What Laboratory Tests Help Diagnose Ulcerative Colitis
Your doctor would conduct a few blood tests and a stool test to identify if the cause of your symptoms is ulcerative colitis or something else.
Blood tests: A low red blood cell count and low hemoglobin level indicate that you have anemia, which is a symptom of ulcerative colitis.
If you have ulcerative colitis, your blood test may show an increase in white blood cells, a low level of the protein albumin and an elevated C-reactive protein level.
Stool test: Your stool test can let your doctor know if your symptoms are due to infections, such as gastroenteritis.
Surgery For Ulcerative Colitis
Some people get surgery to remove part or all of the colon. Your doctor may suggest this if your medicine isn’t working, your symptoms get worse, or your ulcerative colitis leads to serious complications.
When you have an operation to remove your entire colon, the surgeon most often creates an opening, or stoma, in your belly wall. They attach a bag there and bring the tip of your lower small intestine through the opening. Waste passes through it and collects in a pouch, which gets attached to the stoma. You’d need to wear the pouch all the time.
A newer surgery, called a pelvic pouch or ileal pouch anal anastomosis , doesn’t create a permanent opening. Instead, a surgeon removes your colon and rectum, and your small intestine is used to form an internal pouch or reservoir that serves as a new rectum. This pouch is connected to the anus.
A procedure called a continent ileostomy is done if you want your external pouch converted to an internal one, or if you can’t get the IPAA operation.
In this procedure, there is a stoma but no bag. Your surgeon removes your colon and rectum and creates an internal reservoir from your small intestine. They make an opening in your belly wall and join the reservoir to your skin with a nipple valve. To drain the pouch, you insert a catheter through the valve into the internal reservoir.
Good Bacteria Might Help You Feel Better
UC has been linked to harmful bacteria in the gut. Probiotics are beneficial bacteria that help get rid of bad germs. Adding these supplements to your treatment could help keep you in remission.
No all probiotics are the same, however, and not all of them have evidence to show they can help with UC. People should speak to their doctor before using this option.
Read Also: Signs Of Having An Ulcer
Ways To Naturally Treat Ulcerative Colitis
Is yoga the key to soothing ulcerative colitis? Will an herb provide relief? Natural remedies for ulcerative colitis may not be your primary treatment approach, but they can help you manage symptoms and reduce the frequency of flares.
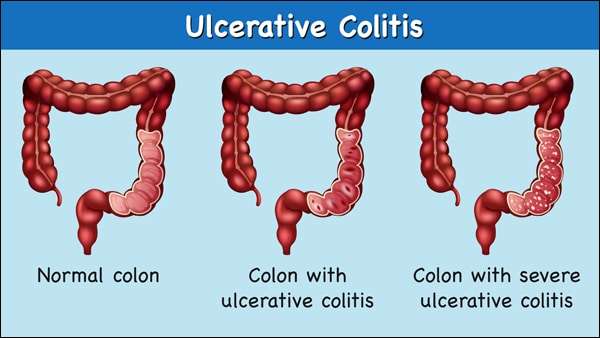
To date, there is no cure for UC, a chronic disease of the large intestine in which inflammation brought on by a faulty immune response creates sores or ulcers in the lining of the colon.
The chronic condition affects nearly 1 million Americans and tends to run in families. Epidemiological research shows that Westernized populations and people with diets high in fat are at higher risk for UC, as well as Caucasians and Ashkenazi Jews. But no one has yet uncovered the main cause of the disease.
Although the official cause of ulcerative colitis has evaded the medical community, its important to understand that it results from an interaction of genetic, environmental, and lifestyle factors, says Benjamin Snider, ND, a naturopathic doctor in private practice in Kitchener, Ontario.
Treatments for ulcerative colitis include medications such as nonsteroidal anti-inflammatory drugs, immune system suppressors, and steroids to control inflammation and other symptoms of the condition. Surgery to remove the colon and rectum is another form of treatment if medication doesnt prove effective.
- Wheatgrass juice
- Curcumin
Read on to learn about some different kinds of natural therapies.
Ulcerative Colitis Surgical Procedures
The standard surgical procedure to treat ulcerative colitis is a proctocolectomy. This surgery removes both your colon and your rectum .
There are two types of proctocolectomy procedures used to treat ulcerative colitis.
-
Proctocolectomy with ileal pouch-anal anastomosis: Removal of the colon and rectum, and creation of an internal pouch that eliminates the need for a permanent external ostomy.
-
Proctocolectomy with end ileostomy: Removal of the colon, recturm, and anus and creation of an external ostomy.
It can feel overwhelming when you are recommended for one of these surgeries. We can help you understand whats involved with each surgery, and be prepared for life after your proctocolectomy.
You May Like: Food To Avoid For Ulcer Patient
You Dont Need To Change Your Diet Dramatically
Theres no evidence that following a strict diet can put you into remission or keep you there. In fact, cutting out certain foods could prevent you from getting the nutrients you need to stay healthy.
You may want to avoid certain foods like dairy products if they seem to aggravate your symptoms. However, talk with your doctor or a dietitian before making any major changes to your diet.
Youre Kidding Me Right Thats A Sick Joke And Youre Now Going To Help This Person Arent You
Well thats not the case unfortunately. That MD is not going to be able to help even though they may think they are and really want to help in the end.
I remember my Naturopath talking to me about people having their entire colon removed. And STILL suffering from IBD after the resectioning and removal process.
I had complete shock as my response. I knew in my gut it was the truth and I knew it could be me with the same outcome. When I went to the Gastroenterologist MD for the last time, he gave me two options:
Because balsalazide disodium, axathioprine, prednisone and mesalamine enamas did not work.
My response : Excuse me? Are you seriously going to give me an ultimatum that I will go on injectable TNF blockers or get my colon cut out of me?
I kindly excused myself from his office. Never to return.
There are people who have more serious conditions such as the one depicted below. I was not at this point yet. Pancolitis such as this is a ruthless disease of inflammation and autoimmune dysfunction.
Read Also: How Effective Is Humira For Ulcerative Colitis
Rice Water To Fight Ulcerative Colitis
One cup of rice water as soon as you wake up and another before bed will help control ulcerative colitis and its symptoms.
Ingredients
- 1 cup of rice
- 3 cups of water
Preparation
Preparing this drink is very simple.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
You May Like: Ulcerative Colitis Left Side Pain
Accelerate Healing With Aloe
Aloe vera gel and liquid chlorophyll, have been shown to be quite effective in speeding the healing of ulcerative colitis. When considering aloe vera gel, look for whole aloe vera gel, not products with aloe juice in them. I suggest taking about 2 ounces, six to eight times a day, on an empty stomach. Stick with this regimen for several weeks, even if your ulcerative colitis symptoms stop before then.
To make the aloe vera even more effective, add a teaspoon of liquid chlorophyll every time you take the aloe vera.
You May Like: What Medicine Is Good For Ulcers
Living With An Ileostomy
You can live a long, active, and productive life with an ileostomy. In many cases, ileostomy patients can participate in the same activities they did before the surgery, including sports, outdoor activities, swimming and other watersports, travel, and work.
Whether your ileostomy is permanent or temporary, it is common for patients to initially feel self-conscious about their ostomy and you may notice a change in how you feel about your body image. Some patients prefer to limit how visible the bag is to others. The ostomy bag typically lays fairly flat under your clothing.
Remember, it is just as important to take care of your mental and emotional health as it is your physical health. Speak with your doctor or a mental health professional if you feel you are experiencing symptoms of depression or anxiety.
-
There are several pouching systems for you to choose from. You will learn how to use your system as well as how to care for the skin surrounding the stoma.
-
Talk to your doctor about any specific dietary restrictions with an ileostomy. It is important for you to drink plenty of fluids to avoid dehydration and loss of electrolytes.
-
Eating foods high in pectin, including applesauce, bananas, and peanut butter, will help thicken your stool output and control diarrhea. Discuss this with your doctor.
The United Ostomy Associations of America has additional resources as you learn to live with your ostomy.
Also Check: How To Ease Mouth Ulcer Pain
Complications Of Ulcerative Colitis
A small number of people with colitis can develop inflammation in other parts of the body, such as the liver, skin, joints and eyes.
Regular monitoring by a gastroenterologist, as well as colonoscopies, may help prevent complications from developing. But medications, including steroids and drugs designed to prevent inflammation and occasionally surgery may be needed.
Osteoporosis can develop as a side effect of long-term corticosteroid use.
Cases of marked inflammation caused by UC can also lead to:
- nutritional deficiencies
- heavy bleeding due to deep ulcers
- perforation of the bowel
- problems with the bile ducts, affecting the liver
- fulminant colitis and toxic megacolon, conditions that cause the bowel to stop working
In the long-term, UC is associated with an increased risk of developing bowel cancer. After 10 years the risk of bowel cancer is 1 in 50, and after 20 years it increases to 1 in 12. This risk can be decreased by maintaining a healthy diet, exercising and avoiding alcohol and smoking.
How To Treat Ulcerative Colitis Naturally At Home 10 Tips
Ulcerative colitis is an inflammatory bowel condition that can cause the inflammation of the rectum and colon. It is known as an autoimmune disease in which the immune system attacks the healthy tissues inside the body, leading it to turn into inflamed.
There is still no research that confirms the exact reason for this disease. It is believed that a combination of environmental and genetic factors contribute to this health issue. Stress can even worsen the symptoms of this disease.
Ulcerative colitis can make the symptoms such as abdominal discomfort or pain, rectal bleeding, diarrhea, and production of pus caused by the ulcers or sores in the large intestine inner lining. The signs of this disease often go after coming, but 5 10 % of patients dealing with this condition face the symptoms of the disease all the time.
Don’t Miss: Psc Liver Disease Ulcerative Colitis
Energy And General Health
If youre following a restricted or relatively bland diet to help cope with a flare of ulcerative colitis symptoms, or youre on a liquid-only diet as your body heals from surgery, you may be getting fewer calories and nutrition. As a result, you might not have as much energy as you typically do.
Its important that you try your best to eat enough each day to meet your bodys nutrition and energy needs. Not only to help manage ulcerative colitis but to maintain your overall health.
Complications from IBD, such as infections, may be more likely if your body is weakened from malnourishment, vitamin deficiencies, and dehydration.
Preventing nutritional deficiencies may help prevent flares: In 2017, research from Beth Israel Deaconess Medical Center indicated that people with ulcerative colitis who are in remission may be more likely to experience a relapse of symptoms if they are deficient in vitamin D.
What Are The Causes Of Ulcerative Colitis
The exact cause of ulcerative colitis is unknown. The following have been suggested:
- Immune system
- Ulcerative colitis is thought to be a type of autoimmune disease, in which the body’s immune system malfunctions and attacks the tissues of the bowel.
Ulcerative colitis may occur at any age, but it is most common in young adults in the 15-30 age group or later on, in the 50-70 age group. Women are affected more than men.
Recommended Reading: What Causes Ulcers On The Feet
Will Ulcerative Colitis Ever Be Cured
Researchers are looking at other treatment options and potential cures for UC.
Two of the newest UC medications developed in the last couple of years include biosimilar medications and Janus kinase inhibitors.
Biosimilar medications contain copies of the antibodies used in a common type of UC medication referred to as biologics. Those antibodies help the body stop production of some proteins that can cause inflammation.
Severe cases of UC can be treated with a JAK inhibitor called tofacitinib . It helps block certain enzymes that can trigger inflammation.
Research is ongoing as to whether other therapeutics, such as stem cell therapy and stool transplant, can treat or cure UC.
It is my firm belief that there will be major improvements to UC management within the next decade.
Sudden Severe Ulcerative Colitis
This complication is the main cause of emergency surgery in patients with ulcerative colitis. With sudden, severe ulcerative colitis, medications and intravenous steroids, are unable to control the symptoms.
-
Uncontrolled bleeding can occur from deep ulcerations in the colon, though that is rare.
-
Severe, sudden ulcerative colitis can lead to toxic megacolon, a potentially life-threatening complication caused by severe inflammation.
-
Toxic megacolon leads to rapid enlargement of the colon. Symptoms include pain, distension or swelling of the abdomen, fever, rapid heart rate, constipation, and dehydration.
-
Toxic megacolon requires immediate treatment and surgery.
Don’t Miss: What Not To Eat With Bleeding Ulcers
Ulcerative Colitis Treatment: Surgery
If you did not respond to a medication regimen or you developed complications of colitis, you may be a candidate for surgery to treat ulcerative colitis.
Colectomy may be used in children with ulcerative colitis who experienced growth retardation. In all patients, elective colectomy can be a cure for ulcerative colitis. Almost always, the procedure is a total colectomy, meaning the entire colon is removed.
Surgical procedures include:
-
Total proctocolectomy with Brooke ileostomy. Removal of your entire colon and rectum. Your doctor will perform an ileostomy, which brings out your small intestine through the abdominal wall. Waste collects in an ileostomy bag. An ileostomy can be temporary or permanent.
-
Restorative proctocolectomy with ileal pouch-anal anastomosis. Removal of the entire colon and most of or the entire rectum. A new rectum is created from the small bowel.This procedure can be performed laparoscopically to ease recovery and reduce scarring.
Do You Have A Depressed Gut
Your gut is actually where the majority of serotonin is produced in your body, and lower than normal levels of serotonin is linked to depression.
Is this the mechanism for why inflammatory bowel diseases such as ulcerative colitis are often triggered by periods of emotional stress?
An article from Scientific American states, the enteric nervous system uses more than 30 neurotransmitters, just like the brain, and in fact 95 percent of the bodys serotonin is found in the bowels. Because antidepressant medications called selective serotonin reuptake inhibitors increase serotonin levels, its little wonder that meds meant to cause chemical changes in the mind often provoke GI issues as a side effect.
Irritable bowel syndrome which afflicts more than two million Americans also arises in part from too much or too little serotonin in our entrails, and could perhaps be regarded as a mental illness of the second brain.
The G.I society, an online publication reports: Scientific evidence strongly suggests that serotonin is one of the most important signalling molecules involved in the peristaltic reflex and that alterations in serotonin signalling may be responsible for IBS symptoms. Ninety-five percent of the serotonin found in the body resides in the gut.
One of these discovered by sheer accident is the anti-depressant, Tianeptine
Don’t Miss: What Foods To Avoid When You Have An Ulcer
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.