Squeeze More Exercise Into Your Daily Routine
Exercise has many benefits for your physical and mental health. And it can help you manage the anxiety and stress associated with ulcerative colitis.
Gentle exercises like walking and yoga are exceptionally helpful. Research has shown that exercise in conjunction with other interventions like medication helped to reduce symptoms, improve immunological response, and improve nutrition levels.
Other low-intensity options include swimming, biking, and gentle stretching.
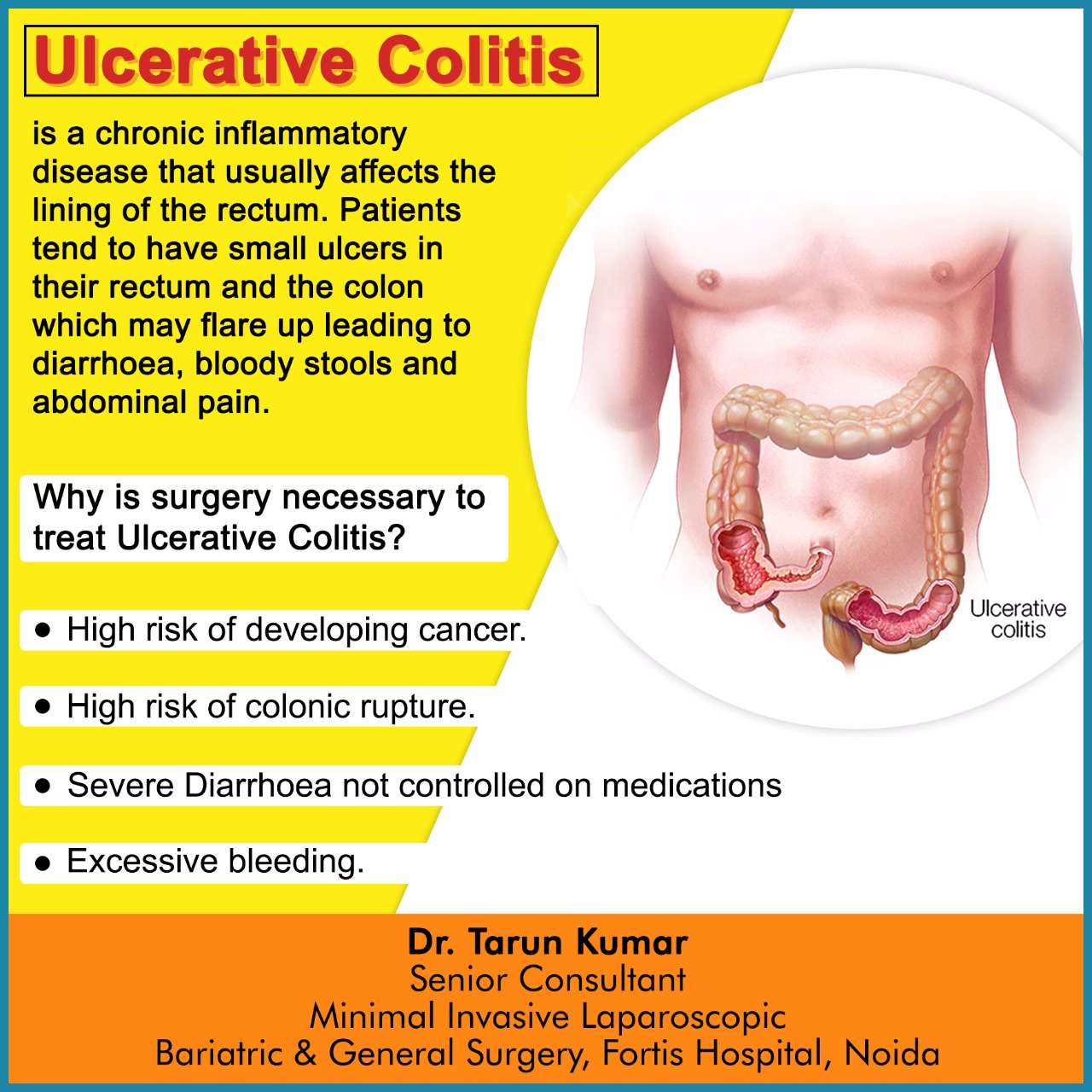
What Is Ulcerative Colitis
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
The inflammation in ulcerative colitis usually starts in the rectum, which is close to the anus . The inflammation can spread and affect a portion of, or the entire colon. When the inflammation occurs in the rectum and lower part of the colon it is called ulcerative proctitis. If the entire colon is affected it is called pancolitis. If only the left side of the colon is affected it is called limited or distal colitis.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medication such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. However, more severe flare-ups need to be treated in hospital to reduce the risk of serious complications, such as the colon becoming stretched and enlarged or developing large ulcers. Both of these can increase the risk of developing a hole in the bowel.
If medications aren’t effective at controlling your symptoms, or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
During surgery, your small intestine will either be diverted out of an opening in your abdomen , or used to create an internal pouch that’s connected to your anus .
Read more about:
Read Also: Food For Ulcer Patient In Nigeria
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- feeling tired
- dehydration
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Alcohol And Ulcerative Colitis Flare
Common effects of alcohol can exacerbate IBD symptoms and contribute to the worsening of your condition. One study has found about 75 percent of people reported a worsening of IBD symptoms after consuming alcohol.
Certain properties of alcohol are likely responsible for the increased risk of IBD flare-ups. For example, alcohol is a natural diuretic that can leave you dehydrated and cause diarrhea by stimulating the intestines. Carbonated alcohol beverages can cause you to be gassy. A healthy balance of bacteria in the gut is important for normal digestive functions, but alcohol can disrupt the amount, diversity, and balance of bacteria in your GI tract. Alcohols irritation of the GI tract lining can also lead to rectal bleeding and poor nutrient absorption in some people.
Studies have shown that alcoholic beverages that contain a large amount of sugar, in particular, may increase abdominal pain and discomfort among people who have UC. A MyCrohnsAndColitis team member noticed the same effect with sugar, stating that Sugar in alcohol gets me every time. Sparkling wine is reported to be well-tolerated by people with ulcerative colitis, compared to other alcoholic beverages.
The consumption of red wine has also been linked to long-term risk for relapse and flare-ups in people with inactive UC due to an increase in permeability in the intestines.
- Anemia
- Gastritis
- Malnutrition
Read Also: Over The Counter Meds For Ulcers
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Are Your Ulcerative Colitis Symptoms Under Control
She emphasizes that your doctor will likely be just as focused on ensuring your treatment also leads to endoscopic remission and histologic/deep remission .
Studies show that those who are in endoscopic and deep remission do best long term, as far as lower chances of hospitalizations for flare-ups and lower chances of complications, including surgery, she says.
Still, your doctor will also recommend that when you do feel your digestion is off that you recognize it and react as quickly as possible.
Pay extra attention if you are exposed to any potential ulcerative colitis triggers. For example, some common medications may prompt flares. The two biggest culprits are antibiotics and nonsteroidal anti-inflammatory drugs , such as ibuprofen, aspirin, and naproxen. Other triggers may include stress and foods that aggravated your symptoms in the past.
Recommended Reading: How To Soothe Mouth Ulcers
What Are The Common Side Effects Of Ulcerative Colitis Medication
All ulcerative colitis medications may have side effects, but these side effects will differ depending on the drug. This is not a complete list, so please talk to a healthcare provider about any questions you have about possible side effects, drug interactions, or any other concerns.
Aminosalicylates are the first-line treatment for ulcerative colitis because they are generally safe medications with few side effects. Side effects are usually limited to headache, abdominal pain, nausea, and loss of appetite. Sulfasalazine, however, is a sulfa drug, so it should not be taken by people with allergies to sulfa drugs.
Topical corticosteroids such as rectal suppositories, creams, or foams usually have few or only mild side effects. They most commonly provoke site reactions such as burning, irritation, and itching. Oral and injected corticosteroids, however, may produce side effects in many people including mood and behavior changes, increased appetite, weight gain, high blood pressure, high blood sugar, acne, thinning skin, fluid retention, and cataracts.
Immunosuppressants can weaken the immune system and decrease the bodys production of white blood cells that serve as the front-line defense against infection and cancer. The most serious side effects of immunosuppressants, then, are potentially severe infections and cancers. Other severe side effects might include liver, kidney, or lung damage.
Treatment Of Ulcerative Colitis
Medical and surgical therapy- pouch procedure
The primary goal of treatment is to improve patients symptoms and, once this is successful, to prevent recurrence. The usual first step is the use of drugs. The choice of therapy depends on the severity of patients symptoms. In cases with mild to moderately severe inflammation, 5-aminosalicylic acid is often prescribed. In patients in whom the joints are also affected, sulfasalazine can be tried. This drug, discovered in 1942 by the Swedish physician Nanna Svartz, was the standard treatment for ulcerative colitis prior to the introduction of 5-aminosalicylic acid. 5-aminosalicylic acid, also known as mesalazine or mesalamine, is a specially manufactured agent designed to be released in the lower third of the small bowel and in the upper two-thirds of the colon. In those cases in which ulcerative colitis affects only the rectum or left side of the colon , the disease may respond to suppositories, enemas or rectal foams that contain either 5-aminosalicylic acid or cortisone preparations. In severe cases, the administration of cortisone preparations either as pills or injections is usually effective.
Don’t Miss: Foods To Eat To Help Ulcers
What Is The Latest Treatment For Ulcerative Colitis
Some doctors and researchers believe that ulcerative colitis flare-ups are due to an imbalance of good vs bad bacteria in the gut. Lactobacillus and E. coli probiotics have been shown in some studies to be effective at preventing flare-ups. For this reason, the newest therapy in clinical trials is fecal microbiota transplantation . A solution of fecal matter taken from a healthy family member or centralized stool bank is injected into the patients colon during a colonoscopy. The goal is to recolonize the gut with healthy bacteria. Early case reports show real promise in achieving remission, but more work needs to be done to see how long the positive effects last.
Ulcerative Colitis Treatment Options
Treatment of ulcerative colitis focuses on one of two goals: inducing remission during an active flare-up or maintaining remission. These goals are largely accomplished through medications that will be tailored to the severity and extent of the illness. Severe disease or complications may require surgical removal of part or all of the colon.
Don’t Miss: Probiotics Good For Ulcerative Colitis
Ulcerative Colitis And Alcohol: Your Guide
When you have an inflammatory bowel disease like ulcerative colitis , dietary and lifestyle changes may become critical for managing your symptoms and preventing flare-ups. Although drinking alcohol isn’t a risk factor for developing UC, alcohol use can sometimes damage the gastrointestinal tract and make existing symptoms worse. As one MyCrohnsAndColitisTeam member stated, I had three Angry Orchard ciders last night. It caused me to have loose stool and rectal pain after.
The decision to consume alcoholic drinks is up to you. Knowing the risks involved may help you make the best decision for your body and your UC.
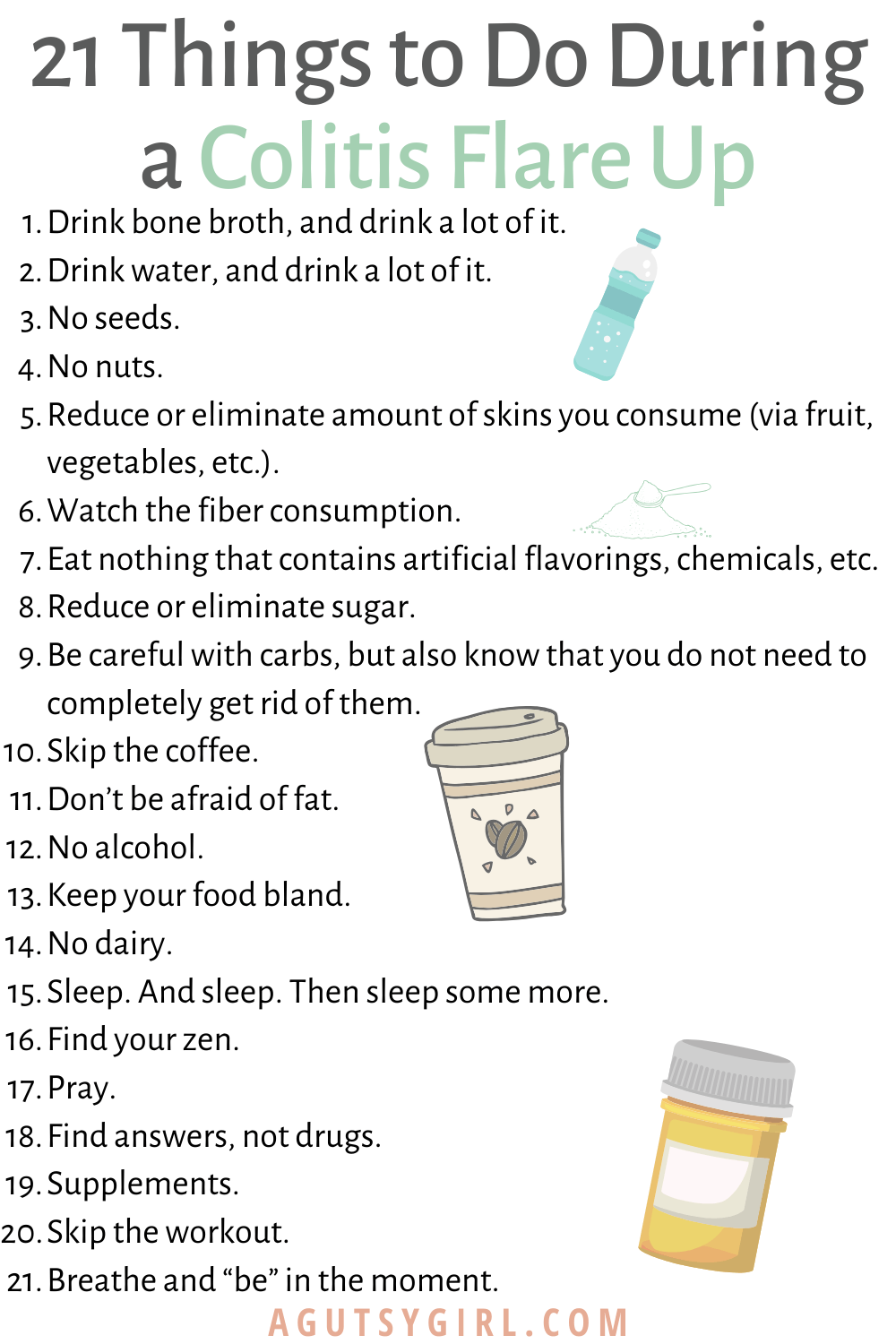
What Are Some Practical Steps To Take When A Flare
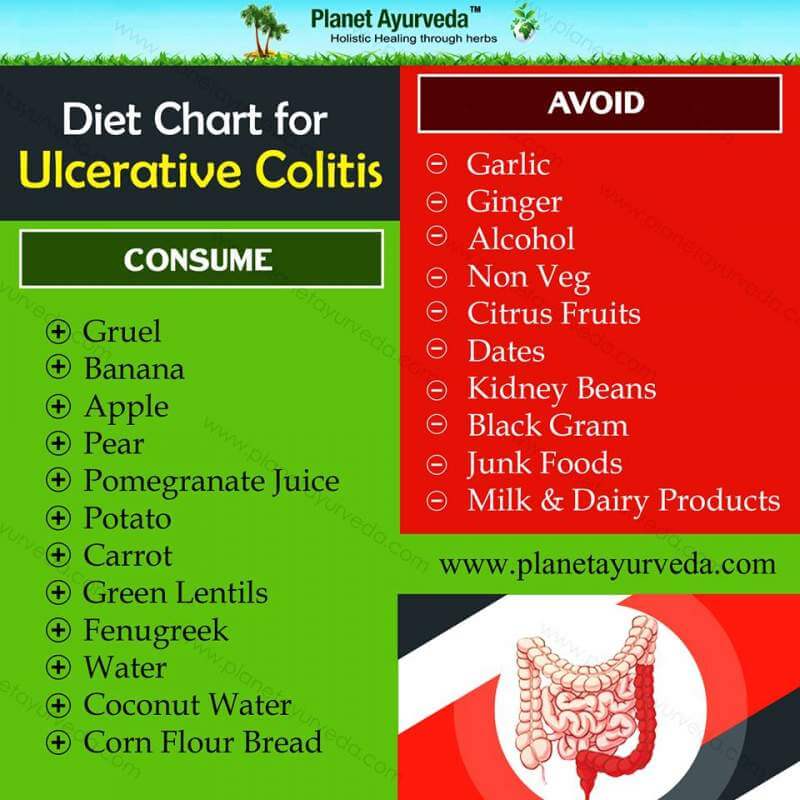
The first thing to do if a flare up occurs is to make sure you are eating a healthy diet which is low in fibre and contains plenty of water. Avoiding dairy products and cutting down carbohydrates may also help. The vast majority of people will requite adjustments to their medication, so you should seek medical advice from your GP or specialist.
Read Also: Does Turmeric Help Ulcerative Colitis
What Is The Best Medication For Ulcerative Colitis
The severity and extent of ulcerative colitis will determine the most appropriate medications for the condition. For this reason, there is no best medication for ulcerative colitis. Instead, a patients medical situation and tolerance for side effects will determine the best medications for treating ulcerative colitis.
| Best medications for ulcerative colitis | |
|---|---|
| Drug Name | |
| Administered weeks 0 and 4 then every eight weeks subcutaneously. | Upper respiratory tract infections, headache, diarrhea, sore throat |
Many of the standard dosages above are from the U.S. Food and Drug Administration or the National Institutes of Health . Dosage is determined by your doctor based on your medical condition, response to treatment, age, and weight. Other possible side effects exist. This is not a complete list.
Easing Symptoms During A Flare
The below suggestions can also help ease symptoms or help keep your body healthy during a flare-up.
Drink water: In UC, the large intestine can have a hard time absorbing water and salt, which can contribute to diarrhea and dehydration. Drinking plenty of water or an electrolyte replacement drink can help avoid dehydration if you’re experiencing a flare.
Eat plain, easy-to-digest foods: During a UC flare, it’s common to lose your appetite. To keep your energy levels up and avoid malnutrition and weight loss, it’s important to continue to fuel your body with food. Unfortunately, fruits and vegetables, particularly when raw, are bothersome for many people with UC. Avoid fatty and greasy foods as well. Your doctor may also suggest meal replacement drinks if you’re losing weight from UC flare-ups.
Get some exercise: If you’re experiencing symptoms like stomach pain and diarrhea, exercise may sound like the last thing you want to do. But in addition to the well-known mood and health-boosting benefits of exercise, a workout can also have specific benefits for UC symptoms. Uncontrolled inflammation in the intestinal tract leads to UC symptoms. Exercise has an anti-inflammatory effect that can help these symptoms.
Also Check: What Can I Take For Ulcerative Colitis Pain
Goals Of Treatment Of Ulcerative Colitis
UC is a chronic condition, which means it is never fully cured. It’s normal for people with UC to have periods of active symptoms, called flare-ups, and periods during which symptoms are improved, called remissions. These are the main goals of treatment:
-
Controlling flare-ups to get you in remission, and to keep you in remission once you get there
-
Improving quality of life and improving your symptoms so they dont interfere with your daily activities
-
Avoiding serious complications, such as serious bleeding or colon cancer
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
You May Like: Is Alcohol Bad For Ulcerative Colitis
How To Lower Your Risk For Colitis Flare
Ulcerative colitis is an inflammatory bowel disease that affects your large intestine. More than 750,000 people in North America alone live with this condition. If youre one of them, you know that ulcerative colitis is marked by inflammation and painful ulcers.
Gastroenterologist Eric Ibegbu, MD, and our team at Atlantic Medical Group can diagnose and treat ulcerative colitis with medications and/or surgery.
If youre suffering from painful flare-ups and GI discomfort, we suggest scheduling a visit with us. A colonoscopy can confirm the cause of your symptoms so you can get the right treatment.
In the meantime, you can lower your risk for colitis flare-ups with these tips.
Layers Of The Bowel Wall
The walls of your bowel have layers. The inner layers take in nutrients from food. The outer layers help move food through the gut and waste out of the body.
In Colitis, theres inflammation and swelling of the inner layer of the bowel wall. This can cause bleeding. More mucus may be produced by the inner layer of the bowel wall. Ulcers develop on the inner layer as the condition gets worse, but they can also go as the condition gets better.
The inflammation in Colitis affects how your body digests food, absorbs nutrients and gets rid of waste.
Everyone experiences Colitis differently. When youre having symptoms, its known as active disease, a flare-up or relapse. Symptoms may be mild or severe and are likely to change over time.
Your symptoms may vary depending on where Colitis is active in your bowel and how severe it is. Find out more in the section Types of Colitis.
The most common symptoms are:
Andy
Read Also: What Are Some Symptoms Of An Ulcer
Work With Your Doctor
Youâll need to see your doctor regularly. It may be every 6 months while youâre in remission. Youâll have routine procedures like colonoscopies and bloodwork to check on your UC.
If youâre having a flare-up, make sure to check in with your doctor. UC isnât the only thing that causes digestive symptoms. They may need tests to rule out something else, like an infection. Or you may need your prescriptions adjusted.
Certain symptoms mean you need help right away. Call your doctor if you:
- Canât keep liquids down
- Have severe diarrhea
- Have a fever
Ulcerative Colitis Flare Symptoms
Flare-ups indicate that the disease is in an active state, which means the rectum and colon are becoming more inflamed or sores are worsening or spreading. Symptoms of flare-ups include:
- Experiencing frequent or urgent bowel movements
- Diarrhea, which may include blood or pus
- Stool thats bloody
- Vomiting
- Weight loss
The pattern of UC flare-ups is unpredictable. The disease is considered active when symptoms are present, and in remission when no symptoms are present. Some people may spend years in remission, while others may have more frequent flare-ups.
Don’t Miss: Ulcerative Colitis Treatment In India