First Cycle Of Change: Action
Training sessions to care staff
The data collected from the action teams of the four homes indicated that many care staff members, especially PCWs, were not aware of the importance of their daily care e.g., repositioning of the residents, use of positioning devices in pressure ulcer prevention. Besides, the majority of HWs did not use tools to assess the PU risk of the residents. Each nursing homes action team designed a training session of 2.5 h for HWs and PCWs, and another training session of 1 h for HWs and/or nurses. The above mentioned knowledge deficit of the PCWs and HWs was emphasized in the training sessions.
Implementation of the protocol
The care staff in each NH carried out the protocol for six weeks according to the flow of the protocol. The HWs/or nurses assessed the PU risk of each resident using the modified Braden scale and then planned the preventive interventions based on the identified risk. The PCWs delivered the care to the residents accordingly and inspected the residents skin when they performed perineal care and re-position the residents. If they noticed redness and/or lesions in the skin, the PCWs notified the HWs or nurses to assess whether they were PUs. During and after the implementation of the protocol in each cycle, some data were collected through various methods including field observations of prevention practices of care staff, focus group interviews with care staff, and assessments of the incidence of PU among the residents.
Description Of The Intervention
This review includes RCTs of any dressings or topical agents applied directly onto or into wounds and left in situ, as opposed to products used to irrigate, wash or cleanse wounds and those that are only in contact with wounds for a short period.
Dressings
The classification of dressings usually depends on the key material used in their construction, and whether additional substances are added to the dressing. Several attributes of an ideal wound dressing have been described , including the ability of the dressing to:
-
absorb and contain exudate without leakage or strikethrough, in order to maintain a wound that is moist but not macerated
-
achieve freedom from particulate contaminants or toxic chemicals left in the wound
-
provide thermal insulation, in order to maintain the optimum temperature for healing
-
allow permeability to water, but not bacteria
-
optimise the pH of the wound
-
minimise wound infection and avoid excessive slough
-
avoid wound trauma on dressing removal
-
accommodate the need for frequent dressing changes
-
provide pain relief and
-
be comfortable.
There are numerous and diverse dressings available for treating pressure ulcers and their properties are described below.
Absorbent dressings are applied directly to the wound and may be used as secondary absorbent layers in the management of heavily exuding wounds. Examples include Primapore , Mepore and absorbent cotton gauze .
Topical agents
Staging Of Pressure Ulcers
The ulcer is staged as per its depth. Staging does not depend on the total area of the ulcer. A stage I or II pressure ulcer may have a large surface area, but a stage III or IV is usually of relatively smaller diameter but of greater depth.
Stages are progressive and need regular assessment and early management.
- Stage 1 There is a change in color of the skin that may turn redder or darker and may not blanch on application of pressure with a gloved finger. The skin feels warmer than that of the surrounding skin. In some cases the skin may appear normal and only an examination determines abnormality.
- Stage 2 In this stage there is break in the outer epidermal layer of skin and some invasion within the next layer the dermis. These show up as shallow craters, ulcers, blisters or abrasions. The blisters may be filled with a clear or cloudy fluid.
- Stage 3 These extend into the subcutaneous tissue and gape as open wounds. Underlying bone, muscle, and tissues are visible but these structures are not affected. There may be formation of tunnels of damage in this stage.
- Stage 4 These ulcers affect the underlying bones and muscles as well as joints, tendons and nerves.
Also Check: Best Thing To Take For Stomach Ulcer Pain
Action Research Approach To Improving Care
An action research approach has the potential to facilitate culture shift and practice change . The central tenant of this model is the importance to establish an equal partnership between action researchers and participants to understand, describe, interpret and explain the social context within which practice change and quality improvement is expected to occur. The action research process allows participants to identify the problems or issues, collect pertinent information, make decisions, plan for implementation, and involve in evaluation on an ongoing, cyclical basis. Through the research process, participants develop a sense of ownership of the problem and they are empowered to make the changes that are most relevant to practice. This research paradigm promotes a bottom up approach to change without imposition of values and practices .
In a systematic review of action research studies, emerging evidence supports this approach to promote acceptance of new care practices, continuation of new initiatives, and adoption of new projects in health care . Other previous studies have also found that action research is a strategy to introduce evidence and change in practice , develop new practice , and improve the care practice in healthcare settings. A recent review on implementing evidence-based nursing practice using action research concluded that the action research approach is promising, although there may have been publication bias .
Change In Home Management
The PCWs gradually experienced an improvement in supervision. Through effective supervision, the PCWs were more cooperative at work and more willing to accept advice and instructions from the HWs and/or nurses. All four homes had a formal handing-over time to allow all care staff on duty to report and learn about the health conditions of the residents and the tasks that needed to be performed for the residents in each duty shift. Communication on the care of the residents was also enhanced, especially among the care staff in the homes without nurses. Previous studies identified communication and coordination as important predictors of staff cohesion , which was negatively associated with the development of PUs in a study involving nursing homes .
Read Also: What Foods Should I Eat With Ulcerative Colitis
Treatment For Pressure Sores
There are a variety of treatments available to manage pressure sores and promote healing, depending on the severity of the pressure sore. These include:
- regular position changes
- special mattresses and beds that reduce pressure
- being aware of the importance of maintaining healthy diet and nutrition
- dressings to keep the sore moist and the surrounding skin dry. There is no advantage of one type of dressing over another.
- saline gauze dressing may be used if ointments or other dressings are unavailable.
- light packing of any empty skin spaces with dressings to help prevent infection
- regular cleaning with appropriate solutions, depending on the stage of the sore
- there is no advantage of one particular type of antiseptic or antibiotic treatment over another
- specific drugs and chemicals applied to the area, if an infection persists
- surgery to remove the damaged tissue that involves thorough debridement of the wound, the removal of underlying or exposed bone, and filling the empty space
- operations to close the wound, using skin grafts if necessary
- continuing supportive lifestyle habits such as eating a healthy and nutritious diet, as suggested by the nutritional staff.
What Is A Stage 4 Bedsore
Stage 4 bedsores are the most severe form of , also called pressure sores, pressure ulcers, or decubitus ulcers. A stage 4 bedsore is characterized by a deep wound that reaches the muscles, ligaments, or even bone. They often cause residents to suffer extreme pain, infection, invasive surgeries, or even death.
A stage 4 bedsore may be an unfortunate sign of . Residents of nursing homes may develop these sores if the staff fails to treat earlier-stage sores.
Thankfully, financial compensation may be available if your loved one develops a stage 4 bedsore while living in a nursing home. Get a free case review to see if you can pursue compensation to help pay for medical treatment.
Victims of stage 4 bedsores can take legal action.
to learn if you can access financial aid and hold abusive nursing homes accountable.
Recommended Reading: Can Ulcerative Proctitis Be Cured
Keep The Skin Dry And Clean
Incontinence is one of the biggest factors associated with the development of pressure sores. When bowel movement or urine stays in contact with the skin, acids and enzymes in them will begin to cause excoriation and degradation of the skin faster than usual. When combined with limited ability to reposition oneself, a senior may develop a pressure sore in the perineal area faster.
If the area appears to become reddened, the senior may have developed a Stage I pressure sore. When this occurs, it is best to assume the area has been subject to more intense pressures and proceed with an appropriate treatment, such as the use of a barrier cream to help prevent further excoriation due to bodily substances. However, the use of a barrier cream does not negate the need for continued repositioning and movement to help prevent worsening of the area.
What Are The Symptoms Of Bedsores In Nursing Homes
Some common warning signs of bedsores in nursing homes include:
- Patches of skin that feel cool or warm to the touch
- Pus drainage from wounds
- Strange changes in skin color or texture
- Swelling
- Tender areas of the skin
The most common way to measure the severity of nursing home bedsores is by the depth of soft tissue damage.
Read Also: How Do They Check For Ulcers
Summary Of Main Results
We have successfully conducted a network metaanalysis of dressings and topical agents for healing pressure ulcers. Alongside the analysis we have applied a new method of GRADE assessment , which allows us to view the results in the light of our certainty in their findings. Using this approach, we found the majority of the evidence to be of low or very low certainty, and was mainly downgraded for risk of bias and imprecision . This level of uncertainty within the totality of the dataset impacts on all subsequent interpretation of its outputs.
This review includes 51 RCTs involving a total of 2964 participants, comparing 39 different dressings or topical agents for the healing of pressure ulcers. Most of the studies were in older participants, but four included participants with spinal cord injuries and one was in younger people said to be chronically ill or physically disabled. Seventeen studies included participants mainly with Stage 2 pressure ulcers and 15 mainly had Stage 3 pressure ulcers 13 studies investigated treatment of ulcers with a mean duration of less than three months.
We treated each topical agent as a separate intervention, but initially grouped dressings by class as described in the . The network involved 39 studies in 2116 participants, encompassing 21 different interventions in 27 direct contrasts and these informed 210 mixed treatment contrasts.
Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
Anatomy of Normal Skin
What is a Pressure Ulcer?
There are many contributing factors.
Don’t Miss: What Are Infusions For Ulcerative Colitis
How To Prevent Bedsores In Nursing Homes
Taking steps to prevent bedsores in nursing homes is very important. Nursing home residents and their loved ones should ensure the following is happening on a regular basis.
To prevent bedsores, residents can:
- Shift weight frequently
- Ask for help if needed to reposition
- Perform wheelchair pushups, in which they use their arms to lift off the seat
- Select cushions or mattresses that relieve pressure
- Adjust a beds elevation to no more than 30 degrees
- Wash skin with a gentle cleanser and pat it dry
- Protect skin with a moisture cream
- Inspect skin every day to look for warning signs of bedsores
How Pressure Ulcers Develop
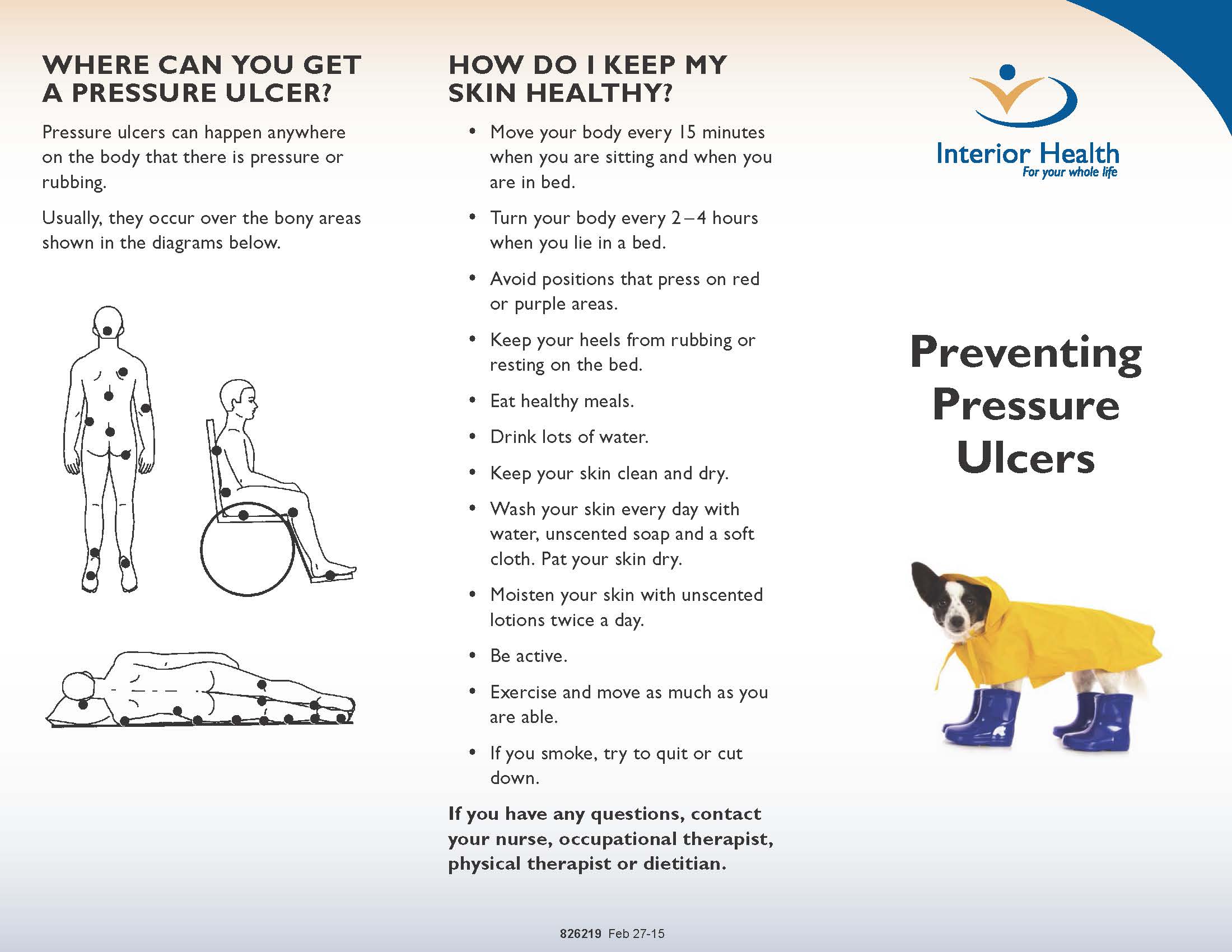
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
Also Check: What Is A Good Diet For Ulcerative Colitis
What Is Pressure Ulcers
Pressure Ulcers also called bedsores ulcers and decubitus ulcers are injuries to skin and underlying tissue resulting from prolonged pressure on the skin. Bedsores most often develop on skin that covers bony areas of the body, such as the heels, ankles, hips and tailbone.
People most at risk of bedsores have medical conditions that limit their ability to change positions or cause them to spend most of their time in a bed or chair.
Bedsores can develop over hours or days. Most sores heal with treatment, but some never heal completely. You can take steps to help prevent bedsores and help them heal.
Criteria For Considering Studies For This Review
Types of studies
We included published and unpublished randomised controlled trials , irrespective of language of report. We did not identify any crossover trials, but we would have included them only if they reported outcome data at the end of the first treatment period and prior to crossover. We excluded studies using quasirandom methods of allocation . We highlighted trials in which three or more interventions were randomised.
Types of participants
We included studies that recruited people with a diagnosis of pressure ulcer, Stage 2 and above , managed in any care setting. We excluded studies that only recruited people with Stage 1 ulcers as these are not open wounds requiring dressings.
We accepted study authors’ definitions of what they classed as Stage 2 or above, unless it was clear that they included wounds with unbroken skin. Where authors used grading scales other than NPUAP, we attempted to map to the NPUAP scale.
Types of interventions
Interventions of direct interest
The interventions in this section were all those that can be directly applied as dressings or topical agents to open pressure ulcers. We presented results for these interventions and included them in summary tables. In the context of a network of competing treatments, there are no ‘comparators’.
Some of the interventions we considered were as follows:
Supplementary intervention set
Terminology
Types of outcome measures
Primary outcomes
-
the proportion of wounds healed
-
time to complete healing .
You May Like: Skin Graft For Foot Ulcer
Description Of The Condition
Pressure ulcers, also known as pressure injuries, bedsores, decubitus ulcers or pressure sores, are localised areas of injury to the skin, the underlying tissue or both. They often occur over bony prominences such as the sacrum and heel , and are caused by external forces such as pressure, or shear, or a combination of both .
Risk factors for pressure ulcer development have been summarised into three main categories: a lack of mobility poor perfusion and low skin status the latter category includes the presence of stage 1 pressure ulcers or incontinence or both, which also increases the risk of ulceration by producing a detrimental environment for the skin .
Prevalence
Pressure ulcers are one of the most common types of complex wound. Prevalence estimates differ according to the type of population assessed, the data collection methods used and period of data collection and whether Stage 1 ulcers were included).
One large European study estimated a hospital pressure ulcer prevalence of 10.5% whilst a US study estimated a prevalence of 9.0% across acutecare, longterm care and rehabilitation settings ). In the UK, national pressure ulcer data are collected across community and acute settings as part of the National Health Service Safety Thermometer initiative . About 4.4% of patients across these settings were estimated to have a pressure ulcer in November 2014 .
Treatments for pressure ulcers
Impact of pressure ulcers on patients and financial costs
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Also Check: Best Vitamins For Ulcerative Colitis