When To Use Mepilex Border Sacrum
Treatment
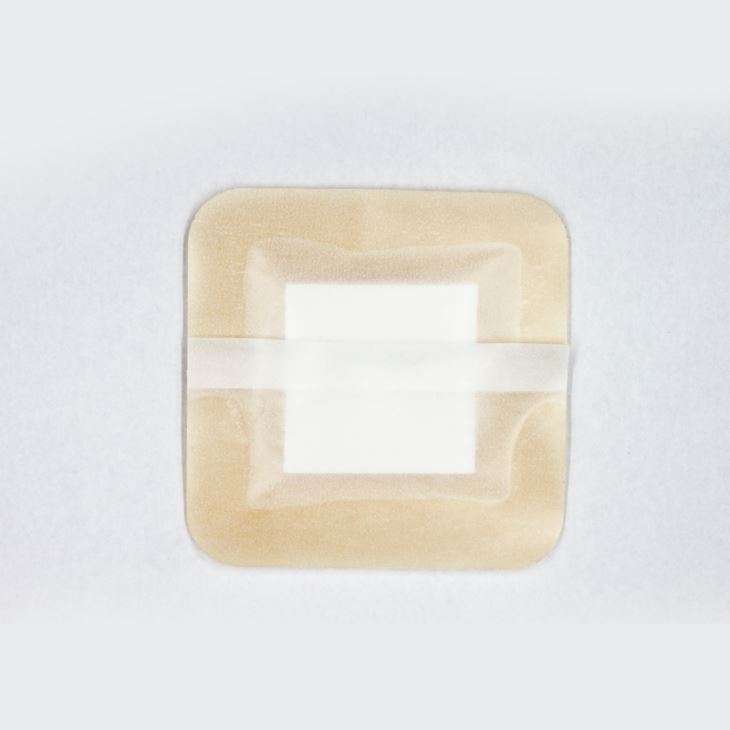
Use Mepilex Border Sacrum for medium-to-high exuding sacral wounds, such as pressure ulcers or surgical excision of pilonidal cysts. The dressing maintains a moist wound environment, which supports debridement, so you might see an initial increase in the wound size. This is normal and to be expected.
Pressure ulcer prevention
A recent randomised controlled trial in the USA revealed a statistically significant effect of Mepilex Border Sacrum in reducing the incidence of hospital acquired pressure ulcers by 88% You can apply the dressing prophylactically for at risk patients , such as the immobile, those with poor skin perfusion and impaired skin condition, in emergency rooms, in intensive care, or before and during long surgical interventions. Scientific studies have demonstrated that Mepilex Border Sacrum has the ability to impact on four extrinsic factors that can contribute to developing pressure ulcers: by minimising and redistributing shear, redistributing pressure, reducing friction, and maintaining an optimal microclimate .
Note: the use of dressings as part of a prophylactic therapy does not preclude the need to continue to develop and follow a comprehensive pressure ulcer prevention protocol.
Pressure Ulcer Prevention And Treatment: Use Of Prophylactic Dressings
Accepted for publication 5 March 2015
11 October 2016Volume 2016:3 Pages 117121
Kathleen Reid,1 Elizabeth A Ayello,2 Afsaneh Alavi,3
Introduction
Pressure ulcers are a major cause of mortality, morbidity, patient suffering, and cost on the health care system worldwide. The management of pressure ulcers is a compounding challenge to health care professionals across disciplines. Individuals who acquire pressure ulcers often require long-term interventions, representing a large economic burden to the health care system. It has been estimated that in Australia, these injuries increase the length of hospital stay and subsequently incur $285 million in cost annually.1 Since 2008, the Centers for Medicare and Medicaid Services no longer reimburses American hospitals at a higher rate for any pressure ulcer that occurs during a patients hospitalization, which provides a strong financial stimulus for pressure ulcer prevention protocols to be implemented.2 Indeed, the profound impact of pressure ulcers on the emotional, physical, mental, and social domains of life has been shown in different studies.3 Current management strategies target pressure-relieving surfaces: patient repositioning, nutritional support, and application of protective dressings to prevent pressure injuries. Dressings are accessible and easily implemented devices however, they can also contribute to high health care costs. Therefore, it is important to evaluate their efficacy.
Prophylactic role of dressings
Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
Anatomy of Normal Skin
What is a Pressure Ulcer?
There are many contributing factors.
Recommended Reading: Yea Sacc For Horses With Ulcers
Proper Foam Dressing Application Instructions
The procedure for applying a foam dressing is as follows:
The flexibility of foam dressings allows for a wide variety of clinical applications with wounds that have from moderate to heavy exudate. Because they are easy to use and can be easily cut to fit irregular wound areas, they are a good dressing choice for many situations.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of IncontinenceSource, Kestrel Health Information, Inc., its affiliates, or subsidiary companies.
Setting And Eligibility Criteria
This study will recruit patients who receive primary health assistance, including patients able to attend the primary health center or receive health assistance in homes, nursing-homes and non-acute long term hospitalization centers. Each patient must present with at least one PrU-II.
Inclusion criteria
-
Age18 years.
-
Confirmed diagnosis of PrU-II. If a patient has more than one PrU-II, only the largest diameter ulcer will be assessed. Other PrU-II will receive the best treatment elected by the study nurse.
Exclusion criteria
-
Stage I, III or IV PrU only.
-
Non classifiable PrU.
-
Surgical treatment prior to PrU and/or PrU in previously irradiated areas.
-
Participation in another clinical trial within 3 months of study entry.
-
Allergy or hypersensitivity to materials in the study dressings.
-
Signs of PrU basal infection , cellulitis or osteomyelitis. Patients successfully treated for infection can be included if the PrU can be classified as stage II.
-
Venous ulcers and/or diabetic feet.
-
Type I diabetes.
-
Situations of extreme severity and/or agony e.g. patients in terminal phase with < 3 points on the Braden scale and/or a life expectancy< 1 month.
Also Check: L Glutamine Ulcerative Colitis Dosage
Why It Is Important To Do This Review
Pressure ulcers are a relatively common yet complex type of wound that are a significant source of suffering for patients and their loved ones and an economic burden to healthcare systems . They are an internationally recognised patient safety problem and serve as a clinical indicator for the standard of care provided. As a result, significant investment has been made in strategies aimed at pressure ulcer prevention. However, pressure ulcers remain a prevalent condition in many care settings. Dressings are widely used as a treatment strategy for pressure ulcers, and understanding the existing evidence base and potential uncertainty around clinical efficacy and costeffectiveness of different dressing types is important for effective decision making.
Internationally accepted guidelines recommend that dressings that keep the wound moist should be used, based upon level C evidence that is “supported by indirect evidence and/or expert opinion” . The same guidelines suggest that foam dressings be used to treat pressure ulcers in various scenarios, mainly for the treatment of exuding Category/Stage II and shallow Category/Stage III pressure ulcers, however these recommendations are based on limited evidence .
Key Challenges And Learning Points
The key challenges faced by the EAC and the company were the issues with generalisability and uncertainty surrounding the clinical evidence. Although a reasonable body of evidence exists for Mepilex Border dressings, all of the clinical trials were conducted outside of a UK setting. This raised uncertainty around whether the evidence from these trials could be generalised to the UK NHS, due to potential differences in standard care pressure ulcer prevention protocols and the baseline incidence rate of pressure ulcers. Standard care prevention protocols were not always clear in the reporting of each of the clinical trials, although in cases where they were clear, it was judged that they were consistent with standard care in the UK. Expert advice and the existence of national prevention guidelines further supported the idea that the comparator in the trials was well matched to the decision problem . The baseline incidence of pressure ulcers estimated for the UK NHS setting by the EAC was also well aligned with the three RCTs on which the meta-analysis was based, and therefore, the scope to benefit from Mepilex Border dressings was judged to be broadly similar in a UK NHS setting.
Also Check: Symptoms Of Ulcer In Female
Silicone Adhesive Multilayer Foam Dressings To Prevent Pressure Ulcer
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| First Posted : February 22, 2018Results First Posted : April 26, 2021Last Update Posted : April 26, 2021 |
- Study Details
The objective of this study is to determine if silicone adhesive multilayer foam dressings applied to the sacrum, heels and greater trochanter in addition to standard prevention reduce pressure ulcer incidence category II, III, IV, Unstageable and Deep Tissue Injury compared to standard pressure ulcer prevention alone, in at risk hospitalised patients. In particular, this trial extends previous trial results obtained in ICU setting. Therefore, only a maximum of 25% of patients will be recruited from ICU settings.
| Phase | ||
|---|---|---|
| Pressure Ulcer | Device: Allevyn® brand silicone adhesive multilayer foam dressingsDevice: Mepilex® brand silicone adhesive multilayer foam dressings | Not Applicable |
A multicentre randomised controlled open label parallel group medical device trial in approximately 8 hospitals in Belgium.
Patients will be randomly allocated to three study arms based on a 1:1:1 allocation:
Study arm 1 :
Study arm 2 :
Study arm 3 :
| Experimental: Study Arm 1 |
Which Wound Dressing Is Best For Your Pressure Ulcer
Now that weve touched on some of the more common types of dressings used for pressure ulcers, you may be wondering which is the best for your particular situation. The answer will depend on multiple factors including where the pressure ulcer is located, how severe the bedsore is, and the degree of skin and tissue damage. Talk to your health care professional about any pressure wounds you notice on your body as soon as possible.
You May Like: Natural Treatment Of Ulcer In Hindi
Foam Dressings For Treating Pressure Ulcers
What is the aim of this review?
The aim of this review was to find out whether foam dressings have any advantages or disadvantages in healing pressure ulcers compared with other dressings . Researchers from Cochrane collected and analysed all relevant studies to answer this question and found nine relevant studies.
Key messages
There is no clear evidence from any of the studies included in this review that foam dressings are more effective at healing pressure ulcers than other types of dressings or that foam dressings are more cost effective than other dressings. This is due in part to the low quality of the studies, many of which had small numbers of participants and did not provide accurate details of their methods.
What was studied in the review?
Pressure ulcers are wounds that develop on bony parts of the body such as the heels, hips and lower back. Sitting or lying in the same position for long periods can cause damage to the skin and underlying tissue. People at risk of developing pressure ulcers include those with limited physical mobility such as people with spinal cord injuries, older people, or those ill in hospital.
What are the main results of the review?
Generally, the studies we found did not have many participants and the results were often inconclusive. Overall the evidence that exists is of very low quality.
How up to date is this review?
We searched for studies that had been published up to February 2017.
Background To The Indication And Devices
Pressure ulcers are localised injuries to the skin and/or underlying tissue as a result of pressure, or pressure in combination with shear . Pressure ulcers can range in severity and can be classified into the following categories or stages :
-
Stage 1 Intact skin with non-blanchable erythema of a localised area. Discoloration of the skin, warmth, oedema, hardness or pain may also be present.
-
Stage 2 Partial thickness loss of dermis presenting as a shallow open ulcer with a red/pink wound bed, without slough or bruising. It may also present as an intact or open/ruptured serum-filled blister.
-
Stage 3 Full thickness tissue loss. Subcutaneous fat may be visible, but bone, tendon or muscle are not exposed. Some slough may be present. It may include undermining and tunnelling.
-
Stage 4 Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present. It often includes undermining and tunnelling.
Pressure ulcers can have a significant impact on a patients quality of life, both physically and psychologically. They can also lead to further health complications such as infection, extended hospital stays, restricted rehabilitation and restricted treatment options for other medical conditions .
All patients are at risk of pressure ulcers. However, Mepilex Border dressings have been indicated for use in people identified as either at risk or at high risk of developing a pressure ulcer.
Guy reports that risk factors for pressure ulcers include:
Recommended Reading: Ulcer On Eye From Contact Lens
Description Of The Condition
Pressure ulcers, also known as pressure injuries, decubitus ulcers and bed sores, are a localised injury to the skin, underlying tissue, or both, usually occurring over a bony prominence, as a result of pressure, or pressure in combination with shear stress from restrictive bedding where unaligned body weight is pushing one part of the body such as bone or muscle in one direction, and another part of the body, usually skin, in the opposite direction . The development of a pressure ulcer is a serious complication resulting in pain, decreased quality of life and significant expenditure of both time and money for the healthcare industry . Pressure ulcers are an internationally recognised patient safety problem, estimated to affect 2.5 million people annually .
The main factors associated with the development of pressure ulcers are exposure of the skin to excessive pressure, and a reduced tolerance of the skin to pressure. Pressure is exerted on the skin, soft tissue, muscle, and bone by the weight of an individual or a device applied against the surface of their skin. Tissue tolerance is the ability of the skin and its supporting structures to tolerate the effects of pressure by distributing it and by the transfer of pressure loads from the skin surface to the skeleton . Tissues are capable of withstanding enormous pressures briefly, but prolonged exposure to pressure initiates a series of events that lead potentially to necrosis and ulceration.
What Is A Foam Dressing

Wound dressings can accelerate the healing process by protecting the injury or wound from bacteria and creating an environment which supports healthy healing. Foam dressings are an effective tool for moist wound healing and are particularly useful in preventing dressing-related trauma, managing exuding wounds, and minimizing dressing discomfort and pain.
Recommended Reading: Is Ulcerative Colitis Considered An Autoimmune Disease
Construction And Features Of Foam Dressings
Made of semipermeable polyurethane, foam dressings contain foamed polymer solutions with small, open cells that can hold fluids. These cells may be layered with other materials. Their absorptiveness varies depending on the thickness of the dressing. The contact area of a foam dressing is nonadherent and nonlinting, so the dressing is easy to remove. The outer layer of the dressing is often hydrophobic or waterproof to keep out bacteria and other contaminants. Foam dressings come either with or without an adhesive border and in many sizes and shapes. Some foam dressings also include a bacterial barrier made from a transparent film. Additionally, some foam dressings are impregnated with an antimicrobial agent such as silver, Manuka honey, cadexomer iodine, antibiotics, or include surfactants as a vehicle for delivery of these substances to the wound bed.
A primary feature of foam dressings is that they help maintain a moist wound environment. Also important is that foam helps cushion the wound and periwound area from additional trauma, as well as providing thermal insulation for wounds. Easy to apply and remove, foam dressings don’t cause wound trauma. Foam dressings can be used when there is an infection and during compression therapy. In addition, foam dressings are compatible with enzymatic debridment agents. Depending on the amount of exudate, foam dressings have a wear time of one to seven days.
Description Of The Intervention
Treatment of a pressure ulcer is primarily twofold and involves the relief of pressure allied with wound management. Other general strategies include patient education, pain management, optimising circulation/perfusion, optimising nutrition and the treatment of clinical infection . Wound management may involve surgical or chemical debridement and dressings to protect the wound and possibly promote healing. Dressings can be divided into four main categories, namely, basic wound dressings, advanced wound dressings, antimicrobial dressings and specialist dressings. Classification of a dressing depends on its purpose and the key material used in its composition. Key attributes of a dressing have been described , and include: the ability of the dressing to absorb and contain exudate without leakage or strikethrough lack of particulate contaminants left in the wound by the dressing thermal insulation permeability to water but not to bacteria avoidance of wound trauma on dressing removal frequency with which the dressing needs to be changed provision of pain relief and comfort.
Basic wound contact dressings
Advanced wound dressings
Antimicrobial dressings
Specialist dressings
-
Proteasemodulating matrix dressings: these dressings are designed to alter the activity of proteolytic enzymes in chronic wounds and are thought to promote natural debridement.
Also Check: Do Stomach Ulcers Cause Nausea