How Long Do Ulcerative Colitis Flare
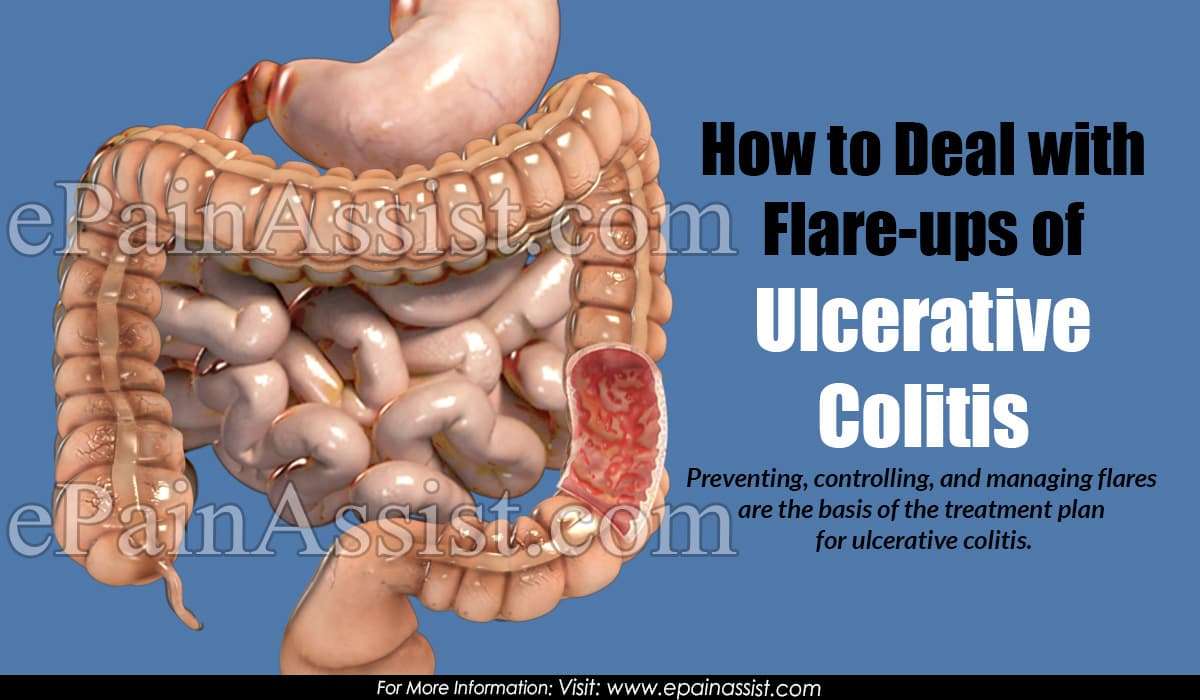
People with ulcerative colitis , a type of inflammatory bowel disease that causes inflammation and sores in the rectum and colon, experience bouts of symptoms or flare-ups, which are unpredictable and can last for days, weeks or even months. Having a treatment plan in place including medication, diet changes and flare-up reduction methods could help shorten a flare.
Ulcerative Colitis: When To Call
if you have been diagnosed with ulcerative colitis and you have:
- Fever over 101°F or shaking chills.
- Lightheadedness, passing out, or a rapid heart rate.
- Stools that are almost always bloody.
- Severe dehydration, such as passing little or no urine for 12 or more hours.
- Severe belly pain with or without bloating.
- Pus draining from the area around the anus or pain and swelling in the anal area.
- Repeated vomiting.
- Not passing any stools or gas.
If you have any of these symptoms and you have been diagnosed with ulcerative colitis, your disease may have become significantly worse. Some of these symptoms also may be signs of toxic megacolon. This is a condition in which the colon swells to many times its normal size. It requires emergency treatment. Left untreated, it can cause the colon to leak or rupture. This can be fatal.
People with ulcerative colitis usually know their normal pattern of symptoms. Call your doctor if there is a change in your usual symptoms or if:
- Your symptoms become significantly worse than usual.
- You have persistent diarrhea for more than 2 weeks.
- You have lost weight.
What Is A Uc Flare
A UC flare is an acute worsening of the symptoms of bowel inflammation. Flares may occur weeks, months, or even years apart, with different levels of severity.
Medication, your lifestyle, diet, and other factors may contribute to flare-ups. In the same way, taking all prescribed medications, eating balanced meals, and avoiding known triggers can often help prevent flares.
Ulcerative colitis symptoms change based on the severity of a flare-up and the location of inflammation in the intestine. Symptoms often include:
- moderate to severe abdominal pain or cramps
- persistent bowel movements
Also Check: What Foods Should Be Avoided With Stomach Ulcers
When Youre In The Hospital
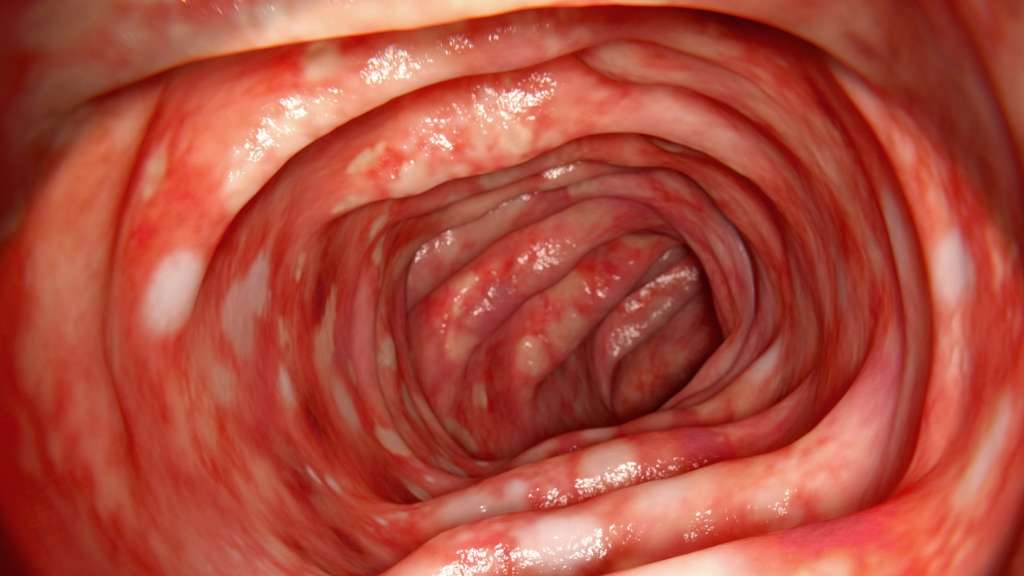
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
Also Check: New Meds For Ulcerative Colitis
Give Yourself Some Tlc
Stress doesn’t cause UC, but it makes symptoms and flares worse for some people. If it affects you, try meditation, breathing exercises, or a massage. You could also see a pro to try biofeedback, hypnotherapy, or a type of counseling called cognitive behavioral therapy, which helps you learn new ways to handle problems. Being active helps, too. Try yoga, tai chi, or other low-impact exercises like walking.
10
Also Check: How To Test For Ulcerative Colitis
Managing Ulcerative Colitis Flare
Ulcerative colitis is a form of inflammatory bowel disease that affects the mucosal lining of the large intestine and rectum, causing inflammation and ulcers in the digestive tract. People with ulcerative colitis experience periods of remission, during which symptoms subside, and flare-ups, during which symptoms return or worsen.
The symptoms of an ulcerative colitis flare may vary depending on the severity of the inflammation and where it occurs. Generally, the most common symptoms of UC flares are abdominal pain, cramping, and diarrhea . Most people with ulcerative colitis experience mild to moderate symptoms, while others may have more serious symptoms, including fever, severe abdominal cramping, and bloody stools.
Flares can be difficult to manage and may interfere with day-to-day life. Luckily, there are ways to manage these symptoms both with your doctor and at home.
Easing Symptoms During A Flare
The below suggestions can also help ease symptoms or help keep your body healthy during a flare-up.
Drink water: In UC, the large intestine can have a hard time absorbing water and salt, which can contribute to diarrhea and dehydration. Drinking plenty of water or an electrolyte replacement drink can help avoid dehydration if you’re experiencing a flare.
Eat plain, easy-to-digest foods: During a UC flare, it’s common to lose your appetite. To keep your energy levels up and avoid malnutrition and weight loss, it’s important to continue to fuel your body with food. Unfortunately, fruits and vegetables, particularly when raw, are bothersome for many people with UC. Avoid fatty and greasy foods as well. Your doctor may also suggest meal replacement drinks if you’re losing weight from UC flare-ups.
Get some exercise: If you’re experiencing symptoms like stomach pain and diarrhea, exercise may sound like the last thing you want to do. But in addition to the well-known mood and health-boosting benefits of exercise, a workout can also have specific benefits for UC symptoms. Uncontrolled inflammation in the intestinal tract leads to UC symptoms. Exercise has an anti-inflammatory effect that can help these symptoms.
Also Check: I Think I Have Ulcerative Colitis
How Can I Be Sure Its An Ulcer
The only way to be sure an ulcer is causing your discomfort is with a medical diagnosis. We will evaluate your medical history and conduct a thorough physical examination.
To determine the root cause of your ulcer, we may run blood, stool, or breath tests. These tests are designed to look for signs of helicobacter pylori, the bacteria linked to ulcers.
Depending on your unique symptoms, we may also order an endoscopy. During an endoscopy, we insert a tube with a tiny camera down your throat and into your stomach to take pictures of any potential damage and collect tissue samples for analysis.
What To Eat During A Ulcerative Colitis Flare
Research shows that nutrition cant cause or cure ulcerative colitis. There are no foods that can cause someone to develop ulcerative colitis, and there is no miracle diet that will cure people of the condition. However, good nutrition does play an important role in the management of ulcerative colitis symptoms, especially during a flare.
Ulcerative colitis flare-ups are uncomfortable and frustrating. Pain, bloating, cramping, fatigue, rectal bleeding, and diarrhea are common symptoms during flare-ups. If youre in the midst of the flare, changes in your diet can help control your symptoms and allow your intestine time to heal. If you have a flare
While carefully watching what you eat can help ease symptoms of ulcerative colitis, there are very few treatments for ulcerative colitis currently available. Participating in research is one of the best ways to actively search for a cure. Research helps increase the understanding of ulcerative colitis and trial new treatment options.
If you or a loved one has ulcerative colitis, fill out the form below to learn more about a clinical trial that you may qualify for.
Recommended Reading: Ulcerative Colitis And Lung Disease
You May Like: How To Treat Ulcerative Colitis Pain
How Do I Know If My Uc Has Gone Into Remission
UC doesn’t have a cure. Instead, the goal of any treatment plan is to send the disease into remission.
When UC is in remission, you don’t experience as many symptoms and start to feel better. If your UC medications and lifestyle changes work well for you, remission may last for months or even years. There are several different kinds of remission:
- Clinical remission: When a patient isn’t experiencing symptoms and may feel better.
- Endoscopic remission: Testing of the intestinal lining shows no inflammation
- Biochemical remission: Blood and stool tests show no sign of inflammation
- Surgical remission: When UC goes into remission after surgery to treat it
- Histologic remission: When both clinical and endoscopic tests didn’t show signs of UC
With UC, it can feel like life revolves around symptoms. If UC symptoms keep coming back, it can be a sign that medications aren’t working. Consider taking part in a clinical trial researching an investigational treatment option for people living with UC.
Medications For Other Conditions
A medication you take for another condition can also trigger a flare-up.
This might happen if you take an antibiotic to treat a bacterial infection. Antibiotics can sometimes disrupt the balance of intestinal bacteria in the gut and cause diarrhea.
Certain over-the-counter nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen , may also irritate the colon and cause a flare-up.
This doesnt mean you should stop taking antibiotics or pain medications, but you should speak with your doctor before taking these drugs.
If you take an antibiotic, you may also need a temporary antidiarrheal medication to combat possible side effects.
If you experience stomach pain after taking an NSAID, your doctor may suggest acetaminophen to reduce pain instead.
Recommended Reading: How To Use Aloe Vera Gel For Ulcerative Colitis
How Are Peptic Ulcers Treated
The goals of treatment for peptic ulcers are:
- relieve symptoms quickly
- heal the ulcer
- prevent it from recurring in the future
Treatment of a helicobacter pylori infection is now recognized as the most important aspect of treatment. All ulcer patients who are infected with bacteria should be offered antibiotic therapy. Usually this requires a combination of drugs for which many different combinations are available. Usually an acid-suppressing drug is necessary to relieve symptoms and induce ulcer healing, but also to boost the effects of the antibiotics. At the same time, two antibiotics are usually necessary to ensure successful eradication of the infection.
This triple therapy is usually taken for one to two weeks and is 8090% successful in getting rid of the infection. Symptoms may take longer to disappear completely, but when they do there is little need to perform further tests to ensure that treatment has worked.
Patients who have had serious complications from their ulcer should undergo repeat testing to ensure that the treatment is successful. For patients whose infection persists after antibiotic therapy, second line therapy is usually given and is successful most of the time. A few patients fail this therapy and require long term acid-suppression therapy to prevent ulcer recurrence.
What Can Affect Ulcerative Colitis Flare

The concrete reasons causing the UC flare-up are still unknown. For some people, the effects might be visible in only a small section, but for a few, it might spread through the entire colon. However, certain factors that might trigger the flare-ups are:
- Smoking Cigarettes are not only one of the major factors that cause UC, but also can cause flare-ups.
- Food that irritates the GI tract There is evidence that food can cause UC or flare. Consuming certain foods during a flare-up can aggravate the symptoms.
- Unnecessary Medication Flare-up can be a result of intake of unprescribed over-the-counter drugs. Nonsteroidal anti-inflammatory drugs like Aspirin, Naproxen, Ibuprofen, and others can worsen the flare-up symptoms.
- Stress Emotional or physical stress doesnt cause ulcerative colitis directly, but it does affect the digestive process and hence contributes to the worsening of flare-ups.
Read Also: What Should You Eat With Ulcerative Colitis
Understanding Ulcerative Colitis Flare
A flare-up is the reappearance of disease symptoms. And for people living with ulcerative colitis , an inflammatory bowel disease , flare-ups can be unpredictable, lasting hours, days, or weeks.
- Frequent and/or urgent bowel movements
- Diarrhea
- Lack of appetite
- Joint and body aches
Because these symptoms may also be caused by something other than UC, it can sometimes be difficult to tell whether you’re experiencing a flare-up. Below, we look at factors that might affect a UC flare-up, and what can help if you are experiencing a UC flare-up.
Ways To Manage Symptoms And Flares Of Ulcerative Colitis
A flare of ulcerative colitis can be painful and embarrassing not only for you, but for those around you. Once you have one flare, are you going to have more? That anxiety can make you feel even worse and trigger one. Lets investigate 6 ways to manage symptoms and flares of ulcerative colitis.
Also Check: New Meds For Ulcerative Colitis
How Is Ulcerative Colitis Treated
Treatment for UC depends on the severity of the disease and often involves both medications and lifestyle modifications.
Medications
Most people require a combination of medications to suppress and/or modulate the immune system:
- Anti-inflammatory drugs: Anti-inflammatory drugs such as 5-aminosalicylates and corticosteroids suppress the cells that cause inflammation. These drugs are usually the first step in the treatment of UC and are well tolerated by most people.
- Immune system suppressors: Immunosuppressant drugs work by suppressing the immune system response that stimulates the inflammation process. Examples include Azasan and Imuran Purinethol and Purixan Gengraf, Neoral and Sandimmune and Xeljanz .
- Biologics : Biologics target and neutralize proteins produced by the immune system. Examples include Remicade , Humira and Simponi . Entyvio is a type of biologic that works by blocking the inflammatory cells from reaching certain parts of the body, and can be used for people who cant tolerate other biologics.
- Anti-diarrheal medications: Your doctor may recommend anti-diarrheal medications such as Imodium for severe diarrhea. You should avoid taking over-the-counter anti-diarrheal medications without consulting your doctor, because they can increase the risk of toxic megacolon .
- Painkillers: Tylenol is safe to use for pain relief. Talk to your doctor before taking other OTC pain medications.
- Antispasmodic medications: Antispasmodic medications can help reduce cramps.
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Don’t Miss: Best Acid Reducer For Ulcer
Symptoms Of Ulcerative Colitis
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience fatigue , loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is. For some people, the condition has a significant impact on their everyday lives.
What To Look For In A Meal Kit
While food triggers vary by person, Kennedy recommends looking for meals with soluble sources of fiber, which tend to be easier to digest and cause less inflammation in the digestive tract.
Things like white rice are minimally processed but still a great source of soluble fiber are great to look for, as are fruits and vegetables that either have the skin removed or can be removed during the prep process, she says.
But the general rule of thumb, says Kennedy, is that whatever meal delivery kit you choose, always opt for foods in their purest, most whole forms. The key is to find meals that use minimally processed foods, and preferably whole foods all together.
Heres a peek at the best meal delivery options for people with ulcerative colitis.
Recommended Reading: Treating Ulcers In Horses With Omeprazole
You May Like: Best Treatment For Ulcerative Colitis Flare Up
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
List Of Foods To Eat To Keep Colitis From Flaring Up
Colitis is an inflammatory bowel disease. There are several types of colitis, depending on the location of the inflammation. Symptoms vary but commonly include abdominal cramps, bloating, constipation and diarrhea. Theres really no nutritional therapy for colitis, nor is there a cure. But learning to strike a balance between getting the nutrients you need and avoiding the foods that seem to trigger your symptoms can help you manage the condition.
Video of the Day
Read Also: Can You Take Tylenol With Ulcerative Colitis
You May Like: What To Put On Leg Ulcers
What Is The Treatment For Peptic Ulcers
The choice of treatment depends on whether or not the ulcer is caused by infection with H pylori. Correct diagnosis is key to whether a treatment works or not. If the bacteria are the cause, treatment focuses on killing the infection. Regardless of whether the bacteria are the cause, reducing acid in the stomach is another important focus of treatment.
The following treatments are recommended for ulcers:
- Lifestyle changes: Quit smoking, avoid alcohol, aspirin, and NSAIDs
- Acid-blocking medications
- Medications that protect the lining of the stomach and duodenum
- Triple-therapy or dual-therapy regimens for ulcers caused by H pylori
No single medication works to get rid of H pylori infection. Two combinations have been found that work well in most people.
These treatments are generally given for two weeks.
Once H pylori bacteria are eradicated from a persons digestive tract, usually it will not come back. The ulcers usually heal completely and do not return.
Treatment for bleeding ulcers depends on the severity of blood loss and includes:
It is important to remember that treatment may not work if the diagnosis is not correct. If the doctor diagnoses an ulcer, it is important to determine whether the ulcer is caused by infection with H pylori.