Right Or Middle Abdomen Pain
This pain may feel like cramps in the middle of the abdomen or the RLQ. It is most common with the types of CD known as ileocolitis and ileitis. Together, these subtypes account for 75% of all CD that is diagnosed.
With ileocolitis, which is the cause in 50% of CD cases, the inflammation is found in the ileum, the last section of the small intestine. It also affects part of the colon, or large intestine.
Ileitis, which is diagnosed in 25% of cases, affects only the ileum. People with ileitis sometimes find that their pain or discomfort will arrive within a few hours of eating a meal.
Tips For Infusion Day
Its been two years since I started getting my medication for my ulcerative colitis by infusion. I get my infusions every six weeks, which isnt quite often enough to completely get used to them. I still wake up early each infusion morning remembering I have an appointment and worrying Ill sleep through my alarm and miss it. But in the two years Ive been doing this, I have learned a few things along the way.
1. Bring things to do that you enjoy. Some infusions have lasted three hours, plus the time spent in the waiting room and waiting for the medication to arrive. Compared with that experience, the half-hour infusion usually flies by. But as with any doctors appointment, I never know how long Ill have to spend waiting around, and I like having multiple options to distract me. I usually bring something fun to read or download a couple of episodes of a show I like onto my iPad, and I make sure I have music or podcasts to listen to. Sometimes I even bring a coloring book. I rarely ever use all of these options, but it makes me feel better knowing I have them.
3. Drink lots of water beforehand. I cant believe it took me two years to figure this one out. Before every infusion, a nurse would spend what felt like an eternity poking around at my arm trying to find a good vein. Sometimes it would take more than one person to try putting in an IV. Since I started making a conscious effort to drink more water before my appointment, I havent had that problem.
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Read Also: Ozanimod Mechanism Of Action Ulcerative Colitis
Back Pain And Ulcerative Colitis
Research indicates that nearly 25 percent of people with inflammatory bowel disease including ulcerative colitis and Crohns disease experience chronic lower back pain. Ankylosing spondylitis and axial arthritis both of which can cause back pain are two common causes of back pain in people with UC.
That said, a doctor may not suspect that a person with back pain has UC unless they also experience gastrointestinal symptoms. If you do experience back pain, its important to let your doctor know even if you dont suspect that its related to UC. They will be able to determine the cause of your pain and work with you to find the best way of managing it.
Also Check: Stomach Ulcer And Weight Loss
Crohns & Colitis Uk Local Networks

Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn’s or Colitis. All events are open to members of Crohns & Colitis UK
Also Check: What Not To Eat With An Ulcer
High Risk For Sexual Dysfunction
Women with IBD do experience sexual dysfunction either in form of pain during sex or lack of sexual desire. Everything in the pelvis is interconnected, and this is why when one organ system isnt functioning, it can affect them all. Women also experience pelvic floor spasms, which tighten and make intercourse difficult.
Considering different sexual positions and focusing on physical intimacy other than traditional intercourse might help to ease the pain.
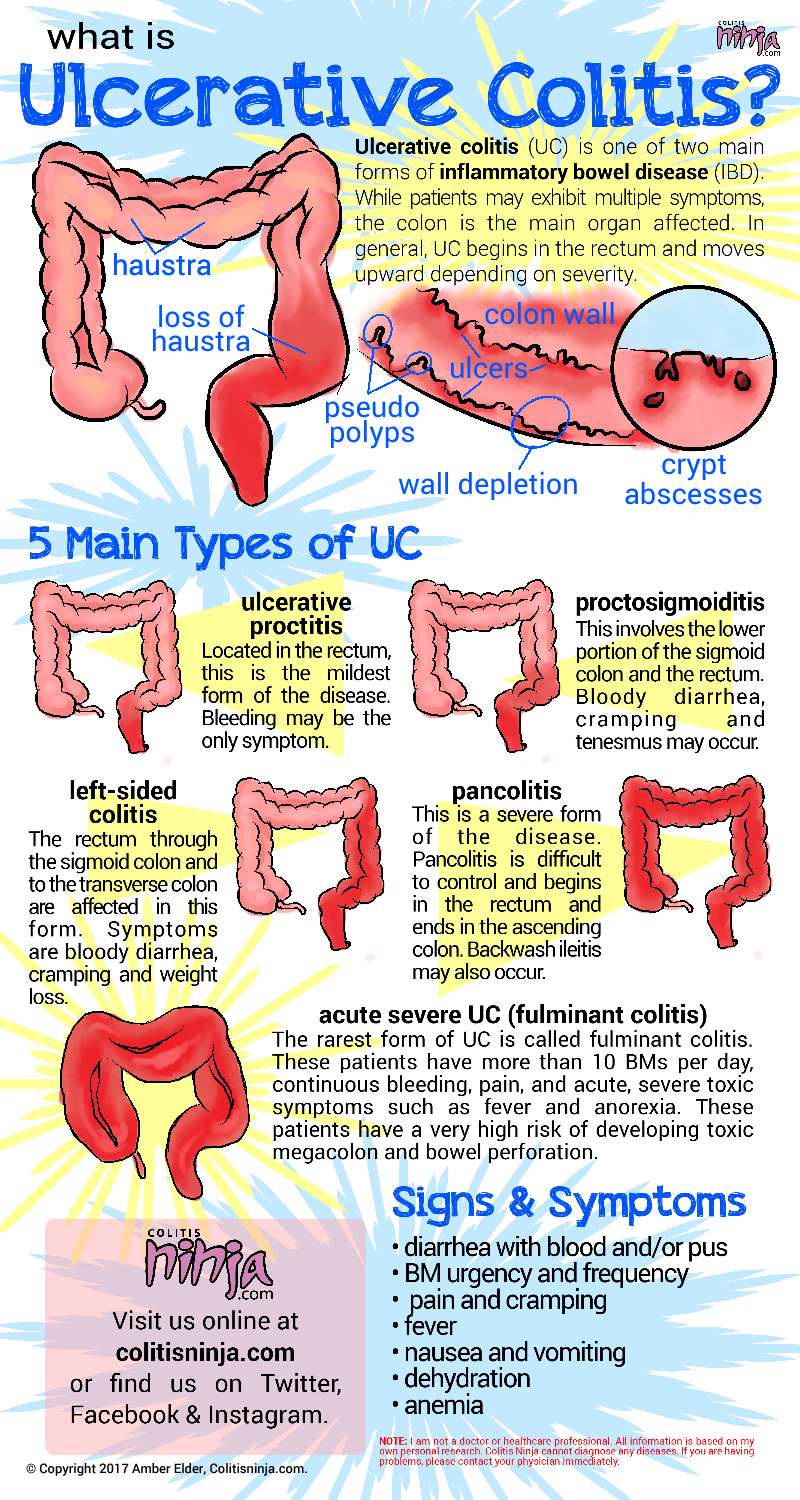
Where Does Ulcerative Colitis Pain Come From
Ulcerative colitis can be an unpredictable condition as the cause of it has yet to be uncovered. The illness is also associated with flare-ups, which can have unique triggers. Approximately 30% of people who are currently in remission will relapse in the next year.
It is believed that there is a genetic component that comes into play with this condition. Those with family members with ulcerative colitis are more likely to be afflicted by this condition. This disease can generally be found in any age group, but it is far more prevalent between the ages of 15 to 30, as well as 50 to 70. It is also believed that Caucasians are much more likely to develop this condition and the risk is even higher for those of Ashkenazi Jewish decent.
At one time, it was believed that ulcerative colitis was caused by stress and diet. Today, researchers believe these can be a trigger, but they no longer think it is a direct cause. Most studies are focused on searching the immune systems for a root cause for this condition. It is thought that the immune system might inadvertently attack the healthy cells in the GI tract when trying to fight off foreign invaders, which causes inflammation.
You May Like: Can Ulcerative Colitis Cause Body Aches
Read Also: How To Treat An Ulcer After Gastric Bypass
Who Develops Ulcerative Colitis
About 2 in 1,000 people in the UK develop ulcerative colitis. It can develop at any age but most commonly first develops between the ages of 10 and 40. About 1 in 7 cases first develop in people over the age of 60 years. Non-smokers are more likely than smokers to develop ulcerative colitis. However, smoking brings other dangers to health which far outweigh this benefit.
Also Check: How To Stop An Ulcerative Colitis Flare
Smoking Increases The Risk Of Both Ulcerative Colitis And Crohns Disease But Nicotine Has Different Effects On Colonic Versus Small Bowel Inflammation
There are two commonly accepted beliefs about the relationship between smoking and Crohnâs disease and ulcerative colitis: smoking increases the risk of Crohnâs disease but protects an individual from developing ulcerative colitis, and smoking increases the severity of Crohnâs disease, but decreases the severity of ulcerative colitis. If ulcerative colitis and Crohnâs disease are both caused by MAP, how can these apparently dichotomous effects be explained? An excellent review article by Lakatos and colleagues helps elucidate the reasons for the different effects of smoking on these diseases.
First, in children, smoking increases the risk of developing both ulcerative colitis and Crohnâs disease. In a study of inflammatory bowel disease in Kentucky children , children who started smoking before 10 years of age were 7 times more likely to develop ulcerative colitis than nonsmokers, and over 3 times more likely to develop Crohnâs disease than nonsmokers. If they started smoking before age 15, they were over three times more likely to develop both diseases. Smoking increased the risk of developing both Crohnâs disease and ulcerative colitis, and in this one study increased the risk of ulcerative colitis more than it increased the risk of Crohnâs disease .
You May Like: How Effective Is Humira For Ulcerative Colitis
Read Also: Bowel Ulcers Signs And Symptoms
When To Call The Doctor
- Cramps or pain in your lower stomach area
- Bloody diarrhea, often with mucus or pus
- Diarrhea that cannot be controlled with diet changes and drugs
- Rectal bleeding, drainage, or sores
- Fever that lasts more than 2 or 3 days, or a fever higher than 100.4°F without an explanation
- Nausea and vomiting that lasts more than a day
- Skin sores or lesions that do not heal
- Joint pain that keeps you from doing your everyday activities
- A feeling of having little warning before you need to have a bowel movement
- A need to wake up from sleeping to have a bowel movement
- Failure to gain weight, a concern for a growing infant or child
- Side effects from any drugs prescribed for your condition
When Does Cramping Usually Happen
UC cramps can be exacerbated by food, so many people notice cramping after eating or before a bowel movement, says Ha. Cramping can also be tied to eating trigger foods, which often include high-fiber fruits and veggies, lactose, nonabsorbable sugars, high-fat or sugary foods, alcohol, and caffeine.
The hormone fluctuations that occur during a womans menstrual cycle may also trigger UC cramping, according to a study published in January 2018 in Inflammatory Bowel Diseases.
Cramping can occur at all times and throughout the night. Medication and other treatments can help reduce symptoms.
Read Also: Remicade Dosing For Ulcerative Colitis
When Should You Call Your Doctor
If youre experiencing certain symptoms, chances are, your current treatment is not working and its time to consider a change in therapy, says Ha. Call your doctor if:
- Cramping is severe
- Youre experiencing a significant amount of abdominal pain that requires medication
- You have a fever that lasts longer than a couple of days
- You experience nausea or vomiting
- You have ongoing diarrhea or blood in your stool
Diagnosing Uc And Crohn’s Abdominal Pain

If your abdominal pain and cramps get worse, it could be a sign that your inflammatory bowel disease is flaring up.9 It may be necessary to see your health care provider.
You may need blood or stool tests to check for signs of inflammation. Your provider may want to do procedures such as colonoscopy or upper endoscopy, computed tomography scan, or small-bowel follow-through. These procedures are done to check for inflammation, obstruction, or abscess.9
You May Like: How Would You Know If You Had A Bleeding Ulcer
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Turmeric And Ginger Tea
Turmeric, a relative of ginger, has been used in Ayurvedic medicine for millennia to help treat inflammatory diseases. Curcumin, the active component of turmeric, may be a safe, effective therapy for maintaining or inducing UC remission when administered with standard treatments, according to a review published in July 2020 in Nutrients. Try this soothing concoction submitted by nascarrunner71 at AllRecipes.com: Hot or cold, this tea combines ginger, turmeric, and honey or maple syrup for a rich and flavorful tea.
Read Also: Stomach Ulcer Treatment Over The Counter
How To Treat Ulcerative Colitis Pain
While there isnt a cure for ulcerative colitis yet, there are ways to treat the inflammation and discomfort. In most UC cases the pain is at its worst during a flare-up, and some peeps are completely pain-free outside of these times. Pain treatment involves a mix of reducing the risk of painful flare-ups and the discomfort experienced during them.
Some treatments are medical interventions, while others are lifestyle and self-management techniques. Here are some effective options:
Outlook For People With Ulcerative Colitis
If you have UC, a doctor will need to monitor your condition, and youll need to carefully follow your treatment plan throughout your life.
The only true cure for UC is removal of the entire colon and rectum. Your doctor will usually begin with medical therapy unless you have a severe complication that requires surgery. Some people will eventually require surgery, but most do well with nonsurgical therapy and care.
Also Check: Can A Heating Pad Help Ulcerative Colitis
Complications Of Ulcerative Colitis
UC increases your risk of developing colon cancer. The longer you have the disease, the higher your risk of this cancer.
Because of this increased risk, your doctor will perform a colonoscopy and check for cancer when you receive your diagnosis.
Repeat screenings are recommended thereafter, according to the American Cancer Society. Regular screenings help lower your risk of colon cancer. Follow-up screenings can detect precancerous cells early.
Other complications of UC include:
- thickening of the intestinal wall
- intestinal bleeding
How Is Ibd Treated
Treatments for IBD may include:
- Medicines. Most people with IBD take medicine to control their symptoms.
- Surgery. Surgery may be an option if medicine does not work to control your symptoms. Learn more about surgery for Crohn’s disease and surgery for ulcerative colitis.
- Steps you can take at home. Your doctor can talk to you about steps you can take at home to help control your symptoms and prevent flare-ups.
- Changes to your eating habits. Avoiding certain foods, changing other eating habits, and limiting or avoiding alcohol may help control your symptoms during flare-ups.
Some forms of psychotherapy, sometimes called “talk therapy,” may also help you cope with stress related to IBD symptoms and help make your pain less severe.14 Your doctor can refer you to a counselor or therapist, or you can find one at .
Some counselors specialize in working with people who have IBD. A counselor can help you talk about any distressing emotions you might have about IBD symptoms. A counselor can also treat anxiety, depression, or other mental health concerns. Ask your doctor or nurse for a referral or recommendation for a counselor in your area.
You May Like: What Is Ultra Ulcerative Colitis
Youre Not Drinking Enough Fluids
If youre experiencing a bout of diarrhea, you run the risk of becoming dehydrated because your body is losing more fluids than its taking in. This can be harmful to your overall well-being and interfere with your bodys ability to heal.
Drink as much water as you can during a UC flare. Just keep in mind that there are some liquids you should think twice about if you have diarrhea, including pear, peach, or prune juice, according to the Crohns and Colitis Foundation all of them contain nonabsorbable sugars that can be rough on your gut.
You May Like: Turn Clock For Pressure Ulcer Prevention
What Are Ulcerative Colitis Treatment Options
Depending on the location and severity of your case of ulcerative colitis, there are different treatments that can help you feel better. For a long time, corticosteroids were the main form of medical treatment for IBD, but they can potentially have adverse effects when used long-term. With more research, options like immunosuppressants arrived. According to the Centers for Disease Control and Prevention , the newest type of medication approved for the treatment of IBD is biologics. These medications are made from living thingsrather than chemical compoundsand work to target proteins made by the immune system to reduce inflammation. If medication isnt effective, surgery is also an option.
Dr. Sinha emphasizes that keeping your health care team informed is key to managing ulcerative colitis. Having this regular communication helps facilitate labs, imaging, or endoscopy that may be necessary, he says. It also allows the providers to understand many other facets of the disease’s impact on the patient, such as the psychosocial impact.
Also Check: Foam Dressings For Pressure Ulcer Prevention
Complementary And Alternative Remedies
Alternative treatments such as acupuncture may help reduce and regulate bowel inflammation, reducing UC pain.
Another form of alternative treatment called moxibustion may also have a positive effect on UC symptoms. Moxibustion is a type of heat therapy. It uses dried plant materials burned in a tube to warm the skin, often in the same areas targeted by acupuncture.
Treatment Options For Crohns Disease
Recommended treatments may vary based on your symptoms and specific health history.
If you have mild to moderate Crohns disease your doctor may recommend:
- Aminosalicylates, like sulfasalazine
If you have moderate to severe Crohns disease, your doctor may recommend:
- Corticosteroids, such as prednisone and prednisolone
- Immunomodulators, like azathioprine and 6-mercaptopurine
- Biologics, like vedolizumab , adalimumab , infliximab , and ustekinumab
If you have severe Crohns disease or an acute flare-up, your doctor may recommend:
- Intravenous corticosteroids, such as methylprednisolone
- Biologics
Regardless of your level of severity, your doctor may prescribe broad-spectrum antibiotics if you have any abscesses or fistulas.
Read Also: Does Ulcerative Colitis Make You Tired