Nursing Home Abuse & Neglect Resources
Common Cases:
Client Reviews
Nursing Home Law Center, LLC is not a law firm. It is an organization that concentrates solely on helping provide nursing home patients and their families the legal help they need. NHLC LLC has a network of recognized attorneys located across the country who have experience representing clients in all types of nursing home injury cases. References to NHLC attorneys or our attorneys are references to attorneys within NHLCs network, and not employees, agents, or partners of NHLC. Please consult the disclaimer page for further information concerning NHLC. All information on this site shall be considered attorney advertising and not construed as legal advice. Prior case results should not be relied on when retaining a lawyer.
Which Dressings Or Topical Agents Are The Most Effective For Healing Pressure Ulcers
Dressings and topical agents for treating pressure ulcers
Review question
We reviewed the evidence about the effects of dressings and topical agents on pressure ulcer healing. There are many different dressings and topical agents available, and we wanted to find out which were the most effective.
Background
Pressure ulcers, also known as bedsores, decubitus ulcers and pressure injuries, are wounds involving the skin and sometimes the tissue that lies underneath. Pressure ulcers can be painful, may become infected and affect peopleâs quality of life. People at risk of developing pressure ulcers include those with limited mobility â such as older people and people with short-term or long-term medical conditions â and people with spinal cord injuries. In 2004 the total yearly cost of treating pressure ulcers in the UK was estimated as being GBP 1.4 to 2.1 billion, which was equivalent to 4% of the total National Health Service expenditure.
Study characteristics
In July 2016 we searched for randomised controlled trials looking at dressings and topical agents for treating pressure ulcers and that gave results for complete wound healing. We found 51 studies involving a total of 2947 people. Thirty-nine of these studies, involving 2127 people, gave results we could bring together in a network meta-analysis comparing 21 different treatments. Most participants in the trials were older people three of the 39 trials involved participants with spinal cord injuries.
Key results
What Causes Pressure Sores
Pressure sores are caused by sitting or lying in one position for too long. Its important to know that a pressure sore can start quickly. In fact, a Stage 1 sore can occur if you stay in the same position for as little as 2 hours. This puts pressure on certain areas of your body. It reduces blood supply to the skin and the tissue under the skin. If you dont change position frequently, the blood supply will drop. A sore will develop.
Dont Miss: Food To Avoid For Ulcer Patient
Read Also: What Causes H Pylori Ulcers
Hydrogel Dressings For Treating Pressure Ulcers
Background
Pressure ulcers, also known as bedsores, decubitus ulcers and pressure injuries, are areas of injury to the skin or the underlying tissue, or both. Pressure ulcers can be painful, may become infected, and affect quality of life. Those at risk of pressure ulcers include those with spinal cord injuries and people who are immobile or who have limited mobility such as some elderly people and people with acute or chronic conditions. In 2004 the total annual cost of treating pressure ulcers in the UK was estimated as being GBP 1.4 to 2.1 billion, which was equivalent to 4% of the total NHS expenditure. Pressure ulcers have been shown to increase length of hospital stay and the associated hospital costs. Figures from the USA suggest that pressure ulcer was noted as a diagnosis for half a million hospital stays in 2006 for adults, the total hospital costs of these stays was USD 11 billion.
Dressings are one treatment option for pressure ulcers. There are many types of dressings that can be used these can vary considerably in cost. Hydrogel dressings are one type of available dressing. Hydrogel dressings contain a large amount of water that keeps ulcers moist rather than letting them become dry. Moist wounds are thought to heal more quickly than dry wounds. In this study we investigated whether there is any evidence that pressure ulcers treated with hydrogel dressings heal more quickly than those treated with other types of dressings or skin surface treatments.
Management Of Sacral Ulcers Varies By Ulcer Stage
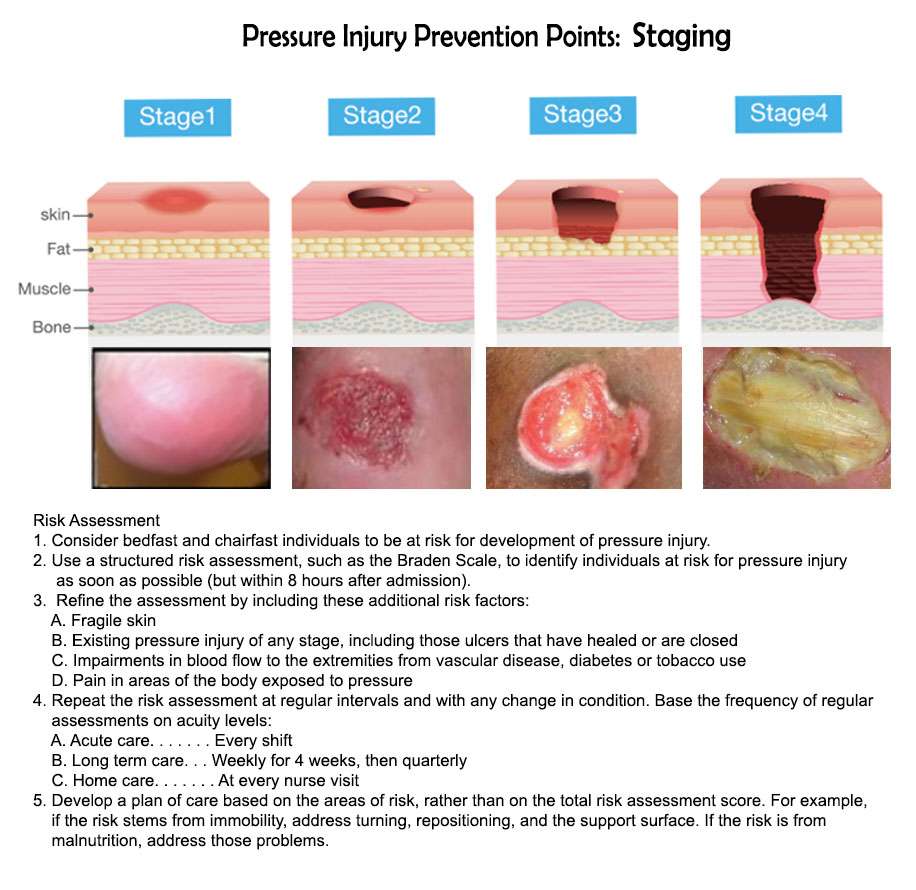
It is important to properly stage pressure ulcers for several reasons, but two of the most important are for prognosis and management planning. Stage 1 and stage 2 pressure ulcers heal by regenerating tissue in the wound. Stage 3 and stage 4 pressure ulcers, on the other hand, heal through scar formation, which means the borders of the wound contract as it heals.
For Stage 1 sacral ulcers, the primary goal of therapy is to ensure adequate tissue perfusion and to protect the wound from further damage.2 This means preventing the sacrum from chronically squeezing the skin and preventing blood flow to the area. The goal of therapy for Stage 2 ulcers is to encourage tissue regeneration and protect the wound surface. For stage 3 or 4 ulcers, management efforts are focused on promoting tissue granulation and epithelialization.
Also Check: Treatment Of Ulcerative Colitis In Child
Stages Of Pressure Ulcers And Treatment
Pressure ulcers can progress in four stages based on the level of tissue damage. These stages help doctors determine the best course of treatment for a speedy recovery.
If caught very early and treated properly, these sores can heal in a matter of days. If left untreated, severe bedsores may require years to heal.
Manage Infected Woundsexpand: More
Askina® Calgitrol®is a range of primary dressings consisting of an ionic silver alginate matrix, which provides a broad antimicrobial effectiveness and helps to prevent contamination from external bacteria. In the presence of wound exudate, the silver alginate matrix helps to maintain a moist wound environment conducive to natural healing conditions.
- Askina® Calgitrol® Paste is a dressing with an ionic silver alginate matrix in a paste form.
- Askina® Calgitrol® Thin is a conformable ionic silver alginate matrix used as a wound bed interface.
- Askina® Calgitrol® Ag integrates an ionic silver alginate matrix on an absorbent polyurethane foam dressing.
Recommended Reading: What To Eat If You Have A Bleeding Ulcer
What Is A Pressure Injury
A pressure injury is an area of injured skin. A pressure injury happens when force is applied on the surface of the skin. This force can be a constant pressure on an area of skin or a dragging force between the skin and another surface. These injuries usually happen over bony parts of the body . A pressure injury can become life-threatening if it advances to a deep wound or becomes infected.
The Available Reconstructive Options Are
Split thickness skin grafting
When the ulcer is superficial and vital tissues such as bone, vessels, nerves or tendons are not exposed, and the ulcer is not copiously discharging, skin grafting is the first option for surgical treatment. The slimy layer over the surface of ulcer is sharply debrided to get a healthy vascular bed for skin grafting.
Local flaps
Variety of local flaps can be used to reconstruct the defect created by excision of pressure ulcers. Local transposition, rotation, limberg flap are the available options .3]. Biceps femoris V-Y advancement for ischial pressure sore and perforator based V-Y advancement is another good options if the anatomy permits .
Sacral pressure sore , debridement and cover by local perforator based V-Y advancement flaps , 1-month post-operative , recurrence on the flap after 11 years due to loss of family support and subsequent improper care. Another patient with the same flap after 16-year of follow-up with a proper weight shifting and care showing stable coverage
Regional flaps
Medial planter flap for heel sore: A long-standing deep trophic ulcer of heel . The islanded medial planter flap was transposed to the defect and the resultant donor site was covered by split thickness skin graft . The 1-week and 3-month post-operative pictures showing stable coverage. Patient allowed full weight bearing from 6th week along with silicone footpad protection
Microvascular free flaps
You May Like: Can Stomach Ulcers Cause Back Pain
Diet And Lifestyle Changes To Avoid Pressure Sores
Changes to avoid pressure sores include:
- Make sure you eat a healthy and nutritious diet. This includes a balanced diet and fluids/water. And if necessary,youre your doctor about vitamin and nutritional supplements .
- Low body weight or being overweight can cause pressure sores, so make sure you maintain heathy body weight
- If youre malnourished or at risk of malnutrition, protein, fluid and energy intake should be increased.
- Be aware of using good hygiene practices.
- Maintain activity levels, where appropriate.
- Make sure you quit smoking.
Keep The Skin Clean And Dry
To help reduce the risk of infection, the skin around the pressure sore should remain clean and dry. Often, nursing staff will use a barrier cream or bandage to help protect the affected skin and keep the patient as comfortable as possible, as well as aiding in the healing process. The type of bandage or barrier cream used may depend on the severity of the pressure ulcer and the patients overall sensitivity.
Also Check: How To Soothe Mouth Ulcers
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
Wound Care: Pressure Ulcer Best Practices
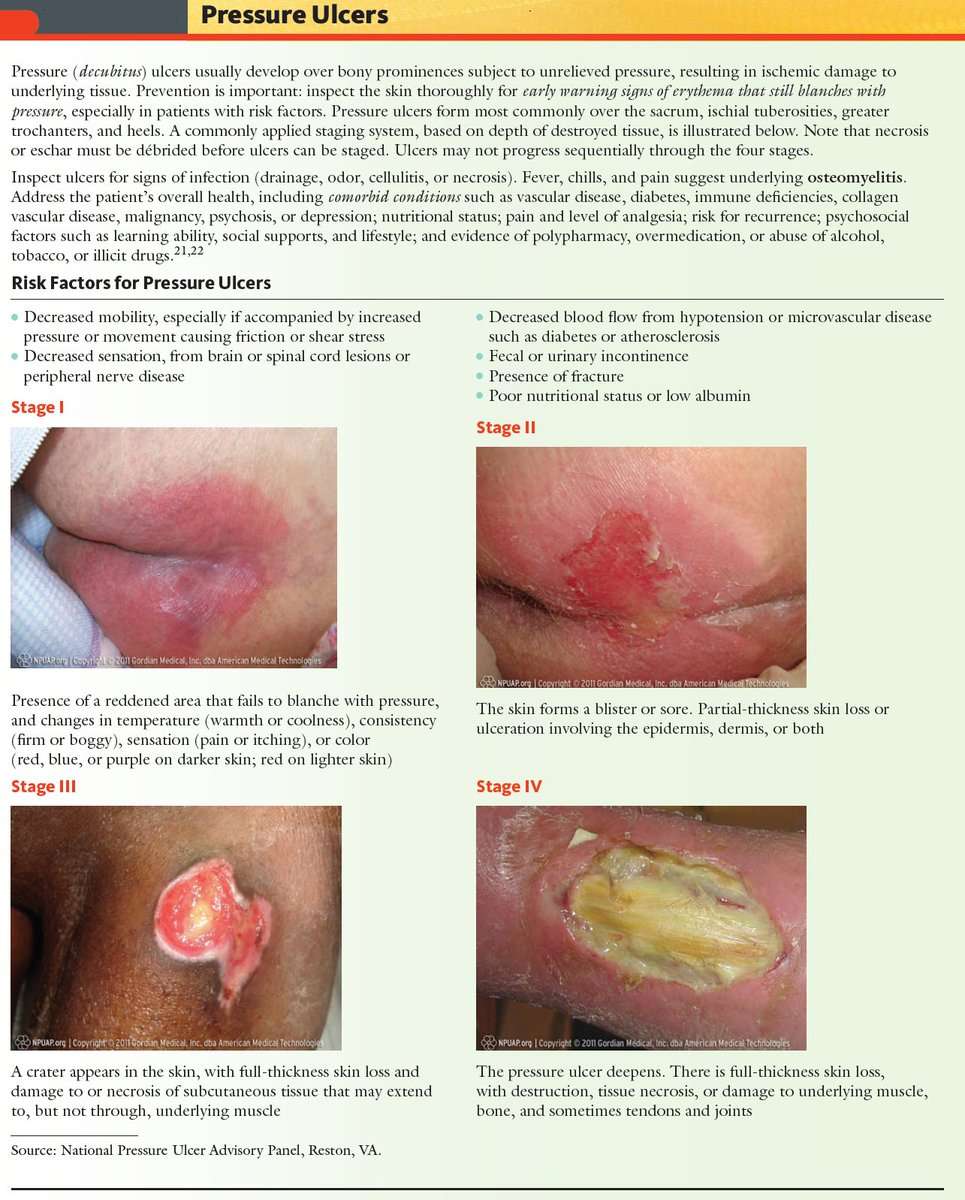
Pressure ulcers, otherwise known as decubitus ulcers, comprise a significant portion of wounds requiring specialized care and presenting additional costs, so prevention is critically important. A pressure ulcer is any lesion caused by unrelieved pressure resulting in damage of underlying tissue. Pressure ulcers usually occur over bony prominences and are graded or staged to classify the degree of tissue damage observed. Stage 1 pressure ulcers are defined as nonblanchable erythema of intact skin the heralding lesion of skin ulceration. Stage 2 is defined as partial thickness skin loss involving epidermis and/or dermis Stage 3 as full thickness skin loss involving damage or necrosis of subcutaneous tissue that may extend down to, but not through, underlying fascia and Stage 4 as full thickness skin loss with extensive destruction, tissue necrosis or damage to muscle, bone or supporting structures.
The Wound, Ostomy and Continence Nurses Society says that pressure ulcer prevention is best accomplished by identifying patients who are at risk for the development of pressure ulcers and initiating early preventive measures. According to the WOCN, This requires an understanding of risk factors, the utilization of research-based risk assessment tools, knowledge of appropriate preventive strategies and access to essential medical equipment such as therapeutic support surfaces.
Related Content:
You May Like: Interventions To Prevent Pressure Ulcers
Assessing Sacral Pressure Ulcers
Pressure-induced skin and soft tissue injuries are often classified using the National Pressure Ulcer Advisory Panel staging system . Under this rubric, the wound should be staged to its deepest extent. This means selecting the highest number stage that accurately describes any part of the wound.
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Non-blanchable is redness that stays despite applying pressure. This means the erythema is not caused by blood within capillaries . Purple or maroon discoloration is not part of stage 1, but rather indicates a deep tissue pressure injury.
What Is A Stage 2 Bedsore
If a stage 1 bedsore is not treated promptly or properly, it may progress into a stage 2 bedsore. At this stage, the bedsore has broken into the top layers of skin, looks like an open blister, and generally causes pain and discoloration.
Nursing home residents may be at risk of bedsores if they have limited mobility or underlying health problems. Untreated stage 2 bedsores can worsen, causing serious health problems or even death. Fortunately, proper medical care can help older adults recover.
You need to know that stage 2 bedsores may be a sign of nursing home abuse or neglect. Staff members are trained to prevent bedsores if they fail to do so, you may be able to hold them accountable through legal action.
Also Check: What Can You Do For A Bleeding Ulcer
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
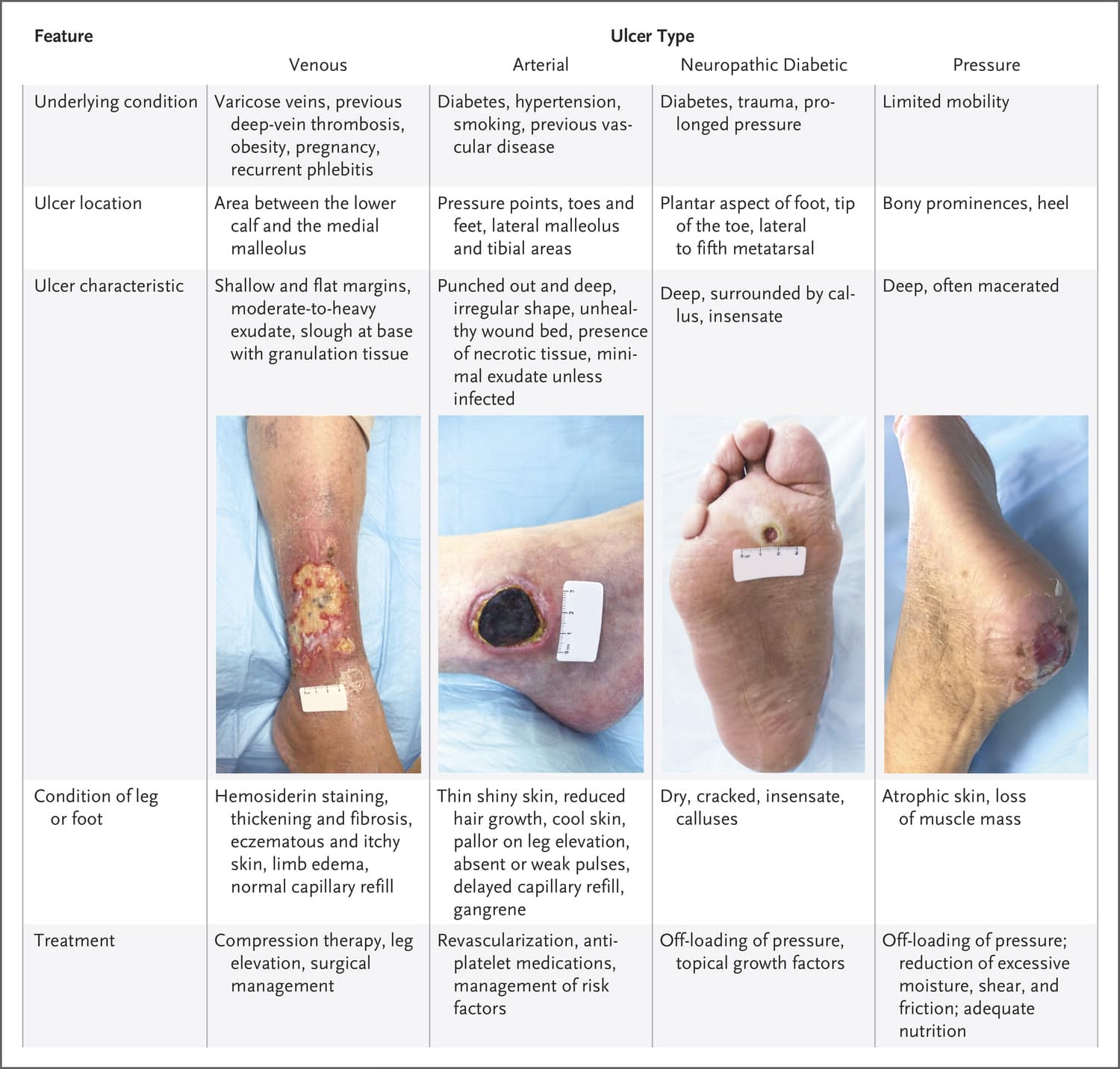
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
What Are The Stages Of Pressure Sores
You may know pressure sores by their more common name: bed sores. They happen when you lie or sit in one position too long and the weight of your body against the surface of the bed or chair cuts off blood supply. You might get them if youre on bed rest or in a wheelchair.
Your doctor may talk about the stage of your pressure sores. The stages are based on how deep the sores are, which can affect their treatment.
If found early, theres a good chance these sores will heal in a few days, with little fuss or pain. Without treatment, they can get worse.
ishonestNo.353 Pores
Youll know theyre better when the sore gets smaller and pink tissue shows up along the sides.
Recommended Reading: Interprofessional Care For Ulcerative Colitis
Summary Of Main Results
We have successfully conducted a network metaanalysis of dressings and topical agents for healing pressure ulcers. Alongside the analysis we have applied a new method of GRADE assessment , which allows us to view the results in the light of our certainty in their findings. Using this approach, we found the majority of the evidence to be of low or very low certainty, and was mainly downgraded for risk of bias and imprecision . This level of uncertainty within the totality of the dataset impacts on all subsequent interpretation of its outputs.
This review includes 51 RCTs involving a total of 2964 participants, comparing 39 different dressings or topical agents for the healing of pressure ulcers. Most of the studies were in older participants, but four included participants with spinal cord injuries and one was in younger people said to be chronically ill or physically disabled. Seventeen studies included participants mainly with Stage 2 pressure ulcers and 15 mainly had Stage 3 pressure ulcers 13 studies investigated treatment of ulcers with a mean duration of less than three months.
We treated each topical agent as a separate intervention, but initially grouped dressings by class as described in the BNF 2016 . The network involved 39 studies in 2116 participants, encompassing 21 different interventions in 27 direct contrasts and these informed 210 mixed treatment contrasts.
Stage 2 Pressure Injury: Partial
In stage 2 pressure injuries there is a partial-thickness loss of skin with exposed dermis. The wound bed is pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Fat and deeper tissues are not visible. Connective granulation tissue and eschar are also not present. Stage 2 injuries are a common result of an adverse microclimate and shear in the skin. For visual reference, see illustrations of pressure injuries from the NPUAP here.
Also Check: Wound Vac For Pressure Ulcers
Stage 3 Pressure Injury: Full
Stage 3 pressure injuries involve full-thickness loss of skin, where fat tissue is visible and granulation tissue, rolled wound edges , and eschar may also be present. However, fascia, muscle, tendon, ligament, cartilage, and bone are not exposed. The depth of tissue damage may vary by anatomical location areas with significant amounts of fat are at risk of developing deeper wounds. For visual reference, see illustrations of pressure injuries from the NPUAP here.
Appendix 6 Assessment Of Risk Of Bias
1. Was the allocation sequence randomly generated?
Low risk of bias
The investigators describe a random component in the sequence generation process such as: referring to a random number table using a computer randomnumber generator coin tossing shuffling cards or envelopes throwing dice drawing of lots.
High risk of bias
The investigators describe a nonrandom component in the sequence generation process. Usually, the description would involve some systematic, nonrandom approach, for example: sequence generated by odd or even date of birth sequence generated by some rule based on date of admission sequence generated by some rule based on hospital or clinic record number.
Unclear
Insufficient information about the sequence generation process provided to permit a judgement of low or high risk of bias.
2. Was the treatment allocation adequately concealed?
Low risk of bias
Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation sequentiallynumbered drug containers of identical appearance sequentiallynumbered, opaque, sealed envelopes.
High risk of bias
3. Blinding was knowledge of the allocated interventions adequately prevented during the study?
Low risk of bias
Any one of the following.
High risk of bias
Any one of the following.
Unclear
4. Were incomplete outcome data adequately addressed?
Low risk of bias
You May Like: Ulcer Cause Blood In Stool