Vitamin And Mineral Supplementation
Nutritional supplements are great for patients with inflammatory bowel disease who may need a bit of extra help preventing a nutritional deficiency.
Your healthcare providers may also recommend a vitamin and/or mineral supplementation plan if your tests show you already have a nutritional deficiency.
You may be able to get all your necessary vitamins and minerals from eating a well-balanced, nutrient-rich diet. But flares, severe symptoms, surgeries, and other complications may make it difficult for some patients with Crohns disease or ulcerative colitis to get enough nutrients from food alone.
Check with your doctor or other healthcare providers before taking any supplements, including over-the-counter medications, herbs, and other complementary therapies.
-
Some supplements can cause gastrointestinal symptoms, including nausea and diarrhea.
-
Check the labels on your supplements for lactose, artificial colors, sugar alcohols, or preservatives, all which can aggravate your IBD, especially when you are in a flare.
-
Most supplements should not be taken on an empty stomach.
Video Length00:02:00
Vitamin and Mineral Supplementation in IBD Often times, when you have Crohn’s disease or ulcerative colitis, you may need to take vitamins or minerals to prevent or make up for a nutritional deficiency. Watch and listen this video to learn more about common vitamin and mineral supplements for IBD patients.
What Types Of Diets Should I Consider
Both experts agree that everyones ulcerative colitis symptoms, triggers, and treatments are different, but there are certain eating styles that may be worth considering.
Talk with a health professional about whether one of these diets could be beneficial for you.
FODMAP is an acronym for types of carbohydrates that are poorly absorbed in the small intestine, specifically:
- Fermentable
- Monosaccharides
- Polyols
Because of their poor digestion, FODMAPs can cause gastrointestinal issues in some people7. Research suggests an improvement in IBD symptoms in some patients who follow a low FODMAP diet, but there is no evidence of improved inflammation8.
Some health care providers may counsel their patients to try a FODMAP elimination diet during an UC flare, followed by reintroduction of FODMAP foods once in remission.
What does that mean for actually eating food? Well, you may want to try swapping high-FODMAPs like cauliflower, mushrooms, dried fruit, cows milk, and legumes for low-FODAMPs like eggplant, carrots, grapes, potatoes, eggs, quinoa, and tofu.
The Mediterranean diet is widely considered to be one of the worlds healthiest eating patterns for people with and without chronic conditions.
While you may have heard of the paleo diet, the autoimmune protocol diet , which is considered to be similar to the paleo diet, may have some benefits for people with IBD.
Although some very small studies see the benefits of this style of eating, more research is needed10.
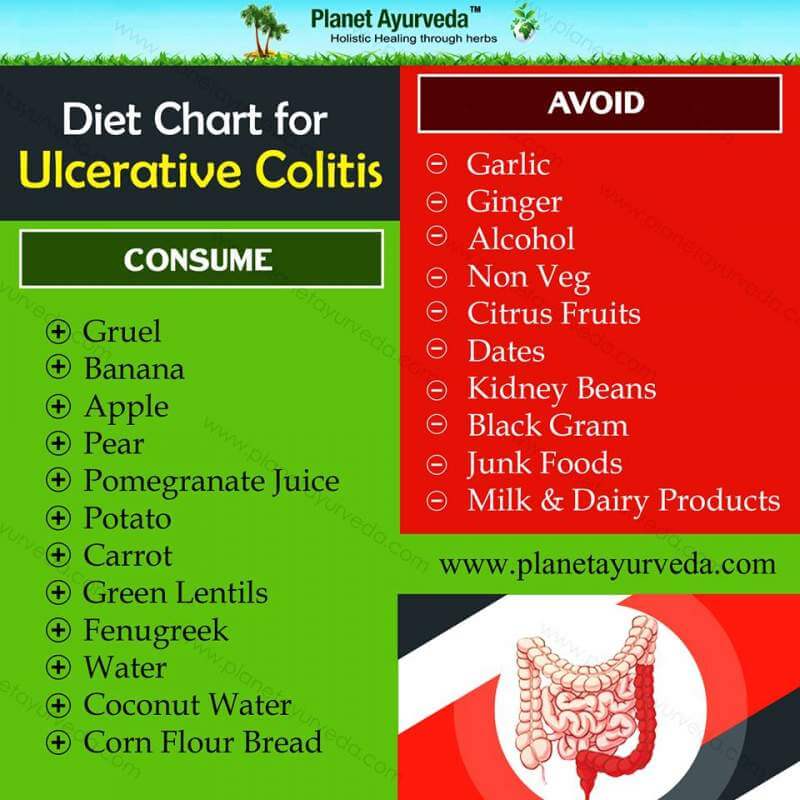
Diet For Ulcerative Colitis
Ulcerative colitis is, literally, a pain in the rear: An inflammation of the large intestine and rectum. The symptoms abdominal pain, cramping, diarrhea and bleeding can be debilitating.
And if you have ulcerative colitis, you know that sometimes it flares up, and it often depends on what youve had to eat. Its important to understand that certain foods do not cause ulcerative colitis and the Crohns and Colitis Foundation of America says diet is not a major factor in causing inflammation. However, some colitis sufferers experience issues related to what theyre eating, so its smart to have an Ulcerative Colitis Diet Plan to help control those flare-ups.
Many people do identify some food triggers and these should be avoided if possible, says Crozer Health gastroenterologist Joyann Kroser, M.D. I think patients who keep a food-and-symptoms diary have more insight into what foods may challenge them. Here is a diet plan that works for most ulcerative colitis patients:
Don’t Miss: Worst Foods For Stomach Ulcers
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
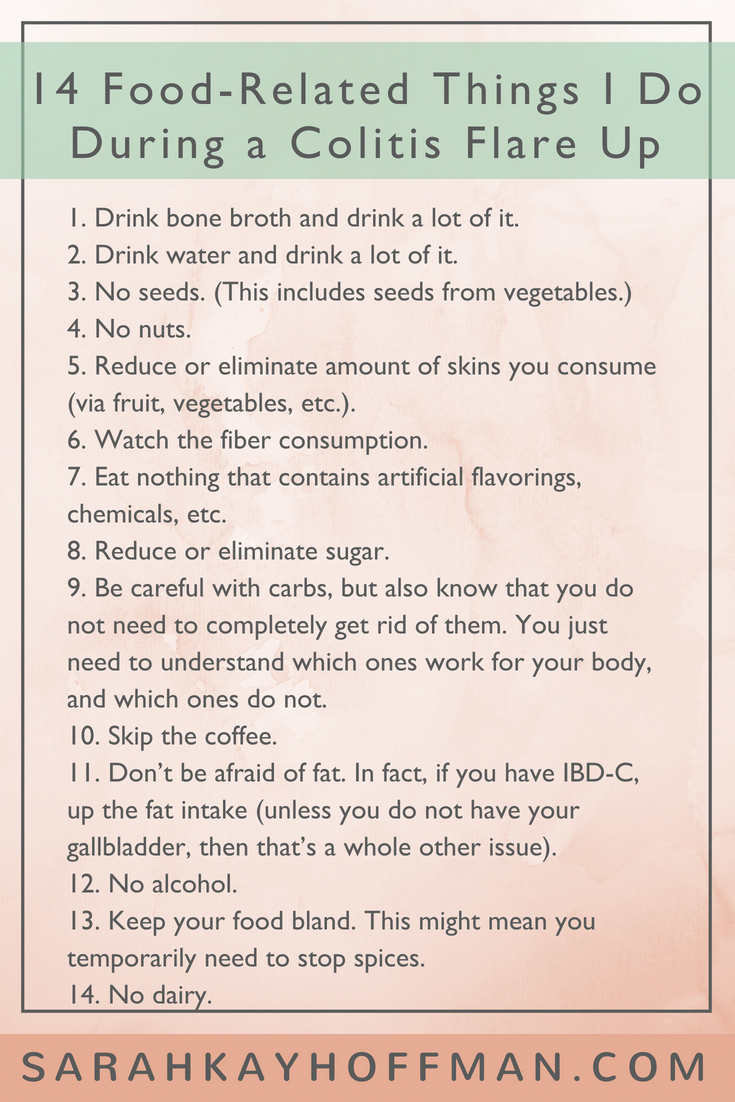
What To Do During A Flare
Medications are used to manage flares and induce remission as quickly as possible.
Doctors may prescribe a corticosteroid , antibiotic, 5-aminosalicylate, immunomodulator or biologic.
In addition, certain diet changes may help shorten flares. Some tips to keep in mind:
- Keep a food and symptom journal during flares to identify bothersome foods. This also ensures that foods are not avoided without cause.
- Eat small, more frequent meals as opposed to 3 large meals in a day .
- Ask your doctor whether to limit fiber until symptoms pass. Eating a maximum of 10 grams of fiber per day may reduce irritation and lower the risk of intestinal blockage. Once you are in remission, gradually increase your fiber intake, depending on how much you can tolerate, until you reach the recommended daily intake of 2530 grams.
- Drink plenty of fluids to avoid dehydration.
Recommended Reading: Hand Foot And Mouth Ulcers
Cooked And Peeled Vegetables
Many vegetables are high in fiber, but as with fruit, peeling them removes a layer of insoluble fiber.
Some vegetables do not need peeling, such as asparagus tips and mushrooms, but it can help to remove the skins of potatoes, carrots, and squash.
Cooking vegetables also makes them easier to digest, and it can reduce the fiber contents.
However, avoid roasting or frying vegetables in oil or butter, because fats can irritate the digestive system and worsen symptoms of Crohns. Try boiling or steaming them instead.
Read Also: Best Ulcerative Colitis Diet Book
What Are Some Of The Different Diets That People Try For Ibd
There are several diets that people claim can help with IBD, but these recommendations are often based on reported experiences rather than research. We will review some of the more popular diets, with their potential advantages and disadvantages. Still, it is important to know that none of them have strong scientific support.
Also Check: Ulcerative Colitis Medication Not Working
What Should I Eat
Its not always easy knowing what foods best fuel your body, especially when you have Crohn’s disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, thesymptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
Also Check: What Foods Should You Eat If You Have An Ulcer
General Guidelines When Ulcerative Colitis Is In Remission
Some members of MyCrohnsAndColitisTeam find they can eat a wider variety of foods safely during remission periods when ulcerative colitis is not as active and symptoms are absent or mild. Still, every individual is different, and purportedly beneficial foods may trigger symptoms. Trial and tracking is the only way to know for sure.
If it is safe for you, these guidelines may help you stay your healthiest during remission:
- Get 25 grams to 35 grams of fiber per day to promote bowel regularity and reduce inflammation.
- Consume plenty of lean meats, which are a good source of B vitamins. Include fatty fish, tofu, and nut and seed butters.
- Include probiotic foods such as yogurt, tempeh, kefir, kimchi, miso, and sauerkraut.
While some members find kefir too sour for their liking, others report experiencing benefits from trying the fermented drink. Kefir has been helping me over the past week, wrote one. Been trying kefir the past few days. Will keep you posted. So far less pain, said another.
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
Recommended Reading: What Not To Eat If You Have An Ulcer
Foods To Avoid During Ulcerative Colitis Flares
During a flare, ulcerative colitis symptoms become more severe, and certain foods can worsen them further.
Following these guidelines can keep you away from the most common food triggers during UC flares:
- Avoid high-fiber foods, such as whole grains, dried fruit, and raw vegetables or vegetables with tough skin. Make sure to cook vegetables thoroughly, and avoid vegetables with seeds.
- Avoid cruciferous vegetables that produce gas, such as broccoli, cauliflower, and Brussels sprouts.
- Avoid spicy foods.
- Avoid caffeine in coffee, tea, and other beverages. This can contribute to diarrhea.
- Avoid whole nuts and seeds. Choose smooth nut butters. Almond butter, peanut butter, cashew butter, and sunflower butter are all great choices.
- Avoid fried foods, fatty foods, and highly processed foods.
- Avoid high-sugar foods, like fruit juice and baked goods. These can contribute to diarrhea.
Some members of MyCrohnsAndColitisTeam learned about their food triggers the hard way. Last time I drank coffee, I felt every centimeter of my intestines. Big no for me, shared one member. Another member communicated her hard-won personal rule very clearly: No sugar, and I mean NO SUGAR AT ALL!
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
Also Check: Does Smoking Cause Ulcers After Gastric Bypass
Yogurt Parfait With Mixed Berries
Yogurt is a source of probiotics, or good bacteria, which can be especially helpful for someone with Crohns, as probiotics aid digestion and help heal the gut. The bacteria also eat some of the lactose, which makes this naturally easier to digest for those with lactose intolerance or sensitivity.
Yogurt is also a great and provides calcium and potassium. Look for plain, unflavored yogurt that contains live, active cultures and no added sugars.
Ingredients
- ¼ c strawberry fruit spread*
- ½ c frozen blueberries, unthawed
- 1 c fresh strawberries, sliced
- ¼ c slivered almonds**
- ¼ tsp lemon juice
*Both the yogurt and the fruit spread in this recipe are homemade and sweetened with honey, to adhere to the Specific Carbohydrate Diet . If you use store-bought ingredients, try to select an additive-free fruit spread that has no added sugar and plain yogurt with active, live cultures. Visit Elizabeth M Jacobs blog for this recipe and other ideas.
**Substitute with a well-tolerated breakfast cereal if nuts irritate your stomach.
Practical Advice For What To Eat On An Ulcerative Colitis Diet
Many organizations post food shopping lists for Ulcerative Colitis Disease. These resources are a good starting point. Download a list and make it your own. Mark off your trigger food and add foods that you can safely eat.
Plan ahead and enhance your weekly menus with MealPro Ulcerative Colitis meal delivery service. These anti-inflammatory meals are designed to eliminate known trigger foods and reduce flares.
Roasted salmon: This meal is full of flavor while providing healthy omega-3s with a portion of asparagus and yellow bell peppers. Roasted potatoes round out the meal for a satisfying choice in carbs.
Turmeric Turkey: Lean turkey seasoned with the anti-inflammatory spice turmeric. Served with fresh green beans and bake yams. Rice is the foundation of this meal.
So, can Ulcerative Colitis symptoms change the way you eat? Yes. Although it is possible to adjust the foods you eat to improve and enhance your quality of life.
Also Check: Bland Diet Recipes For Ulcers
What Foods Should I Eat During An Ulcerative Colitis Flare
When you are experiencing an ulcerative colitis flare-up, experts suggest you stick to foods that are less likely to aggravate your gut. Some of these include:
- White rice, bread, and pasta
- Crackers and cereals made with refined white flour
- Cooked veggies without the skin
- Tender, soft meats and fish
- Olive and coconut oil
- Eggs
- Lots and lots of fluids, since an ulcerative colitis flare-up can lead to diarrhea and thus dehydration
These foods have been found to be easily digestible in some ulcerative colitis patients, but be cautious when adding them to your diet since they can be triggers in other patients:
- Squash
- Probiotics
- Plain instant oatmeal
When you are experiencing an ulcerative colitis flare-up, experts suggest you stick to foods that are less likely to aggravate your gut.
How To Eat During An Ibd Flare
Robert Burakoff, MD, MPH, is board-certified in gastroentrology. He is the vice chair for ambulatory services for the department of medicine at Weill Cornell Medical College in New York, where he is also a professor. He was the founding editor and co-editor in chief of Inflammatory Bowel Diseases.
People with inflammatory bowel disease often face an uphill battle when it comes to diet, especially when the disease is active. Many people with IBD don’t know what food to eat when the Crohn’s disease or ulcerative colitis is flaring. Everyone with IBD is different, and one person’s flare-up diet isn’t going to work for another, but there are some broad ideas that may work for many.
-
Milk, cheese, ice cream, and yogurt
-
Brown rice, popcorn, oats, and barley
-
Fried food
-
Raw veggies
Also Check: How Do I Get Rid Of A Stomach Ulcer
Tips For Meal Prepping
Now that you have a sense of what to eat for ulcerative colitis, its time to get in the kitchen. Meal prepping some simple ingredients can make your life easier and prevent a UC flare. Here are some simple strategies:
- Buy pre-chopped fruits and veggies. Having produce in your fridge that dont require any preparation will make you more likely to add them to your plate at mealtime.
- Go frozen. Frozen fruits, veggies, and whole grains are generally as nutritious as fresh produce. Buy frozen fruit for smoothies, frozen veggies for soups and casseroles, and frozen grains to heat up in the microwave as a side dish.
- Pick up ready-made proteins. Stock up on simple options, like a rotisserie chicken or canned beans.
- Make a big batch of soup. Not only is soup soothing, its also an easy way to add a ton of veggies to your diet and is super easy to make in big batches.
- Stock up on healthy fats. Load up your cabinet with nuts, oils, and seeds for snacking, cooking, or adding texture to a recipe.
What Is The Scd Diet
The Specific Carbohydrate Diet was developed by Elaine Gottschall whose own daughter was diagnosed with severe ulcerative colitis at the age of 4 and has helped people all over the world manage the symptoms of Crohns disease, ulcerative colitis, IBS, celiac, diverticulitis, autism, cystic fibrosis, and other ailments rooted in the digestive tract.
The SCD Diet allows specific foods based on their chemical structure. It limits the use of complex carbohydrates and focuses primarily on monosaccharides. Foods that are not properly digested, such as grains, sugars, starches, and processed foods, are banned on the SCD Diet as they cause bacterial and yeast overgrowth, irritation of the small intestine, and challenges with food absorption. The SCD Diet is designed to restore gut flora and stop the vicious cycle of bacteria and yeast overgrowth by eliminating the foods they feed on, thereby allowing the intestinal tract to repair and heal.
You can find an extensive list of the foods that are and are not allowed on the SCD Diet HERE, and I urge you to read Elaines book, Breaking the Vicious Cycle, in its entirety as she does such a great job of describing the role diet plays in the treatment of the disorders listed above.
Weve written an entire post about the SCD Diet, including tips for beginners, strategies to stay motivated, and some of the things my husband and I learned through trial and error, which you can read HERE.
Read Also: What Happens When You Have A Bleeding Ulcer