Daily Life For People With Ibd
People with IBD lead useful and productive lives, even though they need to take medications. When they are not experiencing a flare-up of their disease, they feel quite well and are often free of symptoms.People with IBD can marry, enjoy sexual activity and have children. They can hold down jobs, care for families and enjoy sport and recreational activities.Even though there is currently no cure for IBD, medical therapy has improved the health and quality of life of most people with Crohns disease and ulcerative colitis. Research underway today may lead to further improvements in medical and surgical treatment, and even a cure.
How Is Treatment Of Crohns Disease Different From Ulcerative Colitis
Although the medications may seem similar, there are differences in how Crohns disease and ulcerative colitis are treated. Many medication classes treat both conditions, so there is a lot of overlap. However, there are enough differences that getting the right diagnosis is important. For example, people with ulcerative colitis usually take aminosalicylates, while only a limited number of people with Crohns disease will benefit from these medications. When it comes to more advanced therapies like biologic agents, some can only be used for ulcerative colitis and some can only be used for Crohns disease.
Getting the correct diagnosis can be tricky. Sometimes it might look like you have ulcerative colitis at first, but later your providers will find out that its actually Crohns disease. Work closely with them to be sure you get the right treatment.
Living With Ulcerative Colitis And Kidney Disease
If you are living with UC and kidney disease, it is important to maintain a healthy lifestyle. Many MyCrohnsAndColitisTeam members have shared their tips on how they live with UC and kidney disease. I have regular appointments with my urologist/kidney specialist to check my blood and urine, one member noted. Another said, I exercise and stay at a good weight, while a third member wrote, I try to get enough potassium and vitamin D in my diet.
Also Check: Can I Eat Eggs With Ulcerative Colitis
Don’t Miss: Nasal Cannula Pressure Ulcer Prevention
Treat To Target Disease Monitoring And Long
The treatment strategy in ulcerative colitis has evolved into a treat to target approach, in which patients are regularly assessed to ensure they are meeting strict targets for disease control. The targets for ulcerative colitis are resolution of patient reported outcomes and endoscopic remission.3 Given the importance of endoscopic healing, the colon should be directly assessed 36 months following the initiation of a new treatment.3 Flexible sigmoidoscopy is sufficient for assessing endoscopic healing.155 Patients should have a regular follow-up at a minimum of every 3 months until symptom resolution, and then at least every 612 months with the goal of maintaining tight control.3 Once patients are in remission, non-invasive markers, such as fecal calprotectin, can be used to monitor disease activity. In a post-hoc analysis of a clinical trial,156 a fecal calprotectin cutoff of 150 mg/kg was best for endoscopic remission .
Crohns & Colitis Uk Local Networks
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn’s or Colitis. All events are open to members of Crohns & Colitis UK
Recommended Reading: Can Stress Give You An Ulcer
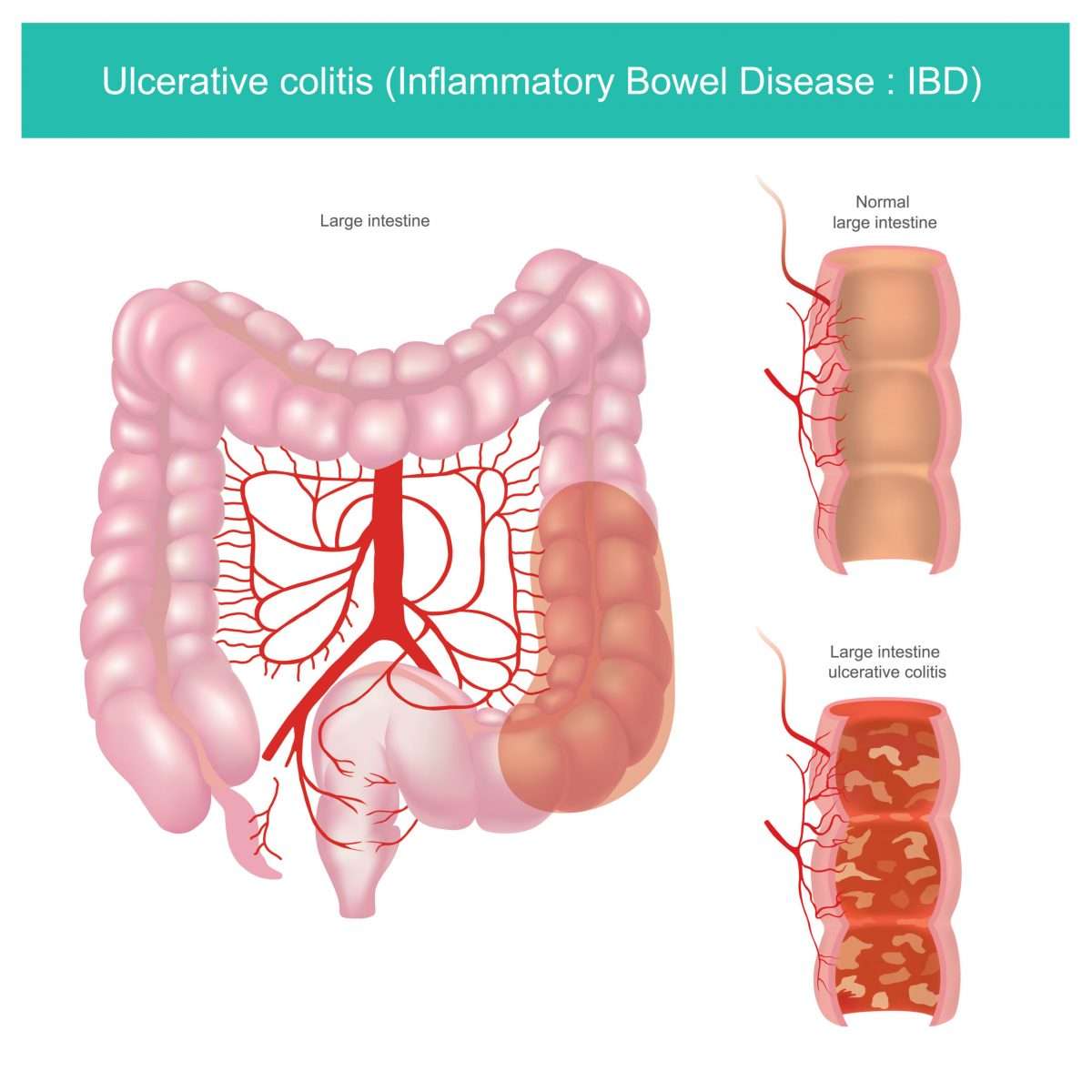
Inflammatory Bowel Disease And Colitis
Ulcerative colitis and Crohnâs disease are the two types of inflammatory bowel disease that cause colitis. Crohnâs disease and ulcerative colitis are considered autoimmune diseases .
- Ulcerative colitis always begins in the rectum and may spread to the rest of the rest of the colon, spreading from the rectum to the sigmoid, descending, transverse, and finally the ascending colon and cecum in that order. Ulcerative colitis is considered an autoimmune disease, and symptoms include abdominal pain, and bloody, diarrheal bowel movements.
- Crohnâs disease may occur anywhere in the gastrointestinal tract , including the esophagus, stomach, small intestine, and colon. In Crohnâs disease, there may be âskip lesions,â that is, abnormal segments of the GI tract interspersed with normal segments.
Both Crohnâs disease and ulcerative colitis may have other organ systems involved in addition to the gastrointestinal tract.
Either collagen or lymphocytes infiltrate into the layers of the wall of the colon, presumably as a result of inflammation. This is an uncommon illness and maybe an autoimmune disease. Diarrhea often is watery, and no blood is present in the stool.
Also Check: Can Ulcers Cause Black Stool
Treatments For Ibs And Ibd
Treatment is very different for IBS and IBD. If you have IBD, you will take medications that lower the inflammation in the GI tract such as anti-inflammatory medications, biologic agents, and immunomodulators which can reduce the damage IBD is causing.
Treatment of IBS is different. You and your providers will focus on treating the specific symptoms you are having. Changes to your diet and exercise habits are a good first step.
Heres a few examples of some foods to avoid when you have IBS:
-
Apples
If diarrhea is one of your main IBS symptoms, you might take medications that reduce the diarrhea, such as rifamixin and eluxadoline . If you are more often constipated, you might take medications that help keep the GI tract moving, such as lubiprostone , linaclotide , or plecanatide .
You might also need treatment of stress, anxiety, or depression with medications or therapy if you and your provider think this is playing a role in your IBS.
You May Like: Easy To Digest Foods For Ulcerative Colitis
How You May Feel
Ulcerative colitis attacks the lining of your digestive tract. It causes swelling and sores in the lining.
If youâve just been diagnosed with it, hereâs what might happen during a flare-up:
You might have some of those symptoms, but not all. And they may change over time. They can range from very mild to very bad.
Complications Caused By Nutritional Deficiencies
Some of the complications of malnutrition include:
- Dehydration diarrhoea causes your body to lose fluid, which can lead to dehydration. Severe dehydration can damage your kidneys.
- Anaemia reduced iron in the diet combined with losing blood from the bowel can lead to anaemia .
- Weight loss reduced appetite and poor absorption of food nutrients can cause weight loss.
- Reduced growth inadequate nutrition during childhood and adolescence can impair a childs growth and physical development.
Read Also: Average Age Of Ulcerative Colitis Diagnosis
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Also Check: How To Sleep With Stomach Ulcer
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohn’s disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
You May Like: Does Stelara Work For Ulcerative Colitis
More Evidence Ties Acne Drug To Bowel Disease
4 Min Read
NEW YORK Adding to evidence that the acne drug isotretinoin may lead to bowel disease in some users, a new study finds that patients on the medication were four times more likely than non-users to develop ulcerative colitis within a year.
Reporting in the American Journal of Gastroenterology, researchers say that the risk of any one isotretinoin user developing ulcerative colitis is likely quite small.
However, the findings do strengthen the evidence of a cause-and-effect relationship between the acne drug and inflammatory bowel disease a group of digestive disorders that includes ulcerative colitis and Crohns disease.
Isotretinoin, which is used to treat severe acne, is probably best known by the brand-name Accutane. That drug was taken off the market last year in the face of competition from generic alternatives though in pulling the medication, maker Roche Pharmaceuticals also cited costs from defending personal-injury lawsuits.
Earlier this year, the company was ordered to pay $25 million in damages to a former Accutane user who claimed that the drug caused his IBD.
The company has maintained that there is no strong evidence that the acne drug triggers IBD. Between 1997 and 2002, 83 cases of IBD among isotretinoin users were reported to the U.S. Food and Drug Administration, but that does not prove that the drug itself is to blame.
SOURCE: here 4a.html American Journal of Gastroenterology, online March 30, 2010.
What Are The Symptoms Of Ulcerative Colitis And Pancolitis
Because pancolitis is a type of ulcerative colitis , symptoms, complications and treatment of both are generally the same.
Signs and symptoms of ulcerative colitis and pancolitis may include:
- Abdominal pain
- Increased frequency of bowel movement
- Bloody stools or pus in stools
- Diarrhea that does not respond to the usual medication
- Weight loss
- Tenesmus
- Inflammation of other body partseyes, skin, etc.
Also Check: Turning Patients Every 2 Hours To Preventing Pressure Ulcers
Ulcerative Colitis Vs Crohns Disease Vs Irritable Bowel
Other gut diseases can have some of the same symptoms.
- Ulcerative colitis affects only your large intestine and its lining.
- Crohns disease causes inflammation, but it affects other places in your digestive tract.
- Irritable bowel syndrome has some of the same symptoms as UC, but it doesnt cause inflammation or ulcers. Instead, its a problem with the muscles in your intestines.
Living With Ulcerative Colitis
With careful management, most people with UC are able to enjoy life, including work, travel, recreation, sex and having children.
To keep healthy, consider:
- eating a nutritious diet to help with healing and reduce fatigue
- keeping a food diary to check if there are any foods that make your symptoms worse during a flare-up
- asking your doctor about supplements if you think you may be malnourished
- exercising regularly to lift your mood and help relieve stress
- learning some relaxation techniques to help manage stress
Recommended Reading: First Line Treatment Ulcerative Colitis
Stanford Scientists Link Ulcerative Colitis To Missing Gut Microbes
Bacteria normally inhabiting healthy peoples intestines and the anti-inflammatory metabolites these bacteria produce are depleted in ulcerative colitis patients, a Stanford study shows.
Aida Habtezion is the senior author of a study that describes how people with ulcerative colitis have insufficient amounts of a metabolite produced by a family of gut-dwelling bacteria.Steve Castillo
About 1 million people in the United States have ulcerative colitis, a serious disease of the colon that has no cure and whose cause is obscure. Now, a study by Stanford University School of Medicine investigators has tied the condition to a missing microbe.
The microbe makes metabolites that help keep the gut healthy.
This study helps us to better understand the disease, said Aida Habtezion, MD, associate professor of gastroenterology and hepatology. We hope it also leads to our being able to treat it with a naturally produced metabolite thats already present in high amounts in a healthy gut.
When the researchers compared two groups of patients one group with ulcerative colitis, the other group with a rare noninflammatory condition who had undergone an identical corrective surgical procedure, they discovered that a particular family of bacteria was depleted in patients with ulcerative colitis. These patients also were deficient in a set of anti-inflammatory substances that the bacteria make, the scientists report.
Retrograde Labeling Of Bladder Afferent Neurons
Bladder afferent neurons were specifically labeled by conventional neuronal tracing dye Fast Blue in live animals through surgery as described previously . Briefly, the rat urinary bladder was exposed with a lower abdominal incision under anesthesia . FB was injected into 10 sites in the muscular wall of the bladder to label bladder afferent neurons in the DRG. Sterilized Hamilton syringe was used for injection. To prevent leakage and labeling of adjacent tissues, a cotton swab was used, close to the injection site, to wipe off any excess dye that might leak during needle withdrawal after each injection. We also avoided to inject dyes into the lumen, major blood vessels, or overlying fascial layers. The incision was closed with 40 sutures. The surgeries were done 7 days prior to harvest of tissues. We also checked the leakage of the dyes by examining the bladder and surrounding tissues after euthanasia of the rats. No contamination was found.
Read Also: Medihoney For Stage 1 Pressure Ulcer
Also Check: Patient Education On Pressure Ulcer Prevention
How Are Skin Rashes Treated
Skin complications for people with ulcerative colitis are often improved by treating UC flare-ups as they come. One study found that symptoms of erythema nodosum in particular decreased if the underlying UC condition improved.
Many ulcerative colitis skin problems respond well to topical or oral steroids. Sweets syndrome and mild cases of pyoderma gangrenosum are often initially treated with oral or topical corticosteroids. Mouth ulcers can also be treated with topical steroid agents.
If the conditions do not respond to those medications, Humira is often the second treatment of choice. Unfortunately, one of the side effects of Humira is a rash.
Have you experienced skin rashes as a part of ulcerative colitis? Do you have any tips for dealing with them? Comment below or start a new conversation on MyCrohnsandColitisTeam.
Who Is More Likely To Have Microscopic Colitis
Anyone can develop microscopic colitis. The disease is more common in
- older adults. The average age at which people are diagnosed with microscopic colitis is 60 to 65 years.2 However, microscopic colitis may occur in people of any age, including children.
- women. Research suggests the disease is three to nine times more common in women than in men.2
You May Like: What Is Ultra Ulcerative Colitis
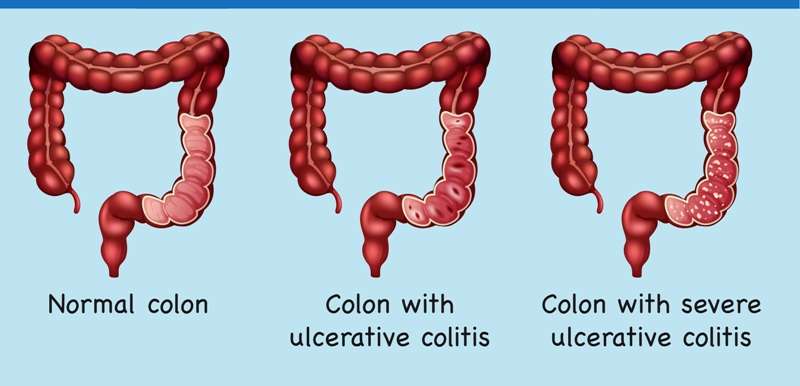
Where Inflammation Occurs
Both illnesses are caused by inflammation in the GI tract, but where the inflammation occurs can lead a doctor to the correct diagnosis. The most basic difference is that Crohns disease can involve the entire GI tract, from the mouth all the way down to the anus, whereas ulcerative colitis is restricted to the colon, says Louis Cohen, MD, assistant professor of gastroenterology at Icahn School of Medicine at Mount Sinai in New York City.
According to the UCLA Center for Inflammatory Bowel Disease, Crohn’s disease usually results in healthy stretches of the intestine between inflamed areas. People who suffer from colitis experience continuous inflammation of the colon.
What Sets Them Apart
There are three key differences:
1. Location.
Ulcerative colitis affects only the large intestine.
But in Crohnâs disease, inflammation can appear anywhere in the digestive tract, from the mouth to the anus.
2. Continuous inflammation.
People with Crohnâs disease often have healthy areas in between inflamed spots. But with ulcerative colitis, there are no healthy areas in between inflamed spots.
3. Which layers are affected.
Because Crohnâs disease affects more of the GI tract, it can cause some problems that doctors don’t usually see in people who have ulcerative colitis. For instance:
- Mouth sores between the gums and lower lip, or along the sides or bottom of the tongue.
- Anal tears , ulcers, infections, or narrowing.
Also Check: What Medicine Is Good For Ulcers
How Is Microscopic Colitis Diagnosed
During a colonoscopy, a biopsy will be taken and examined. Even if the lining of the colon looks normal, it is important to remove tissue samples for a microscopic analysis. Without these diagnostic steps, it could take weeks, months, or even years to discover the reason for the chronic diarrhea.
Once the biopsy samples are examined under a microscope, various features may reveal the source of the inflammation and pinpoint the diagnosis even further. There results of the biopsy may show the following:
- In patients with collagenous colitis, a biopsy of the colon shows inflammation and thickened tissue made from a protein called collagen. The appearance of this tissue may vary, so it is important to look at several different samples.
- In those with lymphocytic colitis, a biopsy of the colon shows an increased number of special white blood cells . A thickened band of collagen band can be seen on the biopsy, as patients can often exhibit features of both collagenous and lymphocytic colitis.