Youre Eating Large Meals
When UC symptoms are active, you can ease your bodys burden by eating frequent, smaller meals so the volume of food and fluid is stable and limited. Consider having five to six fist-sized meals every three to four hours instead of three large meals a day.
On top of helping reduce discomfort from UC symptoms, this strategy is also a way to cope with nausea or loss of appetite that might accompany your flare.
Alcohol And Ulcerative Colitis Flare
Common effects of alcohol can exacerbate IBD symptoms and contribute to the worsening of your condition. One study has found about 75 percent of people reported a worsening of IBD symptoms after consuming alcohol.
Certain properties of alcohol are likely responsible for the increased risk of IBD flare-ups. For example, alcohol is a natural diuretic that can leave you dehydrated and cause diarrhea by stimulating the intestines. Carbonated alcohol beverages can cause you to be gassy. A healthy balance of bacteria in the gut is important for normal digestive functions, but alcohol can disrupt the amount, diversity, and balance of bacteria in your GI tract. Alcohols irritation of the GI tract lining can also lead to rectal bleeding and poor nutrient absorption in some people.
Studies have shown that alcoholic beverages that contain a large amount of sugar, in particular, may increase abdominal pain and discomfort among people who have UC. A MyCrohnsAndColitis team member noticed the same effect with sugar, stating that Sugar in alcohol gets me every time. Sparkling wine is reported to be well-tolerated by people with ulcerative colitis, compared to other alcoholic beverages.
The consumption of red wine has also been linked to long-term risk for relapse and flare-ups in people with inactive UC due to an increase in permeability in the intestines.
- Anemia
- Gastritis
- Malnutrition
What Is The Effect Of Alcohol On Ulcerative Colitis
The effect of alcohol on ulcerative colitis will vary based on each individual. Since alcohol is a known irritant of the digestive tract, many people experience flare-ups of stomach pain, inflammation, gas, and other digestive upset after drinking an alcoholic beverage. Some may be able to handle one or two drinks with no problems, while others can take a few sips and soon experience an onset of symptoms. This will depend on each person and the severity of their condition and their individual makeup.
Ulcerative colitis is caused by inflammation of the colon which can eventually lead to ulcers and lesions. This causes severe pain in many people and can lead to digestive upset, stomach pain, constipation, and other uncomfortable side effects. Certain foods are known to trigger symptoms, and these items will be different for each sufferer. This why the effects of alcohol on ulcerative colitis are different for everyone.
Read Also: Foods Bad For Ulcerative Colitis
Causes Of Ulcerative Colitis
There is still some debate as to the exact cause of ulcerative colitis. In the past it was believed that stress was a major reason for the condition, but this has not been supported by evidence. It is likely that the condition is due to a number of different factors combining together including:
* It is likely that genetics plays a role in the development of ulcerative colitis. Those who have a parent or sibling with UC are more likely to develop the condition.* It is also likely that this condition is originally triggered by some type of infection.* It may occur because the immune system is mistakenly triggering an inflammatory response to kill a pathogen that is not there.* Certain types of diet may encourage such inflammation* Those who are of Ashkenazi Jewish decent seem to be more likely to develop the condition. White people also have a higher risk of developing UC than non-whites.* Those who are under thirty years of age have a higher risk of developing UC.* Those individuals who have taken the drug Isotretinoin seem to be more at risk.
Alcohol And Trigger Flares
Alcohol, caffeine, spicy food and other irritants are known to cause and prolong flares for people with UC. Sadly, UC is an incredibly difficult disease to live with, and alcohol consumption is a modifiable risk factor that can make the disease easier to live with.
If you or someone you know needs alcohol rehab treatment for abuse or addiction and they have ulcerative colitis , The Recovery Village can help. Alcohol cessation can help control symptoms of UC and make it more manageable. To take the first step toward recovery, call The Recovery Village today.
- Sources
The Mayo Clinic. Ulcerative Colitis Symptoms and Causes. 2018. Accessed 29 Apr. 2019.
Medical Disclaimer: The Recovery Village aims to improve the quality of life for people struggling with a substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare provider.
Also Check: How Do I Know If I Have A Peptic Ulcer
When Could Drinking Be Problematic
Some people may feel that they cant control their drinking, have negative feelings when they dont drink, or generally feel that their alcohol consumption is negatively impacting their life. These factors may be signs of alcohol use disorder. If you feel as though you cant limit how much you drink or you continue drinking even though its hurting you or those around you, its time to talk to your doctor.
Whether you decide to continue your current alcohol intake, reduce your alcohol consumption, or eliminate alcohol altogether, its important to listen to your body and have open conversations about these topics with your health care team. They are your best resources for getting medical advice when it comes to limiting the negative effects alcohol has on you and your life.
Selection Of Genetic Variants For Mendelian Randomization
Overall, 540 Linkage Disequilibrium-independent SNPs that were genome-wide associated with the 3 risk factors were selected. shows the sample size of a GWAS meta-analysis for CD and UC used in the current study for the extraction of summary results for those 540 SNPs. shows a schematic representation of the current MR analysis and the number of SNPs selected for each exposure phenotype. Summary data for the estimates of the associations of the genetic variants with smoking, coffee consumption, and alcohol consumption respectively are presented in Supplementary Tables 16. The estimates of the associations of the genetic variants with the risk for CD and UC are also presented in Supplementary Tables 16. These SNPs were all genome-wide associated with each exposure phenotype, but none was genome-wide associated with any IBD type risk at a genome-wide level. The selected SNPs are relatively strong instruments for the corresponding addictive risk factor, with F statistic values greater than the recommended threshold of 10with the exception of one SNP associated with coffee consumption, which has an F statistic value of 9.
Read Also: Ulcerative Colitis Medication Not Working
How Alcohol Affects The Body
Alcohol is considered a depressant – it slows down functions in the body such as speak, movement and reactions. The more alcohol that is drunk the more likely you are to feel these effects. It is absorbed into the bloodstream meaning its effects can be felt very quickly.
It is addictive and it is possible to overdose on it which can lead to death.
Chronic alcohol use can cause a number of serious long-term conditions including liver disease, nerve damage, brain damage, deficiencies, malnutrition and cancer of the mouth and throat.
Youre Avoiding Certain Healthy Foods
It can be hard to eat a healthy diet or anything at all if youre experiencing abdominal pain, cramps, or nausea. But if youre not eating the right foods, you could be at risk of nutrient deficiencies, malnutrition, and unwanted weight loss.
While theres no one meal plan that works for everyone, many people find they can tolerate low-fiber fruits , lean proteins, cooked veggies, and grains like sourdough and oatmeal. A doctor or dietitian who specializes in IBD can help you develop a personalized meal plan.
Read Also: What To Avoid With An Ulcer
Effect Of Alcoholic Intoxication On The Risk Of Inflammatory Bowel Disease: A Nationwide Retrospective Cohort Study
-
Affiliations Department of Emergency Medicine, China Medical University Hospital, Taichung, Taiwan, School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan
-
Affiliations Department of Emergency Medicine, China Medical University Hospital, Taichung, Taiwan, School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan
-
Affiliations School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan, Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
-
Affiliations Department of Emergency Medicine, Chang Gung Memorial Hospital, Chiayi, Taiwan, Department of Nursing, Chang Gung University of Science and Technology, Chiayi, Taiwan
-
Affiliations Graduate Institute of Clinical Medicine, National Taiwan University College of Medicine, Taipei, Taiwan, Department of Dermatology, National Taiwan University Hospital Yunlin Branch, Douliou, Taiwan
-
Affiliations Department of Emergency Medicine, China Medical University Hospital, Taichung, Taiwan, School of Medicine, College of Medicine, China Medical University, Taichung, Taiwan
Lifestyle Changes To Manage Ulcerative Colitis
There are things that people with UC can do to reduce the chances of inflammation including:
* Avoiding excessive use of alcohol. It is a good idea to take a break from drinking alcohol to see if this reduces the severity of symptoms.* Those who are lactose intolerant should avoid too much dairy products.* The individual is likely to find that certain foods will exacerbate their symptoms and this can differ between people. Keeping a food diary will allow people to see which food items need to be avoided.* Avoid too much caffeine as these drinks can exacerbate diarrhea.* It is best to eat regular small meals rather than large ones.* Some people benefit from adding more fiber to their diet while for other people this may make their symptoms worse.* Stress may not cause UC but it is still likely to exacerbate the symptoms. It can therefore be highly beneficial to learn some relaxation techniques in order to deal with stress more easily.
Don’t Miss: How To Get Remission In Ulcerative Colitis
No Link Between Alcohol Use And Ibd
Through 5.1 million person-years of follow-up, there were 370 cases of Crohns disease and 486 cases of ulcerative colitis identified.
And overall, increased alcohol consumption was not linked to cases of Crohns disease or ulcerative colitis .
In addition, the multivariable-adjusted HRs for 15.0 + g/day of alcohol intake group were 0.84 for Crohns disease and 1.08 for ulcerative colitis, compared to non-users.
The investigators also analyzed alcohol subtypes and found only moderate consumption of beermore than 1-4 servings per weekwas marginally associatied with a reduced risk of Crohns disease. However, more than 4 servings per week of liquor was associated with an increased risk of ulcerative colitis.
This prospective study did not identify a relationship between overall alcohol consumption and risk of CD or UC, the authors wrote. Our suggestive associations between alcohol types and risk of CD and UC deserve additional investigation.
Lifestyle Changes To Prevent Ulcerative Colitis
Dealing with colitis flare-up can be approached different ways. Some people have reported that herbal remedies help manage their symptoms. Probiotics, the spice turmeric, and the herb boswellia have been used to control ulcerative colitis. Studies have also shown that gingko biloba has been effective in treating colitis in rodents.
Since stress has been linked to the disease, exercises like yoga and meditation are often recommended to patients. At the same time, certain foods have a higher chance of aggravating ulcerative colitis, so obviously avoiding such food items is a good idea. Some examples of foods to stay away from are whole-grain bread, whole-grain pasta, beans, raw vegetables, and dried fruit. Keeping a diary of what you eat can often help you pinpoint the exact cause of a flare-up.
A diary or journal can also help when you are taking medications. For example, if you experience a flare-up while taking an over-the-counter medication, ask your doctor and/or pharmacist about a possible alternative.
Controlling ulcerative colitis flare-up can take time. Some people will have multiple triggers and wont be able to make all the necessary lifestyle adjustments all at once. Sometimes, just a few changes can make a huge difference though. The following simple steps have proven to help many people tame their flare-ups:
- Drinking small amounts of water throughout the day
- Reducing fatty foods
- Eating smaller meals throughout the day
- Lowering intake of milk
Recommended Reading: Stage 2 Pressure Ulcer Treatment Dressing
Youre Skipping Your Uc Medications
The most important thing to do if you have UC? Take your medications as prescribed and work closely with your doctor to stay well, says Richard Bloomfeld, MD, a gastroenterologist and professor at Wake Forest Baptist Medical Center in Winston-Salem, North Carolina.
A variety of medications can treat UC, depending on the severity of your condition and your overall health. It may be tempting to skip doses once you start feeling better: A Canadian review published in January 2013 in the journal Gastroenterology found that out of 1,681 people with UC, the majority did not adhere to their treatment after one year.
Skipping medications is the biggest reason people experience flares, says Laura Yun, MD, a gastroenterologist and assistant professor of medicine at Feinberg School of Medicine at Northwestern University in Chicago. Whether your doctor has you taking an anti-inflammatory drug, an immunosuppressant, or a combination of medications, none of them will work if you dont take them as your doctor prescribes.
Treatment Of Ulcerative Colitis
The goal of treatment for UC is to avoid inflammation and the best approach to this will be decided by the severity of the symptoms. The most common form of treatment for the condition is drugs such as:
* Anti-inflammatory drugs work by reducing inflammation in the body. The usual anti-inflammatory drugs used to treat UC include corticosteroids, mesalamine, and sulfasalazine.* Immune system suppressors such as azathioprine and cyclosporine work by preventing the inflammatory response occurring in the first place.* It can be necessary for people to take other medications for their UC including anti-diarrhea medication, antibiotics, iron tablets , and pain relievers.
If medications are unable to keep the inflammation at bay it may be necessary to perform surgery. This may involve removing the entire colon and rectum. Once the procedure is performed the individual will need to wear a colostomy bag. There is usually no further inflammation after the surgery.
You May Like: Black Tarry Stools Ulcerative Colitis
Is Alcohol An Ulcerative Colitis Trigger
As a 30-year sufferer of ulcerative colitis, I understand the reality of certain foods and drinks not agreeing with the body. Ive lived most of my life like this. Watching what hurts and doesnt hurt my colon. Avoiding all “trigger foods.”
But what about drinking? Does drinking alcohol make UC symptoms worse?
I began mulling over these questions as I handed my son some Imodium.
At the simplest level, my brain says that alcohol would just irritate an already inflamed colon. But is that the case for everyone?
Youre Not Drinking Enough Fluids
If youre experiencing a bout of diarrhea, you run the risk of becoming dehydrated because your body is losing more fluids than its taking in. This can be harmful to your overall well-being and interfere with your bodys ability to heal.
Drink as much water as you can during a UC flare. Just keep in mind that there are some liquids you should think twice about if you have diarrhea, including pear, peach, or prune juice, according to the Crohns and Colitis Foundation all of them contain nonabsorbable sugars that can be rough on your gut.
Recommended Reading: What Not To Eat With Bleeding Ulcers
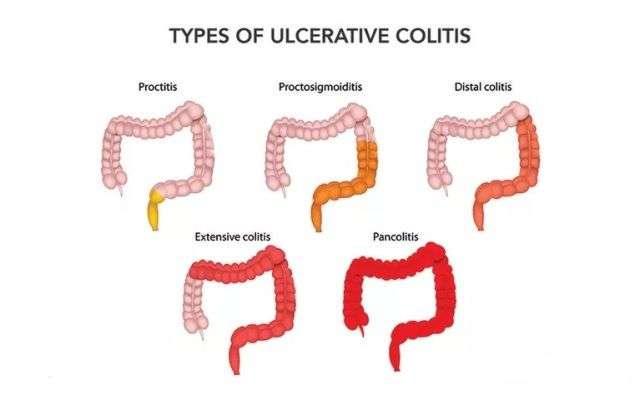
Types Of Ulcerative Colitis
* Ulcerative proctitis involves inflammation of the rectum.* Universal colitis involves inflammation of the entire colon.* Fulminant colitis is a rare form of universal colitis that can be life threatening because it is such a severe inflammation.* Prostosigmoiditis means an inflammation to the sigmoid colon as well as the rectum.* Left sided colitis begins at the rectum and moves in the direction of the left colon.
Extraintestinal Manifestations And Complications
Aphthous ulcersPyoderma gangrenosum
UC is characterized by immune dysregulation and systemic inflammation, which may result in symptoms and complications outside the colon. Commonly affected organs include: eyes, joints, skin, and liver. The frequency of such extraintestinal manifestations has been reported as between 6 and 47%.
UC may affect the mouth. About 8% of individuals with UC develop oral manifestations. The two most common oral manifestations are aphthous stomatitis and angular cheilitis. Aphthous stomatitis is characterized by ulcers in the mouth, which are benign, noncontagious and often recurrent. Angular chelitis is characterized by redness at the corners of the mouth, which may include painful sores or breaks in the skin. Very rarely, benign pustules may occur in the mouth .
UC may affect the eyes. Inflammation may occur in the interior portion of the eye, leading to uveitis and iritis. Uveitis can cause blurred vision and eye pain, especially when exposed to light . Untreated, uveitis can lead to permanent vision loss. Inflammation may also involve the white part of the eye or the overlying connective tissue , causing conditions called scleritis and episcleritis. Uveitis and iritis are more commonly associated with ulcerative colitis, whereas episcleritis is more commonly associated with Crohn’s disease.
Read Also: What Foods Should I Avoid With A Stomach Ulcer