Diagnostic And Differential Diagnostic Value
Previous studies have valued the usefulness of routine laboratory testing in UC. CRP is a helpful index of UC activity, but its utility, as a screening test has not been totally evaluated.
CRP is the most sensitive compared to other serologic markers of inflammation in adult population for detecting IBD. The sensitivity of CRP ranges from 70%-100% in the differential diagnosis between CD versus irritable bowel syndrome and from 50%-60% in UC. In high percentage of paediatric patients, the sensitivity of routine testing , varies from 62%-91% when evaluating the combination of 2 routine laboratory tests, whereas specificity ranged from 75%-94%.
Levels of CRP are higher in active CD than in UC and this difference might be used to differentiate between CD and UC. The measurements of circulating levels of CRP, ESR, platelets count are not useful at all for differentiation between both types of IBD.
Orosomucoid is not useful test for screening healthy populations or differentiating patients with inflammatory vs functional disorders.
The clinical usefulness of pANCA or ASCA testing in patients with non-specific gastrointestinal symptoms is limited, because of the low sensitivity. Assaying all the serum markers available for CD, the sensitivity for the diagnosis of CD is greater than 80% and the positive predictive value is over 90% but only when the prevalence of CD is > 38%.
When Should Uc Complicated By Cmv Infection Be Suspected
Although patients with UC may require early diagnosis and appropriate treatment of CMV infection, CMV may become sporadically reactivated in such patients and then disappear even without prescription of antiviral agents. Matsuoka et al. assayed CMV levels at 2-week intervals for 8 weeks in 69 patients with severe UC to assess CMV reactivation. Such reactivation was diagnosed by CMV antigenemia or CMV PCR . Forty-eight patients were positive for CMV IgG, and half showed evidence of CMV reactivation. No significant difference in the rate of either remission or colectomy was evident between the CMV reactivation and the other group reactivation resolved without antiviral therapy in most patients. do Carmo et al. found that it was rare for patients with IBD to develop an active CMV infection . Therefore, blood tests exploring CMV infection status need not be performed in all IBD patients.
Recently reported risk factors for CMV disease in IBD patients include age > 30 years, immunomodulatory treatment, and refractoriness to drugs such as corticosteroids or TNF antagonists . Another study found that a leukocyte count < 11,000/mL and a disease duration < 60 months were risk factors for CMV infection, in addition to age 30 years and immunosuppressant use . Thus, CMV infection status should be determined in older UC patients who are refractory to immunomodulators such as high-dose steroids, or whose symptoms persist or deteriorate as the steroid dose is reduced.
Microscopic Featuresappraisal Of The Diagnosis
4.3.1 Early stage disease
It has been proposed that a non-specific increase in the inflammatory infiltrate in the lamina propria in combination with absent crypt architectural distortion, indicates a diagnosis of acute, infective colitis, rather than UC. This finding, however, is not confirmed in those studies of patients with early onset colitis .,
Basal plasmacytosis at the initial onset has a high predictive value for the diagnosis of IBD Repeat biopsies after an interval may help to solve differential diagnostic problems and establish a definitive diagnosis especially in adults, by showing additional features
Basal plasmacytosis is observed in biopsies obtained at early onset in 38100% of adult patients, and can help differentiate between UC and infectious colitis. It is particularly a feature in young children in these cases it is notably present in rectal biopsies and decreases proximally. It is an early feature, sometimes the first lesion to appear,,,, and a good predictive marker.
In young children or patients with an aberrant presentation of colitis, UC should always be considered in the differential diagnosis even if the pathology is not typical
Reliable diagnostic features may be absent from biopsies obtained in early onset disease, in acute severe colitis, or in patients with an atypical immunological response . The routine use of additional techniques such as immunohistochemistry is not recommended at present.
4.3.2 Established disease
Recommended Reading: What Are The First Signs Of A Stomach Ulcer
Tests And Investigations For Ibd
- Our information
- Tests and Investigations for IBD
This information looks at some of the medical tests and investigations you may be offered if your doctor suspects you have Ulcerative Colitis or Crohns Disease . The results from these tests can help ensure that you are given a correct diagnosis, and that your treatment is based on good quality information.
As hospital procedures vary, this leaflet is only a general guide to the tests and investigations you might have. For more detailed information about the tests, talk to your doctor or specialist IBD team. They will be happy to help with any queries or concerns. You may also find that the hospital or clinic has its own information sheets about specific tests and procedures. You could also contact our Crohns & Colitis UK helpline or visit our website for further help.
You will probably only need to have some of the tests listed in this information sheet, and you are unlikely to have them all at once. However, Crohn’s and Colitis are fluctuating, ongoing condition and it is likely that you will need to have some of the tests repeated from time to time. After your initial diagnosis, further tests may be needed to determine which treatments are most suitable for you, how well you are responding and whether your disease is in remission.
Diagnosed with Colitis in 2011
Diagnosed with Crohn’s in 2007
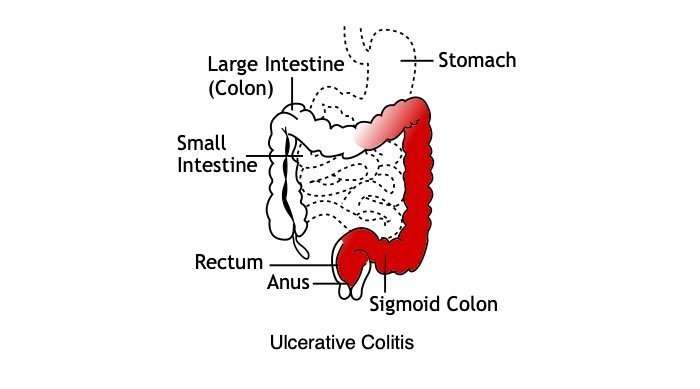
Ulcerative Colitis Is A Type Of Ibd
There are two main types ofinflammatory bowel diseases ulcerative colitis andCrohns disease. Ulcerative colitis is more common worldwide than Crohns disease.
It causes inflammation and sores in the large intestine and may affect part or all of the large intestine.
Ulcerative colitis can happen at any age, but it is more likely to develop in people between the ages of 15 and 30, or older than 60 years of age.
Ulcerative colitis needs to be diagnosed by a health care provider. While there are no cures, there are treatments.
You May Like: How Do I Get Rid Of A Stomach Ulcer
Treatment Of Ulcerative Colitis
Ulcerative colitis is a chronic condition that requires proper treatment to reduce inflammation and prevent the symptoms from worsening.
Several drugs and medications are used to treat UC. The type depends upon the severity of the condition. A medication that works for someone may not work for other people, so sometimes it takes time to identify a proper medication that helps you.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Read Also: Offloading The Diabetic Foot For Ulcer Prevention And Healing
Immunomodulators In The Treatment Of Cmv Colitis
The continued use of immunomodulators, including corticosteroids, thiopurines, and biologics, during antiviral therapy for CMV remains controversial. The European guideline recommends that cessation of all immunomodulatory therapies, including steroids, should be considered until the CMV colitis symptoms are controlled, and that no immunomodulator should be prescribed for patients with systemic CMV disease . However, the evidence level for these recommendations is 5 . Ciccocioppo suggested that steroids should be quickly tapered and discontinued, but immunosuppressants and biological agents with long-lasting effects should be maintained in patients with viral colitis and those exhibiting reactivation of latent infection . On the other hand, it has been suggested that any already initiated IBD treatment should be continued during antiviral therapy for CMV colitis . Sager et al. proposed that conventional corticosteroid therapy should be combined with antiviral therapy, and medical rescue therapy using immunosuppressants should be prescribed when necessary. Therefore, additional studies are required to explore the effects of immunomodulators employed to treat UC complicated by CMV colitis.
Several studies have shown that ganciclovir is essential for patients with steroid-refractory or -dependent UC and histologically high-grade CMV infections. Concomitant anti-TNF therapy to treat the UC may also be appropriate .
Questions To Ask Your Health Care Provider
- How often do I need to see a gastroenterologist?
- How often do I need to undergo testing?
- What are my risks for colon cancer?
- Are there symptoms that should cause worry? If so, what are they?
If you dont know something at any point, ask for more information! For some, hearing that they have ulcerative colitis is a relief, a reason for symptoms and a light at the end of the tunnel. For others, it can be scary and daunting. Many will have a mix of feelings.All of this is completely normal.
Don’t Miss: Does Ulcer Pain Come And Go
Endoscopy Of The Large Intestine
Doctors order endoscopy of the large intestine with biopsies to diagnose ulcerative colitis and rule out other digestive conditions. Doctors also use endoscopy to find out how severe ulcerative colitis is and how much of the large intestine is affected.
During an endoscopy, doctors use an endoscopea long, flexible, narrow tube with a light and a tiny camera on one endto view the lining of the large intestine. Doctors obtain biopsies by passing an instrument through the endoscope to take small pieces of tissue from the lining of your rectum and colon. A pathologist will examine the tissue under a microscope.
Two types of endoscopy used to diagnose ulcerative colitis are
- colonoscopy, in which a doctor uses a type of endoscope called a colonoscope to view the lining of your rectum and your entire colon
- flexible sigmoidoscopy, in which a doctor uses a type of endoscope called a sigmoidoscope to view the lining of your rectum and lower colon
Family And Medical History
A physical examination can involve:
- checking the persons blood pressure, temperature, and heart rate
- listening to the persons stomach with a stethoscope
- checking for tenderness or lumps by pressing on the persons stomach
Sometimes, the doctor may also carry out a digital rectal examination. This means gently inserting a lubricated finger into the rectum to check for signs of ulcerative colitis.
You May Like: Can Diverticulitis Cause Ulcerative Colitis
How An Intolerance Test Can Help Ulcerative Colitis
A 2018 Chinese study saw that a food intolerance test helped patients improve their ulcerative colitis symptoms markedly. The researchers used an IgG test to inform an elimination diet for patients to follow, and compared to a control group who followed a normal healthy diet, saw a noticeable improvement in symptoms.
After intervention, the Mayo score was significantly lower in the intervention group than in the control group . The number of patients with extra-intestinal manifestations decreased from 7 to 2 in the intervention group and from 6 to 5 in the control group.
How Do Doctors Diagnose Ulcerative Colitis
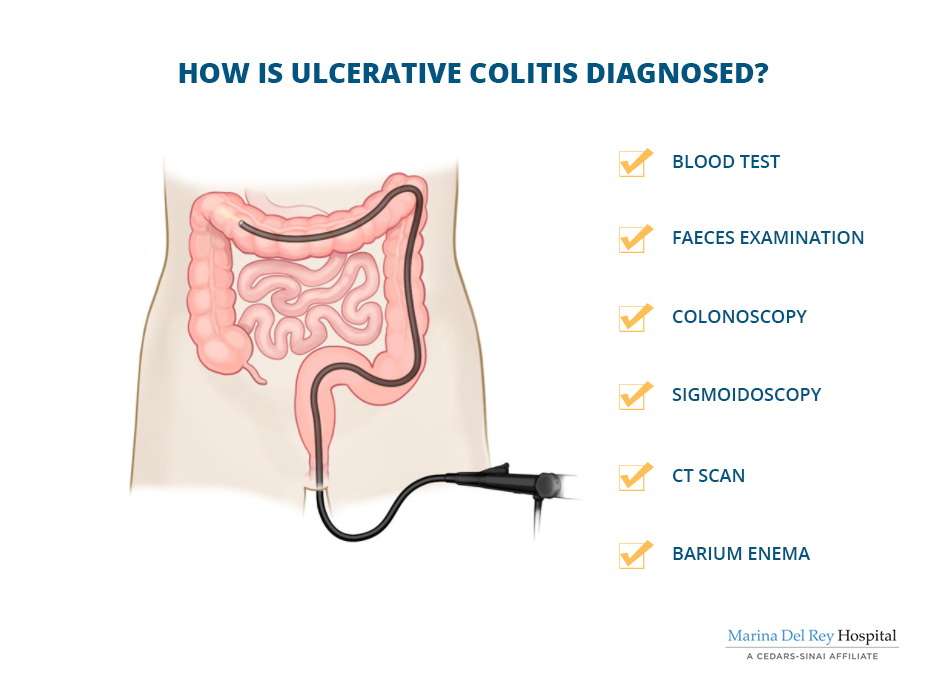
To diagnose ulcerative colitis, doctors review medical and family history, perform a physical exam, and order medical tests. Doctors order tests to
- confirm the diagnosis of ulcerative colitis
- find out how severe ulcerative colitis is and how much of the large intestine is affected
- rule out other health problemssuch as infections, irritable bowel syndrome, or Crohn’s diseasethat may cause symptoms similar to those of ulcerative colitis
Read Also: Wound Vac For Pressure Ulcers
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Ulcerative Colitis Diagnosis And Testing
The path to receiving a chronic disease diagnosis can be overwhelming and even frightening at times. The best thing you can do during this time is be educated and prepared. We can help you understand the process of diagnosing ulcerative colitis and learn about common procedures your healthcare team may recommend.
An ulcerative colitis diagnosis is based on several factors, including your medical history, a physical exam, and a series of medical tests. The tests your doctor recommends will help your healthcare team determine if you have ulcerative colitis and which type of ulcerative colitis you have.
Also Check: Best Ulcerative Colitis Diet Book
Getting Tested For Ulcerative Colitis
There are many tests your gastroenterologist can do to find out if you have ulcerative colitis. First, he or she will take your past health and family health info, listen to your symptoms, and do an exam to feel and listen to your belly. No one test makes the diagnosis, but testing is used to confirm the gastroenterologists clinical suspicion that ulcerative colitis is causing symptoms.
Ulcerative colitis is diagnosed by the presence of the common symptoms and endoscopic and biopsy findings of long-term inflammation in the large intestine.
Talk to your doctor about which test is best for you. Your doctor will tell you how to get ready for your test for ulcerative colitis.
This testcan be done in a doctors officeand does not need anesthesia or sedation .
Sigmoidoscopy is a test during which a doctor uses a short, thin , flexible tube with a tiny camera on the end tocheck the rectum and the lower end of the colon for polyps and cancer. Only the final two feet of the colons six feet are examined.
Introduction of the flexible tube may be somewhat uncomfortable, and some cramping may happen during the test.
You will need to take a couple of cleansing enemas before the testand/or a gentle oral prep.
You may be given medicine to make you relaxed and sleepy during this test.
After the test, there may be some mild belly-gas pains.
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Recommended Reading: How To Check A Horse For Ulcers
Surgery For Ulcerative Colitis
Even with the availability of medicines to treat ulcerative colitis, surgery may still be needed to manage the disease. There are a few types of surgery that your gastroenterologist with discuss with you.
Proctocolectomy
Removes the colon and rectum. Sometimes ileostomy is also done at this time, which is a procedure that brings the ileum, or end of the small intestine, through an opening in the abdominal wall to allow intestinal waste to drain out of the body. After the procedure, the patient wears an external bag over the opening to collect waste.
Restorative proctocolectomy
Removes the colon and rectum but allows the patient to continue to pass stool through the anus.
Before having surgery for ulcerative colitis, it is important to understand what the aim of the surgery is, what will happen during the procedure and the length of the recovery period. Patients with ulcerative colitis having surgery should speak to other patients who have had the procedure. Previous patients are often very willing to share their experiences and add perspective.
Diagnosing Inflammatory Bowel Disease In Adults
In inflammatory bowel disease, or IBD, there is persistent inflammation in the gastrointestinal tract. The condition causes symptoms such as abdominal pain, diarrhea, bloody stool, constipation, and an urgent need to have a bowel movement. The most common types of IBD are Crohns disease and ulcerative colitis.
Gastroenterologists at NYU Langone’s Inflammatory Bowel Disease Center are experts in the gastrointestinal tract and can recommend the appropriate diagnostic tests to determine the cause of your symptoms. There is no single definitive test to confirm the presence of IBD, so the condition is diagnosed based on a combination of tests, including endoscopy, biopsy, and imaging tests.
You May Like: What Are Some Symptoms Of An Ulcer
Prognosis For Ulcerative Colitis
Usually, ulcerative colitis is chronic with repeated exacerbations and remissions. In about 10% of patients, an initial attack becomes fulminant with massive hemorrhage, perforation, or sepsis and toxemia. Complete recovery after a single attack occurs in another 10%.
Patients with localized ulcerative proctitis have the best prognosis. Severe systemic manifestations, toxic complications, and malignant degeneration are unlikely, and late extension of the disease occurs in only about 20 to 30%. Surgery is rarely required, and life expectancy is normal. The symptoms, however, may prove stubborn and refractory. Moreover, because extensive ulcerative colitis may begin in the rectum and spread proximally, proctitis should not be considered localized until it has been observed for ⥠6 months. Localized disease that later extends is often more severe and more refractory to therapy.
Causes Of Ulcerative Colitis Flares
Ulcerative colitis flares can be caused by a variety of things, including:
- Skipping medications or not taking the correct dose. If you regularly take medicine for your ulcerative colitis, you need to be consistent even when your disease is in remission. If you dont follow prescription instructions, flares can occur.
- Taking non-steroidal anti-inflammatory drugs. Common drugs like aspirin, naproxen, and ibuprofen can inflame the bowel and bring on serious symptoms. If you need mild pain relief or fever treatment, you should take acetaminophen.
- Taking antibiotics. Although theyre useful when you have bacterial infections, they affect the bacteria that live in your intestine. These changes can result in diarrhea or the growth of too much of a certain bacteria that then causes inflammation. If you have a bacterial infection, make sure your healthcare provider knows you have ulcerative colitis.
- Not managing stress. Physical and emotional stress can bring on flare-ups. Once you understand that stress causes such a reaction, you can find out what stress management strategies work to keep flare-ups at bay.
- Eating and drinking triggering items. The foods and drinks that bring on symptoms vary by person. Youll need to track your diet so you can pinpoint triggering items when you experience ulcerative colitis flares.
Read Also: Yea Sacc For Horses With Ulcers