What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Pain As A Tool For Diagnosis
Because pain can come from different sources, and pain in the abdomen is particularly difficult to pinpoint, it is not a symptom that is normally used to diagnose IBD or a particular form of IBD.
Rather, the type and location of pain is more often used together with other signs and symptoms when diagnosing IBD or other conditions. In other words, it might be a starting point to help a healthcare provider know where to start looking for inflammation, but it’s only one part of the picture.
Be Consistent With Treatment Drugs
Take your medications consistently. Dont miss or skip a dose even when in remission. Dont try to wean yourself off of a treatment drug as these changes can all lead to flares.
Contact Digestive Health Services at if you have any changes to your flares, or if you think you might have ulcerative colitis.
Tags:
Don’t Miss: Budesonide Vs Prednisone For Ulcerative Colitis
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
What Causes Ibd Flare Ups
A colitis flare up is an episode of abdominal cramping, bloody diarrhea, and fever caused by an inflammation in the large intestine, also known as the colon. People with ulcerative colitis , a form of inflammatory bowel disease , can develop colitis flare ups at random or in response to lifestyle or medication changes.
Don’t Miss: How Long Does An Ulcerative Colitis Flare Up Last
More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Read Also: Exercising A Horse With Ulcers
What Is The Outlook
With modern medical and surgical treatment, there is just a slight increase in the risk of death in the first two years after diagnosis, compared with the general population. After this there is little difference in life expectancy from that of the general population. However, a severe flare-up of ulcerative colitis is still a potentially life-threatening illness and needs expert medical attention.
As mentioned, if you do not take medication to prevent flare-ups, about half of people with ulcerative colitis have a relapse on average once a year. This is much reduced by taking regular medication. However, even in those who take regular medication, some people have frequent flare-ups and about a quarter of people with ulcerative colitis eventually have an operation to remove their colon.
A year from diagnosis, about 9 in 10 people with ulcerative colitis are fully capable of work. So, this means that, in the majority of cases, with the help of treatment, the disease is manageable enough to maintain a near-normal life. However, the condition can cause significant employment problems for a minority.
Treatment for ulcerative colitis is an evolving field. Various new medicines are under investigation. These may change the treatment options over the next ten years or so and improve the outlook .
Speak With Your Doctor
Without treatment, people with UC tend to relapse.
For many people with mild or moderate symptoms, things improve somewhat after diagnosis. This is thanks to medication, along with identifying and avoiding triggers.
More aggressive cases are less common, and only a small number of severe cases will require hospitalization.
Repeated flare-ups can indicate problems with your current treatment, so speak with your doctor and discuss adjusting your medication.
Several classes of medication now exist that can help you get into and stay in remission. Your doctor may need to add another type or increase your dosage.
The only way to prevent UC flare-ups is to have surgery. The most common type of UC surgery is the proctocolectomy, which involves the removal of the rectum and colon.
Candidates for UC surgery include people who:
- have sudden or severe disease
- have a perforated colon
- are at risk for colorectal cancer
- are unable to tolerate their UC medications due to side effects
- have stopped responding to their UC medications
In addition to knowing how to manage flare-ups, its also helpful to recognize factors that can trigger your flare-ups.
Also Check: Preventing Pressure Ulcers In Nursing Homes
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Ulcerative Colitis Flares Are Different For Everyone
There are some people who claim to be in the midst of a flare-up and can still work or go to school. Some can still exercise and do regular physical activity.
There are others whose lab work, imaging tests and/or scopes show they should be hospitalized but feel absolutely fine. There are others who can continue with their daily life but feel some on and off the pain, maybe are a little more tired than usual, aren’t as hungry, and just feel kind of blah.
Recommended Reading: Aip Diet For Ulcerative Colitis
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
The Ability To Differentiate Gas From Liquid Or Solid In The Rectum When Urgency Occurs

Participants can be greatly affected by a loss of the ability to differentiate rectal urgency due to gas from rectal urgency due to stool, mucus, or blood. They usually lose this ability during a flare, and need to go to the toilet anytime they have urgency, to avoid the risk of incontinence.
If I do have gas, I dont dare let it pass because all sorts of other stuff could come with it.
When Im having a flare, I cant tell if its gas or not. Gas can carry some other stuff with it. When theres a flareup, I think gas counts because theres no such thing as just gas.
Recommended Reading: Align Probiotic For Ulcerative Colitis
Figuring Out Which Foods Trigger Flare
As the NIDDK explains, although ulcerative colitis isnt caused by diet or nutrition, certain foods can trigger the symptoms or make them worse in some people. The tricky part is figuring out which ones.
Common ulcerative colitis triggers include dairy, high-fiber foods like fruit, vegetables, and whole grains, spicy foods, alcohol, and caffeine, according to the Mayo Clinic. That said, its really individual. Sam has always loved food and says that when it comes to what she can eat now, I have not figured that aspect out. And its not for lack of trying. I feel like I’ve done everything! she tells SELF, explaining that she tries to avoid various food groups like dairy that can trigger symptoms. It doesn’t mean I don’t ever eat them, but I try to avoid them, she says. I’m definitely still experimenting.
Stacey Bader Curry, 48, was diagnosed with ulcerative colitis in March 2020 and is concerned about giving up foods she loves, as well as alcohol and coffee. I’m trying to focus on what I can eat and not what I can’t eat, she says.
To figure out whether certain foods might be triggering your symptoms, the NIDDK recommends keeping a food diary where you record everything you eat and any flare-ups to help you work out what your dietary triggers could be.
Who Develops Ulcerative Colitis
About 2 in 1,000 people in the UK develop ulcerative colitis. It can develop at any age but most commonly first develops between the ages of 10 and 40. About 1 in 7 cases first develop in people over the age of 60 years. Non-smokers are more likely than smokers to develop ulcerative colitis. However, smoking brings other dangers to health which far outweigh this benefit.
Also Check: How To Stop An Ulcerative Colitis Flare
Understanding Ulcerative Colitis Flare
A flare-up is the reappearance of disease symptoms. And for people living with ulcerative colitis , an inflammatory bowel disease , flare-ups can be unpredictable, lasting hours, days, or weeks.
- Frequent and/or urgent bowel movements
- Diarrhea
- Lack of appetite
- Joint and body aches
Because these symptoms may also be caused by something other than UC, it can sometimes be difficult to tell whether you’re experiencing a flare-up. Below, we look at factors that might affect a UC flare-up, and what can help if you are experiencing a UC flare-up.
People Describe How They Were Diagnosed With Ulcerative Colitis
Ulcerative colitis, or UC for short, is a form of inflammatory bowel disease that affects portions or all of your large intestine and rectum. The Centers for Disease Control and Prevention estimates that 3.1 million Americans have IBD, which also includes Crohn’s disease .
UC is a chronic condition that can cause long-term inflammation and ulceration, severe diarrhea, abdominal pain, blood and mucous in your stool, urgency, nausea, joint paint, fever, weight loss, and fatigue. UC is also a risk factor in colorectal cancer, according to the Mayo Clinic. And while there’s no known cure for ulcerative colitis, removal of the colon and rectum in a procedure called a proctocolectomy can eliminate the disease.
Other treatment options include corticosteroids, anti-inflammatory drugs called 5-aminosalicylates, immunosuppressant biologics , and bowel resection or removal. Patients can also manage symptoms with pain medication, anti-nausea medication, and antidiarrheals, though all medications should be taken under the care of a doctor. IBD is often confused with irritable bowel syndrome , a disorder that causes pain and cramping of the large intestine. But unlike IBD, IBS doesn’t cause long-term damage to your intestinal tissue or increase your risk of colorectal cancer.
Managing UC is a complex puzzle of treatment options and unpredictable symptoms. We spoke with nine women to find out what life is like with the disease.
Responses have been edited for length and clarity.
Related:
Don’t Miss: Bland Diet Recipes For Ulcers
Food As Trigger Of Flare
Participants frequently discussed the possibility that certain foods could trigger flares, but had great difficulty in identifying common themes across participants.
I never could figure out what triggers it. When Ive got a flareup going, I mean, its always, I eat, and then half an hour later Im in the bathroom.
I know until I kept a food journal, I had no concept of what would or wouldnt trigger it. I just its hard to isolate.
When To Call Your Doctor
If youre having any of the above UC symptoms, especially bloody stool, endless diarrhea, or severe pain, make an appointment with your primary-care doctor. It could always be something other than UC, but its important to get it checked out.
The sooner you treat UC and work to stop the damage to your intestinal lining and overall health, the better. If your GP suspects UC, they will likely refer you to a gastroenterologist, which is a type of physician specializing in digestive health care. This doc can further evaluate your symptoms, run any necessary tests, and get you a diagnosis.
If youve already been diagnosed with UC, call your gastro if youre experiencing any increase in symptoms like bloody stools, diarrhea, and pain, along with weight loss, fatigue, and fever.
And we totally get it. Talking about UC symptoms with your doctoror anyone!can feel awkward or embarrassing . But its hugely important that youre honest about whats going on so your doctor can get you the best treatment possible.
Read Also: What Causes Ulcers On The Feet
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
What Is Ulcerative Colitis

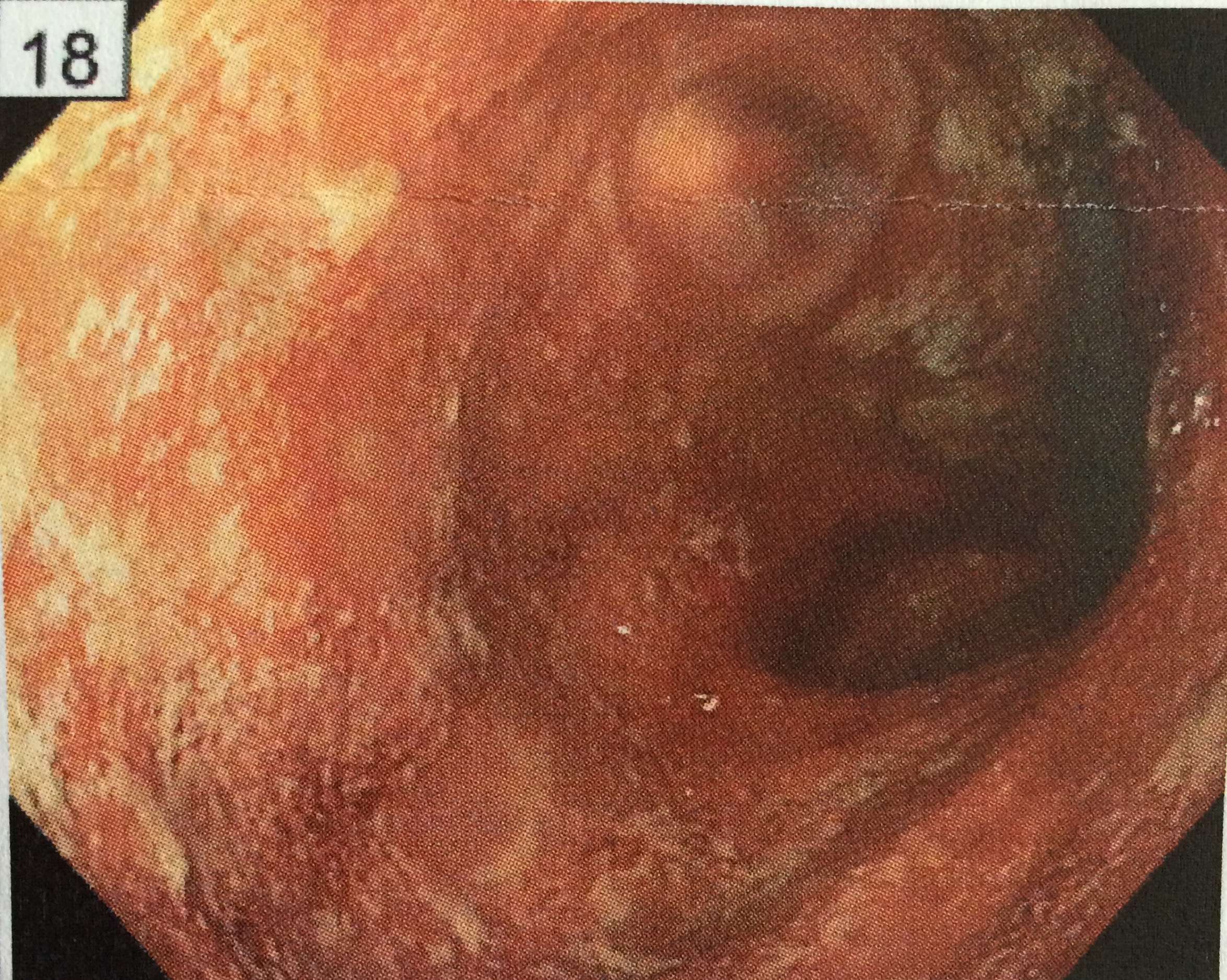
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
The inflammation in ulcerative colitis usually starts in the rectum, which is close to the anus . The inflammation can spread and affect a portion of, or the entire colon. When the inflammation occurs in the rectum and lower part of the colon it is called ulcerative proctitis. If the entire colon is affected it is called pancolitis. If only the left side of the colon is affected it is called limited or distal colitis.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
You May Like: Best Way To Heal Stomach Ulcers