How Is Constipation Due To Ulcerative Colitis Treated
Treatment for constipation depends on the underlying cause. For constipation related to left-sided ulcerative colitis, stool bulking agents or laxatives can help.3 For constipation related to inflammatory bowel disease complications, treating the complication may improve bowel function. Small strictures can be treated with endoscopy. Surgery is used to treat large strictures. Most anal fissures heal on their own. While the fissure is healing, there are things you can do at home to ease the pain. Options include topical pain medication and a sitz bath.9
Ulcerative Colitis Constipation: Tips For Relief
Constipation may be a problem for you if you have ulcerative colitis , an inflammatory bowel disease . According to one study on individuals with ulcerative colitis, nearly half experienced proximal constipation. Proximal constipation refers to constipation that occurs alongside other abdominal symptoms, including abdominal pain, cramping, and the feeling that the bowels have not been completely emptied .
In some cases, UC only affects one side of the colon . Research has shown that people with this form of UC are more likely to experience constipation as a symptom. If you experience constipation with ulcerative colitis, there are several ways you can manage it, at home and with your doctors help.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
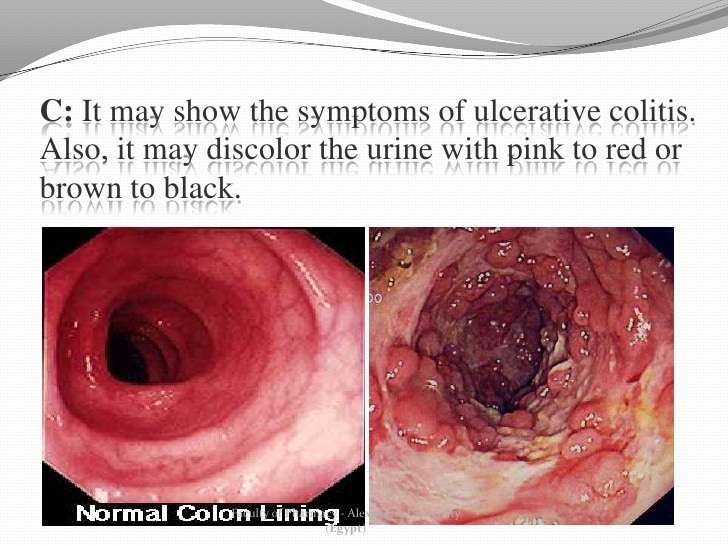
Also Check: Black Tarry Stools Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed
The main clinical symptom of ulcerative colitis, diarrhea with blood or pus, can also occur in other diseases. Diagnostics are, therefore, important in order to confirm the diagnosis and to rule out diseases with similar symptoms .
After a physical examination and a thorough medical history are taken, diagnostic procedures in the following list can be completed when ulcerative colitis is suspected:
- Blood tests: inflammation marker, liver function tests, pANCA
- Colonoscopy : test to determine if there are characteristic inflammatory lesions on the inner lining of the large intestine
- Stool tests: performed to rule out infection and to assess inflammatory markers of the large intestinal mucosa
- Medical imaging: ultrasound, contrast enema , and special MRI exams
With a typical medical history and typical lesions of the intestinal mucosa, an ulcerative colitis diagnosis can be made. The laboratory values are used for orientation in the diagnosis, for example, if the patient’s anamnesis is not clear or symptoms are mild.
What Symptoms And Conditions Can Occur Alongside Ulcerative Colitis
In many cases, ulcerative colitis occurs together with conditions of the skin, liver and bile ducts, joints, and eyes. This is important to know to identify associated conditions as early as possible. If any of these conditions occur, physicians should be vigilant and check for ulcerative colitis. This table summarizes commonly associated conditions:
| Condition | ||
| Inflammation of the fatty tissue under the skin | Painful, red lumps mostly located on the front side of the lower legs | |
| Pyoderma gangrenosum | Rare inflammatory disease of the skin characterized by sores | Small red bumps or blisters evolve into deep skin sores , often with purple edges mostly located on the lower legs |
| Pyostomatitis vegetans | Rare condition with lesions on the inner lining of the mouth | Redness of the oral mucosa with little yellow pimples those can turn into canker sores |
| Iritis, episcleritis, uveitis | Types of eye inflammation | Depend on which part is inflamed eye discomfort or pain due to light , red eye, eye pain, blurred or cloudy vision |
Also Check: What Are Infusions For Ulcerative Colitis
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.
Symptom No : Constipation
Solution: Luckily, constipation isnt very common, but it can cause cramping, bloating, nausea, vomiting, and fewer than three bowel movements a week, according to the American Gastroenterological Association. Try drinking more fluids, adding dried fruit, such as prunes, to your diet, staying physically active, or using suppositories if your doctor signs off on them. You can also ask your provider if adjusting your medication or diet could help relieve your symptoms.
Don’t Miss: Offloading The Diabetic Foot For Ulcer Prevention And Healing
Can Constipation Be A Symptom Of Ulcerative Colitis
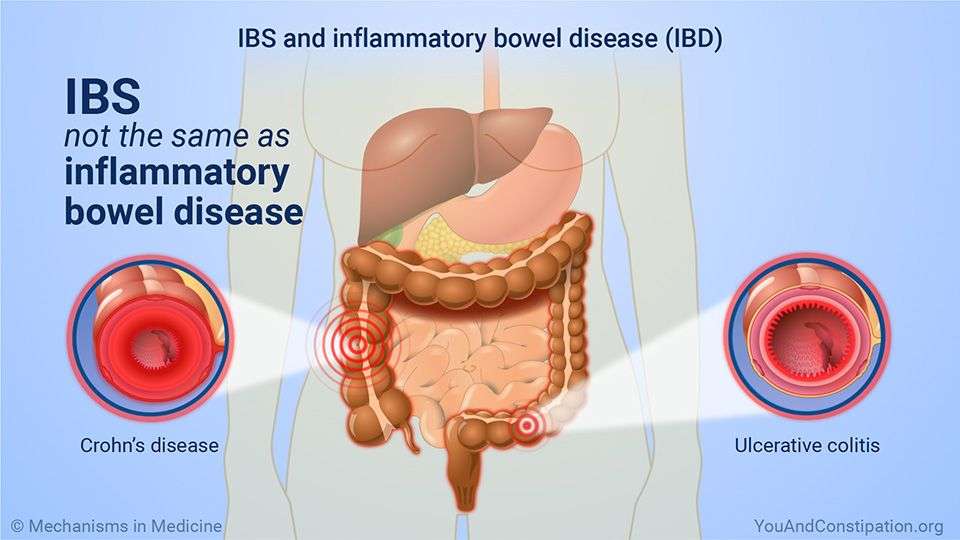
Ulcerative colitis mainly manifests with diarrhea containing blood or pus. However, some people may experience constipation, especially when the condition only affects the last section of the large intestine. Inflammation of the intestinal mucosa in ulcerative colitis can, in rare cases, lead to narrowing of the large intestine . This constriction can also cause constipation. Stenosis is much more common in Crohn’s disease and is not a typical symptom of ulcerative colitis.
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Don’t Miss: Ulcerative Colitis Social Security Disability
How To Identify Ulcerative Colitis Constipation
Constipation is defined in a few different ways:
- Association / Trigger with other Gastrointestinal Symptoms: including gas and stomach pain, which may further complicate Ulcerative Colitis.
Additionally, constipation associated with Ulcerative Colitis may cause further complications such as hemorrhoids and fissures. Hemorrhoids may cause bleeding after a bowel movement, pain while passing stool, and soreness or swelling around the anus. Anal fissures are small tears in the skin that may crack and bleed, and cause pain or itchiness.
Symptom No : Rectal Bleeding
Solution: Stay calm. It probably looks worse than it actually is. If hemorrhoids are the cause, the bleeding will be minimal and can be treated with sitz baths, soluble fiber supplements, or medication, such as steroid suppositories, Dr. Vaughn says. If its caused by an uptick in inflammation, though, you and your doctor may need to adjust your treatment plan.
Until you figure out whats behind your bleeding, consider wearing a sanitary pad or incontinence underwear.
Don’t Miss: What Medicine Is Good For Ulcers
Embarrassing Ulcerative Colitis Symptoms
Gas. Constipation. Bloating. If you have ulcerative colitis, you may not want to share the details of your symptoms with anyone. But in order to start feeling better, you may have to start talking more specifically to your doctor, who can adjust your treatment and recommend ways to ease your symptoms.
Until then, weve rounded up some of the most common symptoms you might be experiencing, along with doctor-recommended tips for finding relief.
Digestive Changes In Ulcerative Colitis
Ulcerative colitis is a chronic condition, meaning it comes on slowly over a long period of time. Currently, there is no known cure for UC.
With UC, inflammation and ulcers develop on the lining of the large intestine . Sometimes the rectum is affected, as well.
This inflammation can cause changes in bowel habits, including urgency, diarrhea, blood or mucus in the stool, and abdominal pain. When your large intestine is inflamed, it contracts and empties often, which is why you may have urgent bowel movements and diarrhea.
When chronic inflammation damages the lining of your colon, ulcers can develop. The ulcers can bleed, leading to blood in your stool. If you regularly lose a lot of blood in your stool, you might develop anemia .
Though diarrhea is more common, some people with UC experience constipation. Inflammation limited to the rectum, known as ulcerative proctitis, may result in constipation.
Other symptoms of UC include painful bowel movements, nausea, vomiting, fatigue, unintentional weight loss, and fever.
Read Also: What Causes Mouth Ulcers On Gums
Can Diet Help Prevent Or Relieve Constipation
According to the Crohns & Colitis Foundation, nutrition is vital to controlling IBD symptoms. Food choices can become more complicated for people with Crohns, because certain foods may worsen symptoms.
A variety of diets have been used to help manage Crohns symptoms or maintain remission, but there is no one tried-and-true diet that works for constipation.
Getting enough fluids, including fiber in the diet, such as soluble fiber like fruits, vegetables, and whole grains, or taking fiber supplements could help, says Adam Cheifetz, MD, director of the center for inflammatory bowel disease at Beth Israel Deaconess Medical Center in Boston. An unprocessed healthy diet without a lot of additives is key, he says.
Increasing fiber should be gradual, cautions Kelly Kennedy, a registered dietitian for Everyday Health, to prevent gas and discomfort.
Fiber is something that many people with Crohns disease limit, so I wouldnt advise going from 0 to 60, but rather increasing little by little until the desired effects are achieved, she says. And during a Crohns flare, patients should limit fiber intake and replace it with foods like white pasta and white rice, even though they are considered to be processed foods. When the flare is over, they can return to gradually increasing fiber intake, Kennedy says.
But Cheifetz says its an intervention worth trying as long as the doctor approves.
How You May Feel
Ulcerative colitis attacks the lining of your digestive tract. It causes swelling and sores in the lining.
If youâve just been diagnosed with it, hereâs what might happen during a flare-up:
You might have some of those symptoms, but not all. And they may change over time. They can range from very mild to very bad.
Also Check: How To Cure Tongue Ulcer
What Are The Symptoms Of Ulcerative Colitis
The main symptom of ulcerative colitis is diarrhea containing blood or pus. The frequency of bowel movements is high. The following symptoms can also occur:
- Painful bowel movements
- Feeling of incomplete bowel emptying
- Urgency to pass bowel movements
- Lower abdominal pain
Serious cases with a sudden, potentially life-threatening evolution can manifest with the following symptoms:
- Severe diarrhea with significant fluid loss
- Severe abdominal cramping
- Significant bulging of the belly with swelling and bloating
- Fever and an increase of inflammatory cells and markers in the blood
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Read Also: Compression Therapy For Venous Leg Ulcers
Focus On Your Gut Health
Introducing more beneficial bacteria into your digestive system can help to keep you more regular. You can do this through taking a probiotic supplement or eating foods high in probiotic bacteria . You should introduce probiotics into your diet slowly to give you digestive system a chance to adjust. The bacteria in your gut likes to feed on fibre, so make sure you are also eating fruit, vegetable, grains, nuts, seeds and legumes too.
How Is It Treated
1. Diet
2. Increased fluid intake
3. Adequate exercise
4. Good habits
5. Laxatives
Also Check: Can I Eat Oatmeal With Ulcerative Colitis
Feeling Comfortable With Your Doctor
Its not always easy to talk about your bowel habits. Talking about poop can be embarrassing, and many people may not be ready to open up to their doctor about it.
Others may ignore the changes to their stool or think that nothing is wrong. However, ignoring symptoms will only make things worse.
Your doctor has studied the gastrointestinal tract along with all that it does and produces. They have seen and heard it all. Nothing you say about your bowel symptoms is going to offend or shock them.
Its part of their job to know about any changes in your symptoms. Your doctor is there to help you, not to judge you.
You dont have to know any fancy medical terms when talking with your doctor about your symptoms. Share your concerns and any changes in your bowel habits you have noticed. Talking with them about changes in your stool can only help get you closer to resolving the problem.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis

Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Also Check: How Do I Know If I Have A Peptic Ulcer
What Makes Yale Medicines Approach To Treating Ulcerative Colitis Stand Out
Our Pediatric Inflammatory Bowel Disease Program team is focused on meeting the complex needs of children with ulcerative colitis. Our IBD specialists, surgeons, and other medical providers are trained specifically in treating children with these diseases. Its a joint program with the nationally-ranked Yale New Haven Childrens Hospital, where the team meets every week to discuss individual patients. We are proud that our remission rates in patients are higher than the national average, Dr. Pashankar says.
We provide lots of practical, emotional, and physical support for families coping with this challenging condition. Our nurse coordinator works closely with you throughout your childs treatment. Our nutritionist discusses appropriate food and diet choices, while a social worker works with your child and family members to cope with any stress or psychosocial issues that may arise at school or work.
We have a smooth transition plan for patients who are 21 and are ready to move into our IBD Program for adults.
Furthermore, we participate in a robust, national quality-improvement project with the goal of improving treatment for children with IBD. Yale Medicine patients also have access to clinical trials not widely available at all treatment centers.
Abdominal And Rectal Pain
People with ulcerative colitis often experience rectal or abdominal pain. Having a large amount of abdominal pain may be a sign that youre having a flare-up or that your condition is getting worse. Pain can range from mild to severe and may also affect your rectum.
Pain may be accompanied by persistent muscle spasms and cramping.
Read Also: How To Heal Leg Ulcers Quickly
Factors Associated With Proximal Constipation
Characteristics of patients in whom proximal constipation had been documented at the study visit and were compared with those without are shown in Table . The majority of patients had active disease at the time of the study visit . Proximal constipation was threefold more likely in women and was significantly associated with distal disease location disease limited to the rectum was present in 50% of subjects with proximal constipation but only 15% of those without and collectively, patients with leftsided colitis had a more than threefold risk. There was no difference between the two groups in terms of age , age at IBD diagnosis , or disease duration . Those with proximal constipation were more likely to be on concurrent rectal aminosalicylates and had higher CAI scores compared to those without proximal constipation at the time of their study visit , .