdominal pain in people with IBD.
Flare-ups can be exacerbated in the setting of recent life stressors, such as the loss of a job, Dr. Kinnucan said. Anxiety and depression can contribute to an increase in clinical symptoms in people with IBD, and may worsen quality of life, she added. It is important to address symptoms of anxiety or depression with your health care provider.
Don’t Miss: Best Medicine For Stomach Ulcer Pain
Bottom Line On Uc Pain Relief
You may be battling UC pain today but that by no means predicts your future. Complete remission should be a shared goal between you and your doctor. It may take patience to find the best treatment but living your life without UC pain is an achievable goal.
Pain Prevalence:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
Over the Counter Medications: Mayo Clinic. Ulcerative Colitis.
How Imodium Works: Imodium. How IMODIUM Products Work.
How Tylenol Works: Tylenol. What Is Acetaminophen?
NSAIDs: Therapeutic Advances in Gastroenterology. Pain Management in Patients With Inflammatory Bowel Disease: Insights for the Clinician.
Prescription Medications:Journal of Crohns & Colitis. Upadacitinib Treatment Improves Symptoms of Bowel Urgency and Abdominal Pain, and Correlates With Quality of Life Improvements in Patients With Moderate to Severe Ulcerative Colitis.
You May Like: Vitamin E And Ulcerative Colitis
Find Your Support System
MyCrohnsAndColitisTeam is a community of more than 138,000 members who understand living with inflammatory bowel disease. Members share tips for managing flares and offer each other support and encouragement.
Do you struggle with UC flares? What has worked for you? Share your tips in the comments below, or on MyCrohnsAndColitisTeam.
You May Like: What Is The Best Treatment For Ulcerative Proctitis
Manage Symptoms Of Ulcerative Colitis Flare
How to deal with colitis flare-up can be approached different ways. Some people have reported that herbal remedies help manage their symptoms. Probiotics, the spice turmeric, and the herb boswellia have been used to control ulcerative colitis. Studies have also shown that gingko biloba has been effective in treating colitis in rodents.
Since stress has been linked to the disease, exercises like yoga and meditation are often recommended to patients. At the same time, certain foods have a higher chance of aggravating those who suffer from ulcerative colitis, so obviously avoiding such food items is a good idea. Some examples of foods to stay away from are, whole-grain bread, whole-grain pasta, beans, raw vegetables, and dried fruit. Keeping a diary of what you eat can often help you pinpoint what causes a flare-up.
A diary or journal can also help when you are taking medications. For example, if you experience a flare-up while taking an over-the-counter medication, discuss an alternative with your doctor and/or pharmacist.
When it comes to controlling ulcerative colitis flare-up, it can take time. Some people will have multiple triggers and wont be able to make all the necessary lifestyle adjustments all at once. Sometimes, just a few changes can make a huge difference though. The following simple steps have proved to help many people tame their flare-ups:
Dont Skip Your Medication
If you already have prescription medication for colitis, take your medication as prescribed. Dont skip your medicine, even if you feel better.
If you need help remembering to take your medication, use a reminder on your phone and/or set a sticky note on your keys
Sticking with your medication schedule can help you stay in remission and avoid a flare-up.
Also Check: Is Burping A Sign Of An Ulcer
How To Reduce Ulcerative Colitis
Without treatment, people with UC tend to relapse.
For many people with mild or moderate symptoms, things improve somewhat after diagnosis. This is thanks to medication, along with identifying and avoiding triggers.
More aggressive cases are less common, and only a small number of severe cases will require hospitalization.
Repeated flare-ups can indicate problems with your current treatment, so speak with your doctor and discuss adjusting your medication.
Several classes of medication now exist that can help you get into and stay in remission. Your doctor may need to add another type or increase your dosage.
The only way to prevent UC flare-ups is to have surgery. The most common type of UC surgery is the proctocolectomy, which involves the removal of the rectum and colon.
Candidates for UC surgery include people who:
- have sudden or severe disease
- have a perforated colon
- are at risk for colorectal cancer
- are unable to tolerate their UC medications due to side effects
- have stopped responding to their UC medications
In addition to knowing how to manage flare-ups, its also helpful to recognize factors that can trigger your flare-ups.
Read Also: In Order To Prevent Pressure Ulcers
Contact Your Doctor At The First Sign Of A Flare

You should contact your doctor if you think you are experiencing a flare so he or she can test to see if the flare is due to an infection, or determine if any new medications or exposures, such as recent antibiotics, might have triggered the flare. In the absence of infection or another reversible cause of the flare, your gastroenterologist may recommend a treatment course of corticosteroids, either topical or systemic .
Symptom flares can also indicate a change in your bodys response to your current treatment. For example, each year a portion of patients who take either immunomodulator or biologic medications such as infliximab or adalimumab stop responding to their medication. Sometimes a major symptom flare can signify that these medications are no longer working. Your doctor can perform tests to confirm if this is the case and, if necessary, switch you to a different medication.
Don’t Miss: Foods To Eat To Heal Stomach Ulcers
Even On Good Days Take Your Meds
It can be easy to forget to take your medicines when you feel good. Or you might think it’s OK to skip them because you feel fine. But you need to stick with the plan your doctor prescribed to keep up those benefits.
You and your doctor will work together to decide if you need to stay on medicines to control your UC. The type of medicine will depend on how severe your UC is.
How Can You Get Tested For Ulcerative Colitis
Someone can visit a clinic like the new Digestive Health Centre at OneWelbeck in London, meet with a specialist, and have tests carried out to provide a clear diagnosis.
For patients who already know that they have ulcerative colitis, it is possible to have your history reviewed and some diagnostic procedures carried out to see if any treatment options may be of benefit.
Don’t Miss: How To Ease Stomach Ulcer Pain
When To Call Your Doctor About A Flare
Flares come with different levels of intensity. You may be able to manage a mild flare-up of symptoms on your own. But a more severe flare may be a warning sign of an ulcerative colitis complication that needs immediate attention.
Theodore J. Saclarides, MD, a colon and rectal surgeon at Rush University Medical Group in Chicago, suggests calling your doctor if you have any of these ulcerative colitis symptoms:
- Severe abdominal pain that lasts more than 24 hours
- A decrease in bowel movements along with abdominal pain
- Abdominal pain with a high fever
- Blood during a bowel movement that is too thick to see through
What Are The Symptoms Of A Flare
When you start to have a flare-up, you may experience a variety of symptoms. These can include:
- Stomach pain
- Redness on the skin and some swelling
- Eye irritation
Are these symptoms a definite sign someone has a flare of ulcerative colitis?
No. These symptoms overlap with other gastrointestinal conditions such as ulcerative colitis or Crohns disease. You can read more on the difference between ulcerative colitis and Crohns disease on our Inflammatory Bowel Disease page.
Can a flare-up be serious?
The vast majority of flare ups can be managed at home with medication meaning it is rare to need hospital admission. However, if someone gets a fever or severe abdominal pain, or excessive bleeding then they should attend either their Dr surgery or see their specialist.
Don’t Miss: Can You Develop Ulcerative Colitis