Who Is At Risk For A Decubitus Ulcer
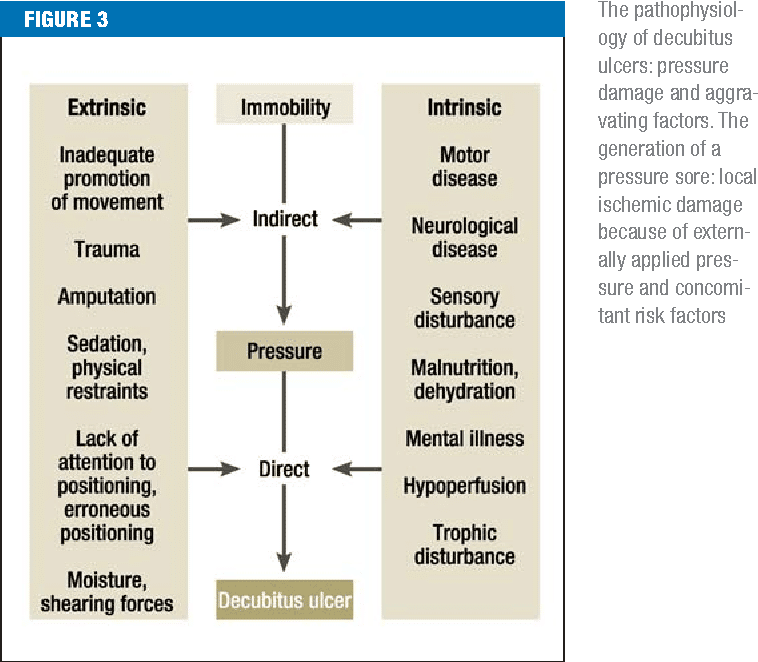
Individuals with limited mobility and who remain for long periods of time sitting or lying in the same position are vulnerable to developing pressure ulcers. Older individuals with more fragile skin are also at risk. Other risk factors include:
- Poor diet with insufficient nutrients for skin health.
- Not drinking enough water to hydrate skin.
- Medical conditions such as diabetes which causes poor blood circulation to skin tissue.
Take Care Of Your Skin
- Do skin checks in the morning and the last thing at night. Look for redness, dark areas, cracks, bruises, and blisters. Note any white spots or areas. The skin may turn white before it reddens. Watch for red, tender, or swollen areas on the skin. Pay special attention to any areas that stay red after the pressure has been relieved. The goal is to find and correct problems before skin breakdown occurs.
- Feel for lumps, soft areas, or unusual warmth . Do not massage a reddened area.
- Clean when incontinent as soon as possible. Use a soft cloth or sponge to reduce injury to skin.
- Minimize moisture from urine or stool, perspiration, or wound drainage. Use pads or briefs that absorb urine and have a quick drying surface that keeps moisture away from the skin.
- When bathing or showering, use warm water and a mild soap.
- To prevent dry skin, use creams, ointments, or oils on the skin. Dont use alcohol or other drying agents on the skin.
- Avoid cold or dry air.
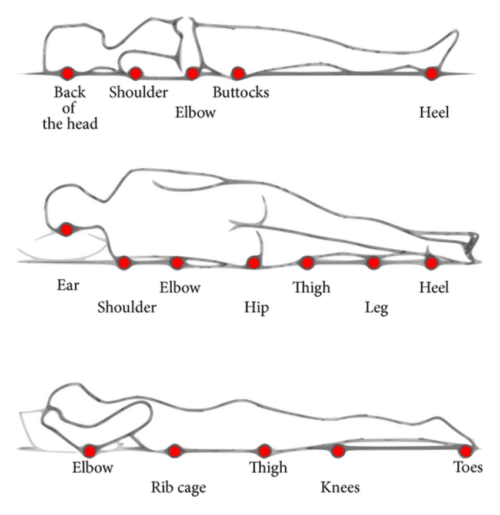
- Limit pressure over bony parts by changing positions.
- If in bed, change position at least every 2 hours.
- If in a wheelchair, change position every 15 to 60 minutes.
- Be careful not to scrape sensitive areas when changing positions. Bed sheets or lifters can be used to help lift the body. A thin layer of cornstarch on the skin may help reduce damage from friction.
- Avoid lying directly on the hip bone when lying on your side. Also, choose positions that spread weight and pressure more evenly.
Clinical Case Presentation: Pressure Ulcer Management
Thorough wound assessments and sensible product selections are essential for preventing and treating wound infections, managing exudate and finally restoring skin integrity.
This is the clinical case presentation of Fernanda Cortes from Chile who explains step by step how she treated the stage 3 pressure ulcer of a 60-year-old family father. Through her commitment and the effective combination of Prontosan®, Askina® and Linovera® the patient eventually recovered.
Please note that the pictures in the video may be disturbing to sensitive persons.
Read Also: Diet When You Have An Ulcer
You May Like: Wound Vac For Pressure Ulcers
Causes And Prevention Of Pressure Sores
Pressure sores are wounds that develop when constant pressure or friction on one area of the body damages the skin. Constant pressure on an area of skin stops blood flowing normally, so the cells die and the skin breaks down.
Other names for pressure sores are bedsores, pressure ulcers and decubitus ulcers.
Keep The Skin Dry And Clean
Incontinence is one of the biggest factors associated with the development of pressure sores. When bowel movement or urine stays in contact with the skin, acids and enzymes in them will begin to cause excoriation and degradation of the skin faster than usual. When combined with limited ability to reposition oneself, a senior may develop a pressure sore in the perineal area faster.
If the area appears to become reddened, the senior may have developed a Stage I pressure sore. When this occurs, it is best to assume the area has been subject to more intense pressures and proceed with an appropriate treatment, such as the use of a barrier cream to help prevent further excoriation due to bodily substances. However, the use of a barrier cream does not negate the need for continued repositioning and movement to help prevent worsening of the area.
Read Also: How To Eat With A Stomach Ulcer
You May Like: Best Feed For Ulcer Prone Horses
Who Is Most Likely To Get A Pressure Ulcer
Anyone living in a care home can develop a pressure ulcer, but some factors make it more likely.
Risk factors include:
- Limited mobility or being unable to change position without help.
- A loss of feeling in part of the body.
- Having had a pressure ulcer before, or having one now.
- Not having eaten well for a period of time.
- Thin, dry or weak skin.
- A significant cognitive impairment.
Hygiene And Wound Dressings
Practice good hygiene. For stage I ulcers, wash the area with water and mild soap, rinse well and pat the area dry gently and carefully. Do not rub forcefully on the area directly over the wound. Usually Stage I decubitus ulcers will not need to be covered.
For Stage II and III ulcers, use saline solution to clean the wound and dry it carefully. Apply either gauze dampened with saline, a hydrocolloid dressing , or a thin foam dressing such as Allevyn. The latter two dressings can be left on until they loosen or wrinkle for up to five days. If gauze is being used, the dressing should be changed twice each day and should stay damp between the times the dressing is changed. Always check to see if the ulcer is healing every time you change the dressing.
The best treatment for decubitus ulcers that are stage IV is to consult a physician for instructions. Many times these types of wounds require surgery and dressings for this kind of ulcer should be applied by a professional. A surgery called debridement is utilized to remove all dead tissue so that the wound will not become infected. Some minor debridement can be done at the bedside but larger areas need to be done in the operating room. The physician will medicate the patient because this is usually a painful procedure.
Read Also: Can A Bleeding Ulcer Cause Blood In Urine
Whos Most At Risk Of Getting Pressure Ulcers
Anyone can get a pressure ulcer, but the following things can make them more likely to form:
- being over 70 older people are more likely to have mobility problems and skin thats more easily damaged through dehydration and other factors
- being confined to bed with illness or after surgery
- inability to move some or all of the body
- medical conditions that affect blood supply, make skin more fragile or cause movement problems such as diabetes, peripheral arterial disease, kidney failure, heart failure, multiple sclerosis and Parkinsons disease
What Are The Symptoms Of Bedsores
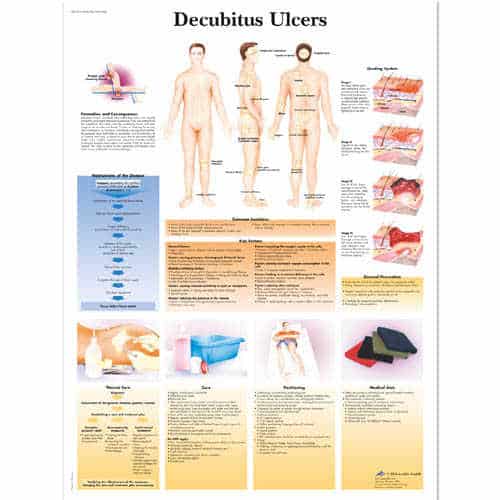
Bedsores are divided into 4 stages, from least severe to most severe. These are:
- Stage 1. The area looks red and feels warm to the touch. With darker skin, the area may have a blue or purple tint. The person may also complain that it burns, hurts, or itches.
- Stage 2. The area looks more damaged and may have an open sore, scrape, or blister. The person complains of significant pain and the skin around the wound may be discolored.
- Stage 3. The area has a crater-like appearance due to damage below the skin’s surface.
- Stage 4. The area is severely damaged and a large wound is present. Muscles, tendons, bones, and joints can be involved. Infection is a significant risk at this stage.
A wound is not assigned a stage when there is full-thickness tissue loss and the base of the ulcer is covered by slough or eschar is found in the wound bed. Slough may be tan, grey, green, brown, or yellow in color. Eschar is usually tan, brown or black.
Read Also: What Is A Vascular Ulcer
Diagnosis Of A Decubitus Ulcer
Wound care physicians and nurses experienced in pressure ulcers are often consulted for decubitus ulcer diagnosis. Medical personnel may take samples of the pressure ulcer tissue and fluid to look for bacteria or cancer. They may also do blood cultures, bone scans or other tests depending on the seriousness of the ulcer. In addition, they will evaluate the condition of the ulcer according to:
- The size of the decubitus ulcer and depth of the crater
- What kind of tissue is affected by the ulcer: skin, bone, or muscle
- The color of the ulcer and skin around it
- The tissue death caused by the ulcer
- The presence of infection, bleeding or foul odor
What Causes Pressure Injuries
- Continuous pressure builds when you sit or lie on a bony area for too long. Pressure slows or stops the blood from flowing to the skin. This may hurt the skin and cause tissue damage. Pressure can start to cause damage to your skin and tissue about 2 hours after staying in the same position.
- Shearing or friction happens when delicate skin is dragged across a surface, such as sheets. This may cause your skin to tear or a blister to form. Sliding up or down in bed or moving from the bed to a chair may tear your skin. Muscle spasms may cause your arms or legs to jerk and rub the sheets, causing tears in your skin.
Also Check: What Should I Eat With Ulcerative Colitis
How Are Bedsores Treated
Specific treatment of a bedsore is discussed with you by your healthcare provider and wound care team and based on the severity of the condition. Treatment may be more difficult once the skin is broken, and may include the following:
- Removing pressure on the affected area
- Protecting the wound with medicated gauze or other special dressings
- Keeping the wound clean
- Removing the damaged, infected, or dead tissue
- Transplanting healthy skin to the wound area
- Negative pressure wound therapy
Healthcare professionals will watch the bedsore closely. They will document size, depth, and response to treatment
Where To Get Help
- Domiciliary care staff
- Ricci JA, Bayer LR, Orgill DP. Evidence-Based Medicine: The Evaluation and Treatment of Pressure Injuries, Plast Reconstr Surg. 2017 Jan 139:275e-286e
- Walia GS, Wong AL, Lo AY, Mackert GA, Carl HM, Pedreira RA, et al. Efficacy of Monitoring Devices in Support of Prevention of Pressure Injuries: Systematic Review and Meta-analysis. Adv Skin Wound Care, 2016 Dec 29:567-574
- Wound, Ostomy and Continence Nurses Society-Wound Guidelines Task Force, WOCN 2016 Guideline for Prevention and Management of Pressure Injuries : An Executive Summary. J Wound Ostomy Continence Nurs. 2017 May/Jun 44:241-246
- Scafide KN, Narayan MC, Arundel L. Bedside Technologies to Enhance the Early Detection of Pressure Injuries: A Systematic Review, J Wound Ostomy Continence Nurs. 2020 Feb 13.
- Munoz N, Posthauer ME, Cereda E, Schols JMGA, Haesler E. The Role of Nutrition for Pressure Injury Prevention and Healing: The 2019 International Clinical Practice Guideline Recommendations. Adv Skin Wound Care, 2020 Mar 33:123-136.
- Qigui X, Qinling Y, Huapeng L. Meta-analysis of effect of foam dressing and hydrocolloid dressing on bedsore management. Chinese Nurs Res. 2017 31:3397-3400.
- Westby MJ, Dumville JC, Soares MO, Stubbs N, Norman G. Dressings and topical agents for treating pressure ulcers. Cochrane Database Syst Rev. 2017 6.
Don’t Miss: What Are The Symptoms Of Ulcers In The Esophagus
Treating And Preventing Pressure Ulcers
Treatment for pressure ulcers includes the use of dressings, creams and gels designed to speed up the healing process and relieve pressure. Surgery is sometimes recommended for the most serious cases.
For some people, pressure ulcers are an inconvenience that require minor nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning or gangrene.
Read more about the complications of pressure ulcers.
Pressure ulcers can be unpleasant, upsetting and challenging to treat. Therefore, a range of techniques is used to prevent them developing in the first place. These include:
- regularly changing a personâs position
- using equipment to protect vulnerable parts of the body such as specially designed mattresses and cushions
Read about treating pressure ulcers and preventing pressure ulcers for more information.
Unfortunately, even with the highest standards of care, itâs not always possible to prevent pressure ulcers in particularly vulnerable people.
What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
Dont Miss: Foods To Eat If You Have A Stomach Ulcer
Also Check: Best Protein Shakes For Ulcerative Colitis
Case Definition And Data Sources
In the GBD 2019 study, decubitus ulcers are defined as an injury to the skin and underlying tissue resulting from an obstruction of blood flow due to pressure on the skin. It is also known as a pressure ulcer/sore. The database in the GBD 2010 study of decubitus ulcers included surveys and systematic reviews in PubMed and Google Scholar with stipulated inclusion criteria. For the GBD 2013 study, the search strategy of the GBD 2010 study was replicated to capture epidemiological studies published between 2012 and 2013. Subsequently, other studies that met the inclusion criteria, hospital inpatient, USA claims data from 2010 to 2016, Taiwan claims data for 2016, and Poland claims data for 20152017, were added during the GBD 2019 study update. The exclusion criteria include abnormal or unreasonable data compared with the regional, super-regional, and global ratios. Details on data adjustment were consistent with previous studies. Data obtained from the GBD 2019 study for decubitus ulcers were employed to calculate the studys estimates. The detail data sources used in estimating the burden of decubitus ulcers in the different countries can be found with the GBD 2019 Data Input Sources Tool using the following link: .
Who Is At Risk For Developing Pressure Injuries
- People with a limited amount of mobility or a total inability to move. Those in wheelchairs or bedridden are at particular risk and need to be moved or turned regularly.
- Those with prosthetic limbs. If the device does not fit properly, the skin can be irritated and a pressure injury can develop.
- People with a loss of sensation. They are at risk because they may not feel the pressure being applied to the skin. As a result, they may not move, which could worsen the damage.
- Those with malnutrition. Wound healing is slowed when nutritional needs are not met.
- The elderly. As people age, the skin naturally becomes thinner and more easily damaged.
Recommended Reading: Booties To Prevent Pressure Ulcers
Nursing Care Plan For Pressure Ulcer 1
Nursing Diagnosis: Impaired Skin Integrity related to skin breakdown secondary to pressure ulcer, as evidenced by pressure sore on the sacrum, discharge from the sores for a couple of days, pain and soreness
Desired Outcome: The patient will have optimal skin integrity by following treatment regimen for decubitus ulcers.
What Are The Long
If the wound becomes infected, the infection can spread to other parts of the body. Several conditions that may occur if an infection spreads include:
- Cellulitis: An infection of the skin.
- Osteomyelitis: An infection of the bone.
- Bacteremia: An infection of the blood.
- Meningitis: An infection of the brain and spinal cord.
- Endocarditis: An infection of the heart.
Also Check: How Do You Cure Ulcerative Colitis
Symptoms Of Pressure Sores
Pressure sores go through 4 stages.
- Stage 1. During this stage, the area of the sore looks red. It may feel warm to the touch. It may burn, hurt, or itch. The pressure sore may look blue or purple in people who have dark skin.
- Stage 2. During this stage, the area is more damaged. The sore may be open. It may look like a cut or blister. The skin around the sore may be discolored. The sore is painful.
- Stage 3. During this stage, the sore will have a crater-like look. This is due to increased damage below the surface. This makes the wound deeper.
- Stage 4. This is the most serious stage. Skin and tissue are severely damaged. The sore becomes a large wound. Infection is possible. Youre likely able to see muscle, bones, tendons, and joints.
Infected pressure sores take a long time to heal. Also, the infection can spread to the rest of your body. Signs of infection at the site include:
- Thick, yellow, or green pus
- A bad smell coming from the sore
- Redness or skin that is warm to the touch
- Swelling around the sore
Signs that the infection has spread include:
Treatment For Pressure Sores
There are a variety of treatments available to manage pressure sores and promote healing, depending on the severity of the pressure sore. These include:
- regular position changes
- special mattresses and beds that reduce pressure
- being aware of the importance of maintaining healthy diet and nutrition
- dressings to keep the sore moist and the surrounding skin dry. There is no advantage of one type of dressing over another.
- saline gauze dressing may be used if ointments or other dressings are unavailable.
- light packing of any empty skin spaces with dressings to help prevent infection
- regular cleaning with appropriate solutions, depending on the stage of the sore
- there is no advantage of one particular type of antiseptic or antibiotic treatment over another
- specific drugs and chemicals applied to the area, if an infection persists
- surgery to remove the damaged tissue that involves thorough debridement of the wound, the removal of underlying or exposed bone, and filling the empty space
- operations to close the wound, using skin grafts if necessary
- continuing supportive lifestyle habits such as eating a healthy and nutritious diet, as suggested by the nutritional staff.
Recommended Reading: Crohn’s Vs Ulcerative Colitis Symptoms