Cabbage Celery And Brussels Sprouts
Avoid eating cabbage, celery, and Brussels sprouts because they are high in fiber and potential colon lining irritants. Instead, have sweet potato, potato, carrots, and squash.
NOTE: Dairy is not mentioned in this list because a few people do not get ulcerative colitis flare-ups while others do. So, check with your doctor to find out if you can consume dairy products.
It may seem like you have run out of options to eat, but thats not the case. Here is the list of foods that you can eat.
What Causes Ulcerative Colitis
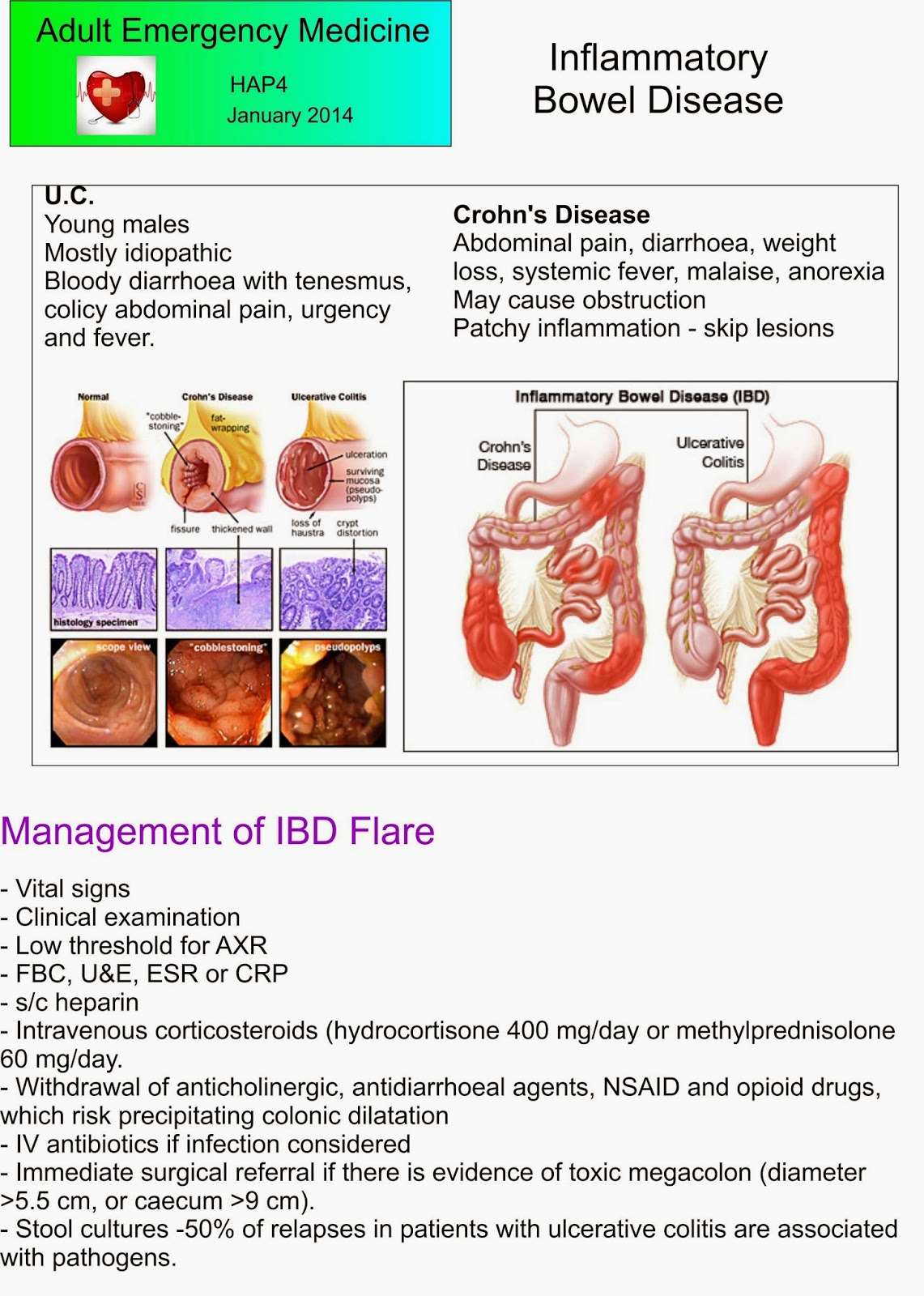
The cause of ulcerative colitis is unknown but it is believed to be caused by a combination of several factors including an overactive immune system, genetics, and the environment.
- Overactive immune system: It is believed that in ulcerative colitis, the immune system is triggered to mistakenly attack the inner lining of the large intestine, causing inflammation and symptoms of ulcerative colitis.
- Genetics: Ulcerative colitiscan run in families. The genetic link is not entirely clear but studies show that up to 20% of people with ulcerative colitis have a close family member with the disease.
- Environment: Certain environmental factors including taking certain medications , and eating a high fat diet may slightly increase the risk of developing ulcerative colitis.
Physical or emotional stress, and certain foods do not cause ulcerative colitis, however, they may trigger symptoms in a person who has ulcerative colitis.
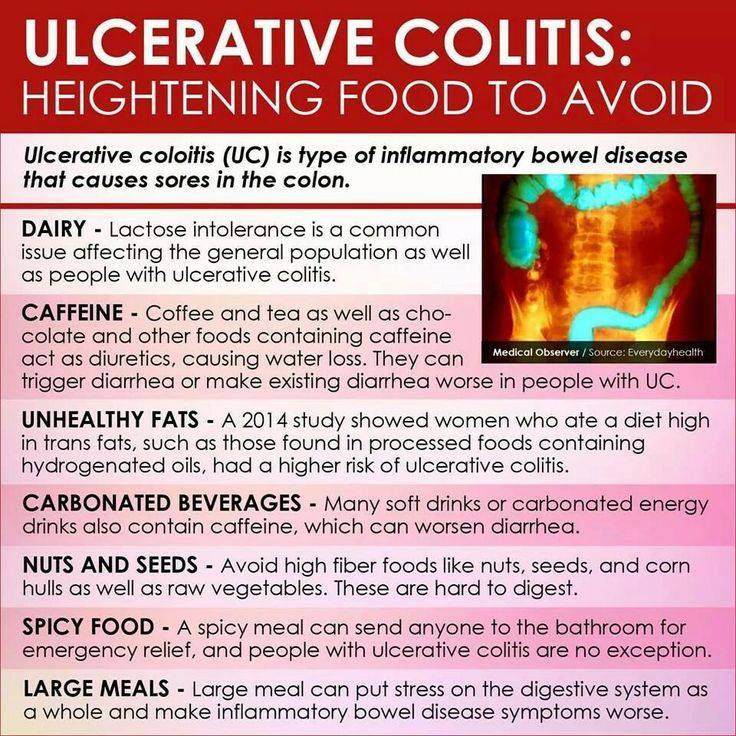
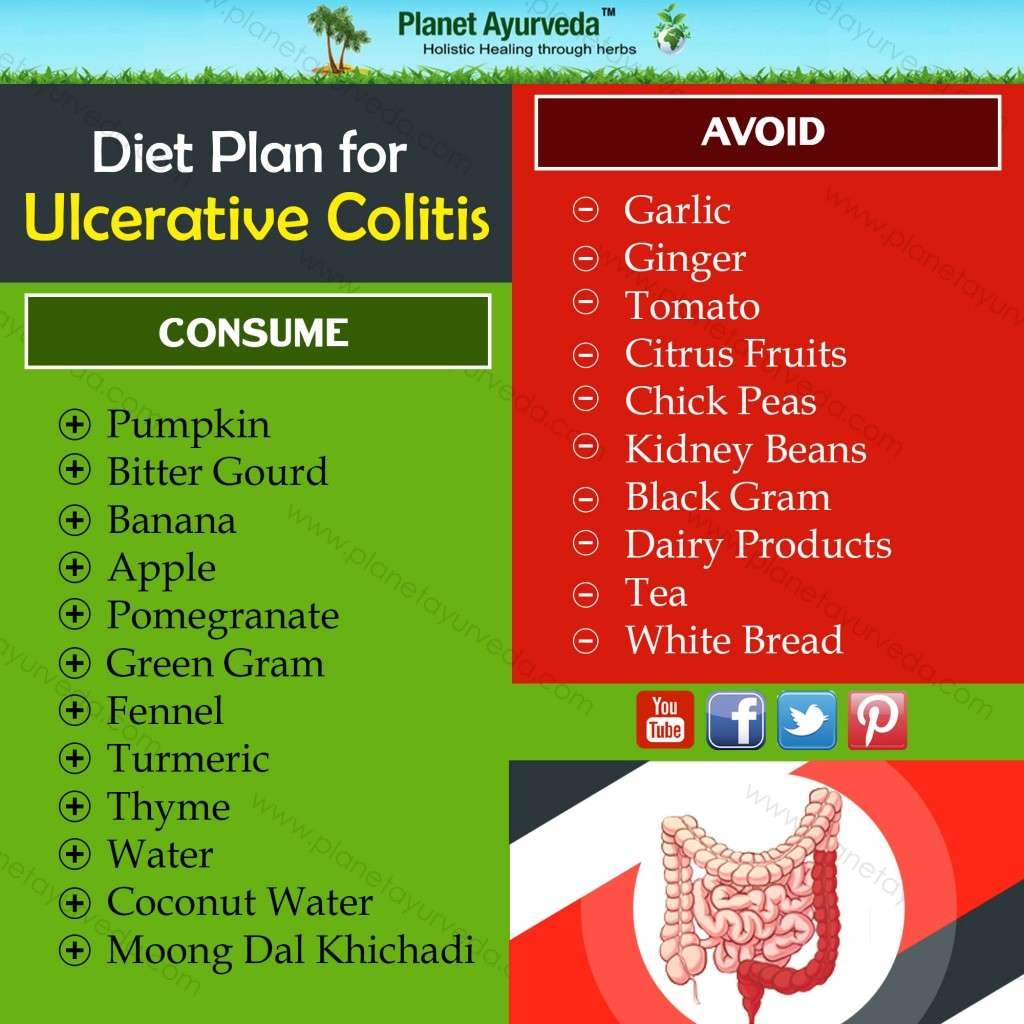
Ulcerative Colitis And Diet
There is no conclusive evidence that ulcerative colitis is caused by diet, but some foods may exacerbate your symptoms. Typically gluten is not considered a food that will trigger ulcerative colitis instead, dairy products, beans, broccoli, popcorn, alcohol, caffeine, raw fruits and vegetables and carbonated beverages are associated with triggering flare-ups of ulcerative colitis. However, if you notice that your symptoms are worse after consuming gluten, you should avoid all foods made with barley, rye or wheat.
Also Check: What Should You Eat When You Have Ulcerative Colitis
Is This Diet Safe
Though many health professionals suggest otherwise, its safe to follow a gluten-free diet even for people who dont necessarily need to do so.
Cutting out wheat and other gluten-containing grains or products will not cause adverse health effects as long as these products are replaced with nutritious foods.
All of the nutrients in gluten-containing grains, such as B vitamins, fiber, zinc, iron, and potassium, can easily be replaced by following a well-rounded, whole-foods-based diet consisting of vegetables, fruits, healthy fats, and nutritious protein sources.
Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
You May Like: Kraft Dressing Gluten Free
Also Check: How Do You Stop A Stomach Ulcer From Hurting
Which Are The Poorly Tolerated Foods For Ulcerative Colitis
Among the poorly tolerated foods, we have the following:
- Whole grains: They contain too high amounts of insoluble fiber, which normally produce adverse reactions, especially during the outbreaks of this disease. Nor are other whole breakfast cereals suitable .
Sometimes cereals with gluten can cause flatulence, so it is advisable to avoid taking wheat bread when pain or diarrhea.
- Cereals provide high vitamin B complex quantities, but whole cereals are not recommended because they can cause digestive irritation. Rice is the most suitable cereal.
- Vegetables: They are very rich in fiber and can be difficult to digest, besides being flatulent, especially if not eaten very cooked.
Food such as peas, chickpeas, or beans should be eaten with caution, overcooked, and always after having tried the patients tolerance.
- Fatty meats: They produce inflammation and mucus in the intestine of these patients. They shoud be avoided. Among them: sausages, pates, bacon, mortadella, salami, etc.
- Lamb meat, pork and duck are also rich in fat.
- Lean beef or skinless chicken can be eaten cooked, but they are inadequate when fried. These meats are adequate to supply the deficiency of vitamin B12.
Tolerance to ham, both sweet or salty, and York type should be proved. If slices of turkey, chicken or ham are consumed, seek those brands containing 0% fat.
Gluten And Ibd: Whats The Connection
Researchers have long suspected a link between celiac disease an immune reaction caused by eating gluten and IBD. One 2020 analysis published in May 2020 the journal Gastroenterology, found that people with celiac disease are 9 times more likely to have IBD than people without celiac.
Both celiac disease and IBD are autoimmune diseases. Sometimes when there is chronic inflammation and autoimmunity, people could tend to have more than one condition, explains , director of integrative gastroenterology at the Susan Samueli Integrative Health Institute at the University of California in Irvine.
When a person with celiac disease consumes gluten, an immune response is triggered in the small intestine. This can result in diarrhea, bloating, constipation, nausea, and vomiting, as well as fatigue and weight loss. Considering IBD also causes many of these symptoms, its easy to see how poorly managed celiac disease could make a persons gastrointestinal symptoms worse.
But what about people like Hanks and others with IBD who dont have celiac disease? Even without a celiac diagnosis, its still possible to have a gluten sensitivity or intolerance, which experts call non-celiac gluten sensitivity . For those with NCGS, consuming gluten can still trigger symptoms such as bloating, abdominal pain, diarrhea, and constipation as well as rashes, headaches, and feeling foggy, according to Mayo Clinic.
Read Also: Different Types Of Ulcerative Colitis
Digestive System Parts: A Brief Anatomy Overview
Before we dive into the specifics of comparing Crohns disease, ulcerative colitis, and celiac disease, lets briefly review the anatomy of your digestive tract. Your digestive tract extends from your lips to your anus. A bite of foods journey through your digestive tract looks something like this.4
Now that we got that out of the way, lets take a deeper look at each of these conditions of the digestive tract.
Ditch Unhealthy Fats For A Happier Digestive Tract
A Inflammatory Bowel Diseases found that diets high in trans fats, such as the hydrogenated oils found in processed foods, as well as peanut, canola, sunflower, and safflower oils, were more likely to trigger inflammation and caused a higher risk of ulcerative colitis. In contrast, people who consumed more omega-3 fatty acids, found in fatty fish, had a lower risk of UC. Another International Journal of Molecular Sciences reported that omega-3 fatty acids reduced intestinal inflammation, maintained remission, and improved quality of life.
Dr. Dassopoulos recommends limiting unhealthy fats for overall health. This includes saturated fats found in red meat. My advice to people with ulcerative colitis and Crohns disease is to follow a healthy Mediterranean diet and limit red meat, Dassopoulos says.
Don’t Miss: Signs You Have A Stomach Ulcer
Improvement Of Symptoms On A Gfd
Of the 314 patients, who have ever followed or were still following a GFD, 206 reported that they experienced an improvement of at least one specific clinical symptom which has been associated with gluten exposure . Furthermore 38.3% also recounted fewer and less severe flares while being on a GFD and 23.6% stated that they required fewer medications to control the disease. There were no significant differences pertaining to baseline characteristics between patients with or without improvement of clinical symptoms on a GFD .
Reported symptom improvements in IBD patients attempting a GFD
Lcerative Colitis Diet Plan
Following an Ulcerative Colitis diet plan is a bit more complicated than something like an IBS plan. The ideal diet for UC patients will vary depending on their symptom severity. For example, during flare-ups, youll want to be gentle on your intestines, eating low-fiber foods. However, when you arent having flare-ups, its healthier and more protective to feed your gut bacteria the fiber it needs.
There is a delicate balance that UC patients need to maintain, and its often a fine line with much back-and-forth from week to week. Your best option is to keep a food journal and log all of your symptoms each day. This way, you can find what works best for you. If you have any questions about how to create a food journal or about other treatments to minimize your UC symptoms, get in touch with the colorectal experts at the Colorectal Clinic of Tampa Bay.
Also Check: How Do You Get Rid Of Stomach Ulcers
Treatment For Crohns Disease
Treatments for this condition are wide ranging and include a mix of medications, treatments, and surgery. Among the most common medications are:
Antibiotics: They help heal the sores Crohnâs can cause. They may even get rid of harmful bacteria in your intestines that kick-start Crohnâs inflammation. Commonly used ones include:
- Ciproflaxin
Anti-inflammatory drugs: These drugs help ease inflammation. The two main types in use are:
- Corticosteroids
- Oral 5-aminosalicylates
Diseases Of The Digestive Tract With Different Causes
Your digestive tract must maintain a delicate balance. One that allows you to absorb nutrients from the outside world while simultaneously defending you against harmful microbes that sneak in alongside those nutrients.
To balance these two divergent needs, the thin lining that makes up the innermost part of your digestive tract is heavily guarded with lymphoid tissue and immune cells. This is meant to protect you, but in inflammatory bowel conditions, the immune cells and tissue lining your gut become unnecessarily activated creating inflammation without infection.
Pinpointing the exact cause of this inflammation can sometimes be tricky considering that Crohns disease, ulcerative colitis, and celiac disease can all have nearly identical symptoms. Lets explore exactly what these symptoms can be.1
Read Also: Ulcerative Colitis And Lactose Intolerance
Foods To Eat During Ulcerative Colitis Flares
A bland diet is best during periods of active ulcerative colitis, when you may experience abdominal discomfort, blood in your stool, loss of appetite, fatigue, weight loss, vomiting, nausea, abdominal pain, and diarrhea. A safer diet during flares might include dry toast, applesauce, and white rice. Although some foods are more likely to be safe for those with UC, individual experiences can vary, especially during flares.
Here are some safer foods to try during ulcerative colitis flares:
- Low-fiber refined grains, such as oatmeal, potatoes, and sourdough bread
- Well-cooked vegetables that are easier to digest
- Vegetable broth, which can be added to grains like rice for additional nutrients
- Fruits or vegetables that contain more soluble fiber than insoluble fiber, such as bananas, carrots, and apples
- Bland protein, such as nut butters, eggs, tofu, and chicken
Diarrhea specifically raises concerns for loss of nutrients, such as potassium, sodium, magnesium, and phosphorus, through bodily fluids. If you choose to drink an electrolyte beverage, choose low sugar versions such as G2, Propel, or BodyArmor Lyte. You can also cut regular Gatorade or BodyArmor with water, diluting it by half.
Adherence To Gfd And Correlation With Symptom Improvement
In those patients who were still following a gluten free diet , adherence was found to be excellent in 41.5%, average in 34.1%, and fair/poor in 24.4%. Excellent adherence to a GFD was associated with reduced fatigue, as compared to fair/poor adherence . Adherence was not associated with significant differences in other clinical symptoms.
Read Also: Early Symptoms Of Ulcerative Colitis
Which Foods Have The Most
When it comes to vegetables, few people are eating large quantities of the sulfur-rich types e.g. cruciferous vegetables like broccoli and Brussels sprouts.
Even if you ate the standard serving of Brussels sprouts 7 of them that equals 70 mg of sulfur.
Other common vegetables with a higher concentration are raw cabbage and boiled spinach. Those each have 90 mg of sulfur per 100g .
Those are all small amounts relative to how much there is in meats.
Theres 220 mg in the same weight of beef.
Is white meat better? Not really, as chicken comes in worse at 300 mg.
Eggs run from 150 for scrambled to 210 for fried.
White bread is comparable at 150 but then again, its processed and loaded with sulfites as a preservative.
Meats and eggs are naturally high sulfur foods, because of they contain high amounts of the amino acids:
- Methionine
- Homocysteine
- Taurine
If you suffer from ulcerative colitis or diverticulitis and want to try reducing your intake of these sulfuric aminos, consider switching out some of your meat and egg intake for plant-based proteins. On a gram for gram basis, you will see that most have lower ratios of these when comparing their amino acid profiles. Instead of whey powder, consider sprouted pumpkin seed protein.
These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
What Your Poop Says
In a study where the feces of healthy individuals was compared to those with UC, it was reported that:
Sulfate-reducing bacteria were the predominant bacterial group for UC inocula whereas they were the minority group for the healthy inocula.
Translated to plain English, those with UC had more sulfate-eating bacteria.
Unfortunately, theres no comparable data for diverticulitis.
These sulfate-reducing bacteria breakdown sulfate, which produce hydrogen sulfide.
Hydrogen sulfide is that rotten egg smell. Aside from literally being created by rotten eggs, its also what you smell from a fart. Or at least a really bad one. That hydrogen sulfide gas comes from these bacteria.
If you think the awful smell is the worst of it, think again.
In your gut, hydrogen sulfide helps to regulate inflammation and motility. If you have too much that regulation may get messed up. Its a toxin thats useful in small amounts but excess is unhealthy.
However for these bacteria in your gut to make too much of it, they need to be munching on the right fuel in the first place foods with the ingredients needed to produce hydrogen sulfide.
So what are those foods?
Sulfate-reducing bacteria growth was stimulated by peptone presumably due to the presence of sulfur-rich amino acids. The results suggest raised sulfate-reducing bacteria levels in UC, which could contribute to the condition through release of toxic sulfide.
Emphasis added. Sulfur-rich proteins!
Those are
- Homocysteine
- Taurine
Recommended Reading: Home Remedies For Stomach Ulcer In Tamil
Creamy And Greasy Food
Creamy and greasy foods containing loads of mayonnaise, butter, cream cheese, margarine, animal fat, etc. can irritate the inner lining of the colon. This can worsen the ulcers and may cause rectal bleeding. Avoid creamy pasta, macaroni and cheese, and creamy cheese containing foods to pacify your colon.
I Have Heard That Fiber Is Good For Ulcerative Colitis What Does Onpoint Say
-
We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well
-
If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently
Recommended Reading: What Is Best Medicine For Ulcer
Also Check: Foam Dressings For Pressure Ulcer Prevention
What Should I Eat If I Have Ulcerative Colitis
If you have ulcerative colitis, you should eat a healthy, well-balanced diet. Talk with your doctor about a healthy eating plan.
Ulcerative colitis symptoms may cause some people to lose their appetite and eat less, and they may not get enough nutrients. In children, a lack of nutrients may play a role in problems with growth and development.
Researchers have not found that specific foods cause ulcerative colitis symptoms, although healthier diets appear to be associated with less risk of developing IBD. Researchers have not found that specific foods worsen ulcerative colitis. Talk with your doctor about any foods that seem to be related to your symptoms. Your doctor may suggest keeping a food diary to help identify foods that seem to make your symptoms worse.
Depending on your symptoms and the medicines you take, your doctor may recommend changes to your diet. Your doctor may also recommend dietary supplements.
One Day Everything Changed
It all started back in May of 2014. I woke up one morning with slight stomach pain. I nodded it off and ignored it thinking I probably ate something wrong the night before. Little did I know at that time what was about to come. Over the next couple of months, I started having stomach pain that lasted 24/7.
By the end of June, I finally went in to see a doctor. He ran a blood test and diagnosed me with Celiac Disease . I was shocked, to say the least. If you have Celiac Disease, it means your body can no longer tolerate any amount of gluten.
My doctor said to go gluten-free immediately, and I should be fine. I was not happy about this news, but I was in so much pain I was still relieved that I might find some comfort at last. After lots of reading online, I got in my car and headed for Whole Foods. I figured out of any place this was going to be the place with the most gluten-free food.
Thankfully I only live less than a mile from one. To my surprise, there were many options, even though it might be slightly more expensive, there is almost an alternative for everything.
Over the next three weeks, I ate 100% gluten-free and still wasnt feeling any better. If anything, I was in more pain than ever. So I headed back to my primary care doctor. He said the next step was to see a Gastroenterologist .
Thankfully a coworker of mine agreed to drive me to the appointment and wait there while I was put under. They dont let you drive afterward.
Read Also: How To Eat With Ulcerative Colitis