Requirements For Vac Therapy
The author has seen many instances where VAC therapy has been applied for diabetes wounds by surgeons without much success. This is due to failure to understand important requirements which must be met before VAC therapy can be applied. These requirements are:
Radical debridement and excision of all infected and devitalised tissues must first be done. VAC dressing cannot be applied over infected or necrotic tissues.
The first application is best done in the operating room after the radical debridement is done by a registrar or medical officer who has been trained in the application of VAC dressings.
Subsequent change of dressings in the ward must be done by a medical officer or a staff nurse who has been trained for VAC therapy.
Training can be provided by an experienced staff nurse on VAC dressing working with the commercial company providing the VAC dressing. The medical officer or staff nurse in the ward in charge of VAC dressing can call upon this experienced personnel in case of any difficulty faced in the application of VAC dressings.
Protocol And Methodological Approach
Our review formed part of a German-language HTA of the benefits and harms of NPWT in patients with wounds healing by secondary intention published by IQWiG in 2019. The full protocol and report are available on the Institutes website . Both the preliminary protocol and the preliminary report underwent public commenting procedures. IQWiGs responsibilities and methodological approach are described in its methods paper . Only completed studies were used, so there was no need for ethical approval and patient consent. We adhered to the PRISMA statement throughout this manuscript.
How Do I Know The Vac Therapy Device Is Working
The therapy status bar at the bottom of the touch screen displays specific therapy information. The spinning icon shows that negative pressure is being applied.Another way to tell if negative pressure is being applied is the foam dressing will be collapsed. You may also see wound fluid moving in the tubing.
How Wound Vac Therapy Works
A VAC therapy system includes a vacuum pump, a special bandage, a canister to collect fluid, and tubing.
A healthcare provider first fits a layer of foam dressing over the wound, which is sealed with a thin layer of film. The film has an opening that rubber tubing can fit through to connect to a vacuum pump.
Once connected, the vacuum pump can remove fluids and infections from the wound while helping to pull the edges of the wound together.
A person undergoing VAC therapy wears the device for close to 24 hours per day while theyre healing. The optimal level of negative pressure seems to be about
Advantages Over Other Possible Treatments
Most treatments for chronic wounds involve a lengthy stay in the hospital. This time can be reduced by using wound vac care because it helps to promote wound closure. If the wound heals quickly, the patient can return to normal activities sooner. Negative pressure wound therapy is also an option with less pain and discomfort for the patient than other possible treatments. And the wound vac success rate is very high.
Wound vac treatment also reduces the risk of an infection versus other forms of treatment. Because wound vac dressing change is only needed every 48 hours, there is less risk of exposure. Other treatments may need to be changed out as much as twice daily.
Graftjacket Regenerative Tissue Matrix
GRAFTJACKET® Xpress flowable soft tissue scaffold supports the body’s repair of damaged or inadequate integumental tissue, such as deep dermal wounds or diabetic ulcers.
GRAFTJACKET® RTM provides a scaffold for the body’s repair or replacement of damaged or inadequate integrumental tissue, such as diabetic foot ulcers, venous leg ulcers, pressure ulcers, or for other homologous uses of human integument.
Featured Products
How Long Does A Wound Vac Stay On
For those who have just had surgery, or have an acute or chronic type of wound, chances are their doctor has prescribed negative-pressure wound therapy as a means to bring healing to the body. Sometimes simply known as a wound vac or vacuum-assisted closure, this therapeutic technique involves using a vacuum pump to apply a type of dressing to the wound.
How To Properly Use The Activac Therapy System Carrying Case
CARRYING CASE
There are 2 different types of ACTIV.A.C. Therapy System carrying cases, which vary by the type of therapy unit you have.
ACTIV.A.C. Therapy System
Place the therapy unit into the case so that the touch screen, power button and charge port are visible through the cut-outs on the carrying case.
ACTIV.A.C. Therapy System with iOn PROGRESS Remote Therapy Monitoring
Place the therapy unit into the case, canister first and run the tubing up the back of the device. Position the unit so that the touch screen, power button and charge port are visible through the cut-outs on the carrying case.
-Keep the therapy unit in the upright position.
-Keep the therapy unit in the carrying case when in use.
-Keep the touch screen facing up if the therapy unit is placed on a level surface such as a table.
Use the adjustable strap to wear the carrying case across your chest.
Do not wrap the carrying case strap, power cord or dressing tubing around neck.
Pressure Sore Vac Treatment
For use in the treatment of pressure sores, there have been many studies that have shown the effectiveness of using VAC equipment to excel and help with the healing of these sores. Part of what makes this machine work well for pressure sores is its ability not only to close the wound but also to protect it from additional bacteria exposure that is often associated with progressed final stage sores . The Agency for Healthcare Research and Quality has several studies that are listed on its website www.ahrq.gov that have shown that this treatment seems to promote faster healing along with protecting the wound from further infection.
Using A Wound Vac To Treat Pressure Sores
Pressure sores, once started, can be difficult to treat and heal, even by the best medical staff. Though prevention is still the best medicine in the case of these painful and deadly sores, there is a treatment that uses a machine called the wound VAC that seems to accelerate the healing while also protecting the wound from infection.
Research Design And Methods
The patient population consisted of diabetic adults 18 years with a stage 2 or 3 calcaneal, dorsal, or plantar foot ulcer 2 cm2 in area after debridement . Adequate blood circulation was assessed by a dorsum transcutaneous oxygen test 30 mmHg, ankle-brachial index values 0.7 and 1.2 with toe pressure 30 mmHg, or Doppler arterial waveforms that were triphasic or biphasic at the ankle of the affected leg. Patients with recognized active Charcot disease or ulcers resulting from electrical, chemical, or radiation burns and those with collagen vascular disease, ulcer malignancy, untreated osteomyelitis, or cellulitis were excluded from the study. Patients with uncontrolled hyperglycemia or inadequate lower extremity perfusion were not enrolled. Exclusion criteria also included ulcer treatment with normothermic or hyperbaric oxygen therapy concomitant medications such as corticosteroids, immunosuppressive medications, or chemotherapy recombinant or autologous growth factor products skin and dermal substitutes within 30 days of study start or use of any enzymatic debridement treatments. Pregnant or nursing mothers were excluded from study participation.
The sample size was based on a type I error probability set at 0.05, with 80% power. Detection of a 20% difference between treatment groups required 206 evaluable patients with a treatment-to-study ratio of 1:1. Sample size was set at 338 to account for subject withdrawal or loss to follow-up.
Wound Coverage And Healing
During the 6 days of NPWT and instillation, visual signs of local inflammation were monitored at each dressing change. It was observed that inflammation decreased over the course of NPWTi treatment. Granulation tissue formation was observed in all thirteen cases.
Six days post-debridement, the wounds were clean with no visual signs of inflammation. The V.A.C. system was removed and wounds were rinsed with the antiseptic agent octenisept®.
The combination of NPWT and octenidine in all 13 patients showed that octenidine is well tolerated and no toxic tissue reactions were reported. These results are consistent with the biocompatibility index evaluated for octenidine, in which the antimicrobial activity and the cellular cytotoxicity of antiseptic agents are assessed. Octenidine demonstrated excellent results on this index, reflected by a BI greater than 1 and therefore superior to a number of antiseptic agents.
Following NPWTi treatment, the wound beds of all patients were clean and clear of infection. A suction drain was positioned under the flap to prevent postoperative fluid accumulation. Patients were cared for on air-fluidised beds to reduce pressure on the wound site.
No signs of inflammation or wound dehiscence around the wound site were observed on day 10 postoperatively. Every day, wound cleansing was conducted using octenisept®. Three weeks after surgery sutures were removed.
How Does Negative Pressure Wound Therapy Work

The best pressure for wound healing appears to be approximately 125 mm Hg, using an alternating pressure cycle of 5 minutes of suction followed by 2 minutes off suction.
Animal studies have demonstrated that this technique:
- Optimises blood flow in the wound bed
- Removes excessive fluid that can slow cell growth and proliferation in the wound bed
- Decreases the numbers of bacteria.
Additionally, intermittent low pressure alters the structure of the cells in the wound bed, triggering a cascade of intracellular signals that increase the rate of cell division and the formation of granulation tissue.
Negative Pressure Wound Therapy With Instillation: Effects On Healing Of Category 4 Pressure Ulcers
Johannes Matiasek1 Gabriel Djedovic2 Ralph Verstappen3 Ulrich M. Rieger2
1Department of Plastic and Reconstructive Surgery, St. Josef Hospital, Vienna 1130, Austria.
2Department of Plastic and Aesthetic Surgery, Reconstructive & Hand Surgery, St. Markus Hospital, Frankfurt 60431, Germany.
3Department of Hand, Plastic and Reconstructive Surgery, St. Gallen Cantonal Hospital, St. Gallen 9000, Switzerland.
Received: First Decision: Revised: Accepted: Science Editor: Copy Editor: Production Editor:
© The Author 2018. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Negative Pressure Wound Therapy For Treating Leg Ulcers
Background
Leg ulcers are wounds that occur between the ankle and the knee as a result of poor blood flow in the legs. These wounds are relatively common often affecting older people. There are several different treatments for these ulcers and the underlying problems that cause them. Negative pressure wound therapy is a treatment currently beng used for wounds including leg ulcers. NPWT involves the application to the wound of a dressing to which a machine is attached. The machine then applies a carefully controlled negative pressure , and sucks any wound and tissue fluid away from the treated area into a canister.
What we found
After extensive searching up to May 2015 to find all relevant medical studies that might provide evidence about whether NPWT is an effective treatment for leg ulcers, we found only one randomized controlled trial that was eligible for this review. The study was small with 60 participants who had hard-to-heal ulcers. The average age of these participants was 73 years, and 77% of them were women. The study was funded by the manufacturer of the NPWT machine. The study explored the use of NPWT in preparing leg ulcers for a skin graft. In the study, the ulcers were treated with NPWT or with normal care until the wounds were considered ready to have a skin graft applied. The study’s results are not relevant for leg ulcers that are not being prepared for skin grafts. Participants remained in hospitals during treatment and until their wounds healed.
How Do I Get Ready For A Vacuum
You likely wont need to do much to get ready for wound VAC. In some cases, you may need to wait a while before having this therapy. For example, your provider may first need to treat an infection in your wound. Dead or damaged tissue may also need to be removed from your wound.
You or a caregiver may need training on how to use the wound VAC device. This is done if you will be able to have your wound vacuum therapy at home. In other cases, you may need to have your wound vacuum therapy in a healthcare facility. If you or a relative will be doing the therapy, youll receive training on how to use the device.
Your healthcare provider will tell you if you need to do anything else to prepare for wound VAC.
Sampling Of Wound Exudates
To simulate realistic wound conditions, wound exudates from patients with leg ulcers, treated with conventional NPWT, were obtained. This occurred when the foam dressings in the wounds were replaced. At this point they were transferred into sterile containers, then soaked with 5 mL of a protease inhibitor solution . To collect wound exudates, the dressings were cut into appropriate pieces using sterile scissors and then squeezed through a sterile press. The wound exudates were collected and captured in 50 mL centrifuge tubes and stored at -20 °C until processing continued or at 6 °C when processed on the same day as the exudates were collected.
How Does Wound Vac Therapy Work
This wound vac therapy includes a vacuum pump, a special bandage for dressing, a canister to collect drainage, and tubing. Firstly, the Wound Care Surgeons will cover your wound with a foam or gauze wound dressing sealed with a thin layer of film. There is an opening in the film that connects to a drainage tube which leads to a portable vacuum pump. When the pump is turned on, it draws fluid and infection from the wound through the foam and also pulls the edges of the wound together. The pump may run all the time or in cycles. It depends on the type of wound vacuum system used.
The undergoing person wears the device for almost 24 hours per day while they are healing. The dressing needs to be changed once a day or more often depending on the type of wound. You or your caregiver will be trained by wound care experts to do this at home or it may be done by themselves.
Treatment Goals For The Application Of Negative Pressure Wound Therapy 101
-
Provide a moist wound environment that is preferable for wound healing
-
Influence expression of genes involved in the wound-healing process, such as growth factors, TGF- expression, and genes that elicit angiogenesis and cellular proliferation
NPWT is often used in the treatment of acute wounds in which healing by primary intention is unlikely or not possible. This includes grossly contaminated wounds and complex soft tissue injuries. NPWT is also used to treat chronic wounds, such as pressure ulcers, trophic, and vascular ulcers. The absence of well-designed studies makes it challenging to draw reliable conclusions regarding the efficacy of NPWT in the treatment of chronic wounds.100 However, single studies have suggested that NPWT can lead to accelerated closure of diabetic foot ulcers when compared with current standards of care using moist wound-healing principles.102,103 NPWT is contraindicated in wounds with exposed viscera, intestinal fistulas, in the presence of invasive soft tissue infection, wound necrosis, or active bleeding. Clinicians should be aware that NPWT can cause pain, pressure necrosis around the wound edges, hemorrhage, and infection when the patient is not properly monitored and treatment is not properly adjusted in light of these adverse responses.69,101
S.A. Moser, S.R. Gilbert, in, 2014
Other Benefits Of Vac
The author has found VAC therapy to be particularly useful for the following:
-
Diabetic wounds which after debridement show exposed bone, tendon, joint capsule or fascia. VAC therapy can promote the production of granulation tissue over bone, tendon, capsule or fascia. However, this takes a much longer time.
-
Large wounds after debridement for necrotising fasciitis.
-
Ray amputation wounds.
Wound Conditioning Using Npwt
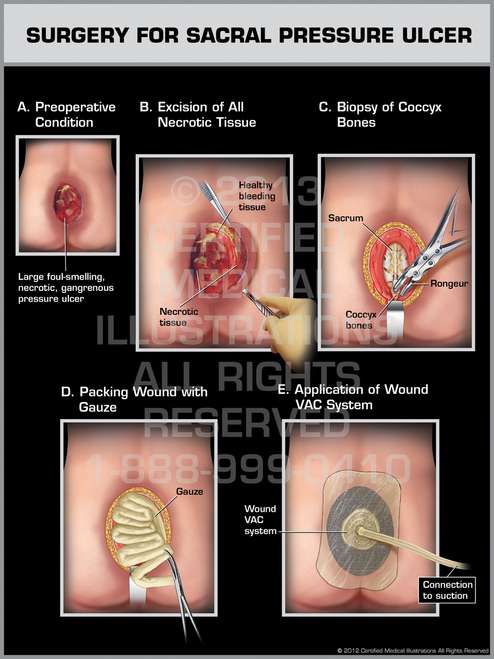
All patients underwent a surgical debridement of necrotic tissue as the first stage of treatment. This was undertaken to remove fluid, exudates and infectious material. NPWT was applied to the wound. A foam dressing was cut into a shape which perfectly fitted the wound cavity. A transparent film was then used to seal the wound and a track pad connected to an adjustable vacuum pump, was applied.
Continuous suction was used to maintain negative pressure at 125 mmHg. Every 12 h, wound rinsing was performed for three minutes using octenilin® wound irrigation solution. To ensure that the ideal quantity of irrigation solution was applied, it was instilled until the foam dressing was completely soaked
The treatment continued for 6 days, after which the wound bed was fully prepared for surgery and free from visible signs of infection.
Prevention Measures For Wound Vac Management
The wound care surgeons will prescribe vac dressing only if it is safe and necessary for the patients to ensure effective wound healing. While the complications can arise, preventive steps need to be taken. Here they are as follows:
-
Make sure that the doctor changing dressing is wearing rubber gloves.
-
Ask healthcare providers whether to stop taking aspirin or other medications that affect bleeding or blood clotting.
-
Avoid keeping the wound vac dressing on without suction for more than 2 hours as it can lead to infection. If the dressing is not repaired or replaced within 2 hours, make sure to remove the entire dressing and consider gauze dressing over the wound.
Final Words
Living with a wound vac can be a little daunting and complex task for the patients, but being aware of important things about the ongoing treatment can make it easier. Vac therapy is an effective treatment option to treat open wounds and increase the healing process. A variety of wounds can be effectively treated with negative pressure wound therapy which is caused by, for example, burns and C-sections , etc. If you are undergoing wound vac therapy, consult your wound care experts and get more information.