Avoid Sources Of Carrageenan
Carrageenan is a food additive derived from seaweed. Its used to thicken and preserve many foods, including some coffee creamers .
In a small 2017 study, 12 people with UC were told to avoid all sources of carrageenan in the diet. Half received a placebo while the other half received carrageenan. Participants were interviewed every 2 weeks and followed for a year or until relapse (
21 ).
Although interesting, this is just a small, preliminary study, and it only showed marginal differences in UC outcomes. Ultimately, more research is needed to learn more especially since carrageenan is not commonly consumed in supplement form.
Summary
Keeping a diary of the types and quantities of foods and drinks you consume can help identify potential triggers of your symptoms.
Cooked And Peeled Vegetables
Many vegetables are high in fiber, but as with fruit, peeling them removes a layer of insoluble fiber.
Some vegetables do not need peeling, such as asparagus tips and mushrooms, but it can help to remove the skins of potatoes, carrots, and squash.
Cooking vegetables also makes them easier to digest, and it can reduce the fiber contents.
However, avoid roasting or frying vegetables in oil or butter, because fats can irritate the digestive system and worsen symptoms of Crohns. Try boiling or steaming them instead.
When Youre In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
You May Like: What Are The Signs Of A Bleeding Stomach Ulcer
Supplements And Other Lifestyle Changes To Try
Besides diet and medicine, there are a few other therapies that could be helpful for people with ulcerative colitis.
Dr. Singh suggests focusing on adequate sleep and reducing stress to prevent flares. One of the most common causes of flare can be stress, so stress reduction is probably the best medicine I talk about when I see patients, he says.
There is also limited research surrounding the use of certain supplements and probiotics as a therapy for IBD, but more evidence is needed before recommendations are made12,13.
General Guidelines When Ulcerative Colitis Is In Remission
Some members of MyCrohnsAndColitisTeam find they can eat a wider variety of foods safely during remission periods when ulcerative colitis is not as active and symptoms are absent or mild. Still, every individual is different, and purportedly beneficial foods may trigger symptoms. Trial and tracking is the only way to know for sure.
If it is safe for you, these guidelines may help you stay your healthiest during remission:
- Get 25 grams to 35 grams of fiber per day to promote bowel regularity and reduce inflammation.
- Consume plenty of lean meats, which are a good source of B vitamins. Include fatty fish, tofu, and nut and seed butters.
- Include probiotic foods such as yogurt, tempeh, kefir, kimchi, miso, and sauerkraut.
While some members find kefir too sour for their liking, others report experiencing benefits from trying the fermented drink. Kefir has been helping me over the past week, wrote one. Been trying kefir the past few days. Will keep you posted. So far less pain, said another.
Don’t Miss: Does Ulcerative Colitis Increased Risk Of Colon Cancer
What To Eat During An Ulcerative Colitis Flare
Research shows that nutrition cant cause or cure ulcerative colitis. There are no foods that can cause someone to develop ulcerative colitis, and there is no miracle diet that will cure people of the condition. However, good nutrition does play an important role in the management of ulcerative colitis symptoms, especially during a flare.
Ulcerative colitis flare-ups are uncomfortable and frustrating. Pain, bloating, cramping, fatigue, rectal bleeding, and diarrhea are common symptoms during flare-ups. If youre in the midst of the flare, changes in your diet can help control your symptoms and allow your intestine time to heal. If you have a flare
While carefully watching what you eat can help ease symptoms of ulcerative colitis, there are very few treatments for ulcerative colitis currently available. Participating in research is one of the best ways to actively search for a cure. Research helps increase the understanding of ulcerative colitis and trial new treatment options. If you or a loved one has ulcerative colitis, fill out the form below to learn more about a clinical trial that you may qualify for.
Creamy And Greasy Food
Creamy and greasy foods containing loads of mayonnaise, butter, cream cheese, margarine, animal fat, etc. can irritate the inner lining of the colon. This can worsen the ulcers and may cause rectal bleeding. Avoid creamy pasta, macaroni and cheese, and creamy cheese containing foods to pacify your colon.
You May Like: Vsl 3 For Ulcerative Colitis
How To Prep Vegetables For Ulcerative Colitis
Cooked vegetables are often easier to tolerate than their raw counterparts, especially when youre in the middle of a flare. Altering the texture can be helpful, too. You can make veggies easier on your GI tract by:
- Peeling them Peeling vegetables such as carrots, parsnips, turnips, squash, and potatoes strips away some of the insoluble fiber, making them less irritating to the gut, say Warren and Leben.
- Cooking them until soft Methods that make veggies tender without the need for too much added fat tend to be best. Try baking, roasting, steaming, or lightly sautéing, Leben recommends.
- Mashing or pureeing them, if needed Particularly during a flare, purees and very soft textures can be easier to digest. Texture changes can help break down fibrous foods and improve tolerance, says Leben. Try mashing soft-cooked veggies or blending them into soups or smoothies, Warren recommends.
Can Food Cure Crohn’s Or Colitis
You may come across diets that claim to cure Crohns or Colitis, but there isnt any evidence to prove that these work. A healthy, balanced diet will give you nutrients that are important to help you stay well.Some people find that making small changes to their diet, for example avoiding spicy food, helps them cope with their symptoms. If cutting out a food makes no difference to your symptoms, make sure you start eating it again to avoid missing out on important nutrients.There are times when your IBD team or dietitian may advise you to change your diet, for example, after surgery or if you have a narrowing in your small intestine, called a stricture. Some people, such as children or people with Crohns, may benefit from a liquid diet, called exclusive enteral nutrition.Always speak to your GP or a dietitian before making any big changes to your diet.
Ive tried just about all the different diets for Ulcerative Colitis and just gone round in a complete circle, not finding any success, only causing problems and stress! I now realise the most important thing is to eat a balanced diet and enjoy my food!
Trevor
You May Like: Low Dose Naltrexone Ulcerative Colitis
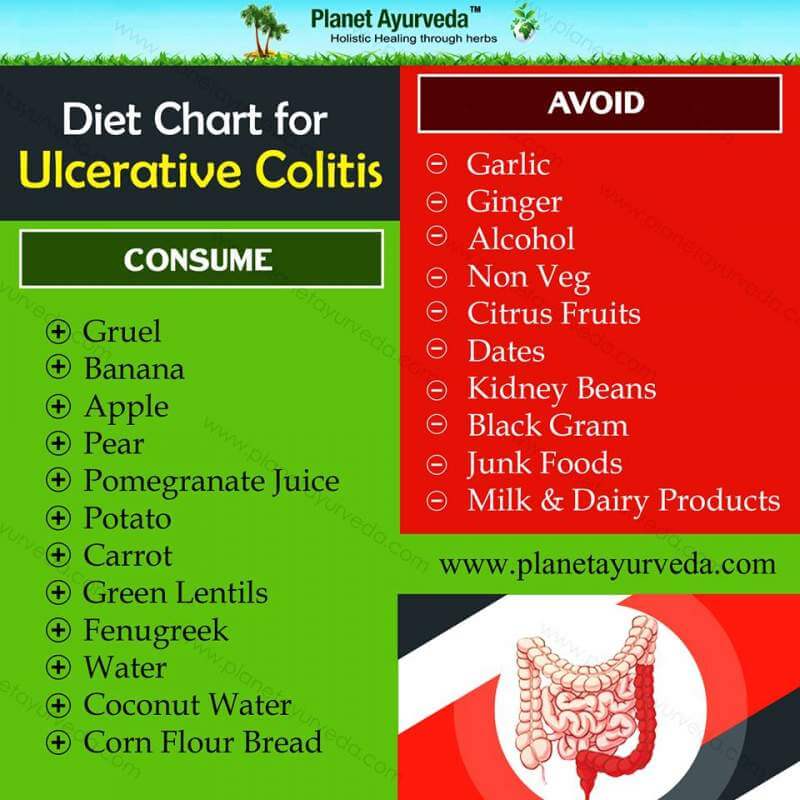
Foods To Eat During Ulcerative Colitis Flares
A bland diet is best during periods of active ulcerative colitis, when you may experience abdominal discomfort, blood in your stool, loss of appetite, fatigue, weight loss, vomiting, nausea, abdominal pain, and diarrhea. A safer diet during flares might include dry toast, applesauce, and white rice. Although some foods are more likely to be safe for those with UC, individual experiences can vary, especially during flares.
Here are some safer foods to try during ulcerative colitis flares:
- Low-fiber refined grains, such as oatmeal, potatoes, and sourdough bread
- Well-cooked vegetables that are easier to digest
- Vegetable broth, which can be added to grains like rice for additional nutrients
- Fruits or vegetables that contain more soluble fiber than insoluble fiber, such as bananas, carrots, and apples
- Bland protein, such as nut butters, eggs, tofu, and chicken
Diarrhea specifically raises concerns for loss of nutrients, such as potassium, sodium, magnesium, and phosphorus, through bodily fluids. If you choose to drink an electrolyte beverage, choose low sugar versions such as G2, Propel, or BodyArmor Lyte. You can also cut regular Gatorade or BodyArmor with water, diluting it by half.
What You Should Know About Food When You Have Ulcerative Colitis
Dealing with a chronic bowel disease like Ulcerative Colitis is often disheartening and frustrating as there is no universal solution in managing your symptoms. Everyones bodies are different, and what works for one person, may not work for another person. Paying attention to your diet and the produce you consume can help you recognize a lot about what your body can and cant tolerate.
When you have an inflammatory bowel disease, its important to source your produce from reputable growers that dont use pesticides or fungicides. A specific pesticide, that goes by the name of glyphosate, is known to be particularly harsh on gut microbes, which in turn could be contributing to discomforting symptoms and amplifying your Ulcerative Colitis symptoms. Changing your diet and sourcing produce without pesticides is one way you can decrease flare-ups.
Another tip given to those who suffer from IBDs is to make sure the produce they consume is seedless, skinless, and low in fiber. High fiber foods are a detriment to your bowel movements as they are hard to digest, cause bloating, and may cause a flare-up. Cooking veggies and fruits you consume, whenever possible, may also help prevent a flare-up. Boiling, baking, or roasting your produce may help break down dietary fiber, making it easier for your intestines to digest.
Also Check: What Causes Ulcers In Your Stomach
Active Left Sided Disease And Extensive Disease
Doses of oral mesalazine > 3 g a day are associated with greater clinical improvement than lower doses. Combined topical and oral treatment can help induce remission in left sided colitis and extensive colitis., Oral corticosteroids are indicated in mild disease that fails to respond to topical treatment and in moderate disease .
Delays in treatment may increase the risk of colectomy. Patients should be treated promptly with an optimal dose of corticosteroids .
Natural Remedies For Uc Flares
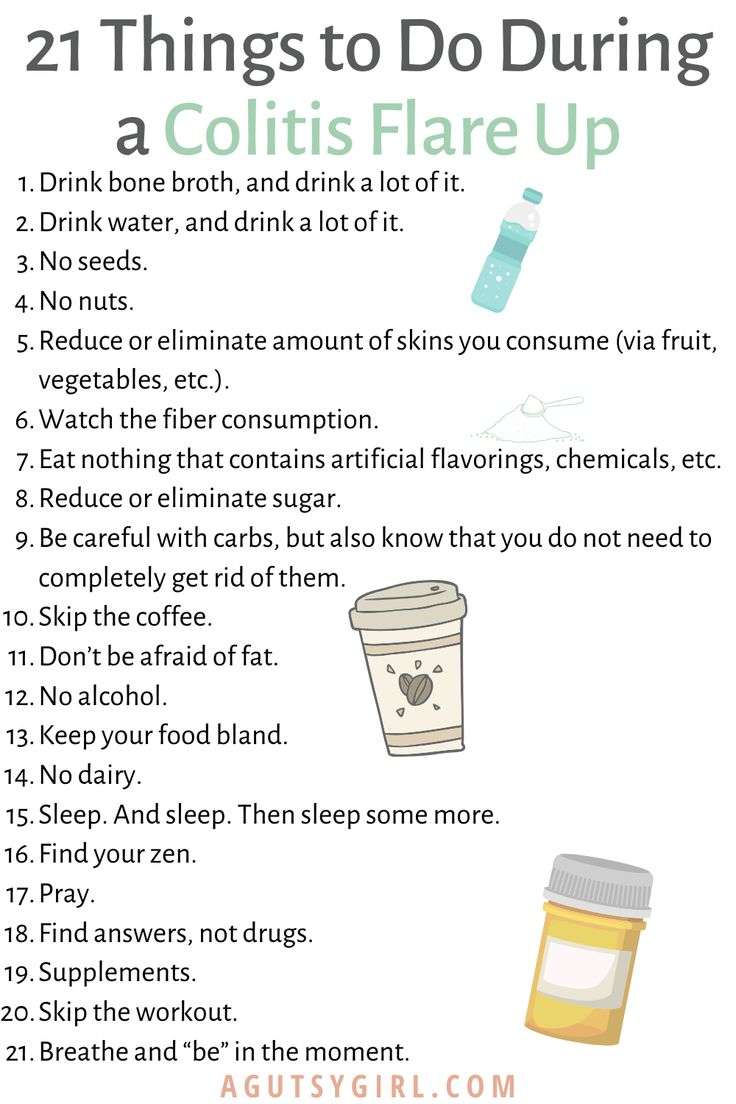
Natural remedies are being studied, but none have been proven yet. The National Center for Complementary and Integrative Health notes that supplementing your standard treatments with meditation may be beneficial during a UC flare-up to help reduce symptoms, and that prebiotics and probiotics have shown promise in bringing about remission and helping people stay in remission when added to usual care.
Still, ulcerative colitis is a chronic, incurable condition, and symptoms may reappear unpredictably.
Recommended Reading: What To Drink With Ulcerative Colitis
You May Like: Diet For Gerd And Ulcers
Best Foods To Eat During An Ulcerative Colitis Flare
HomeUlcerative Colitis7 Best foods to eat during an ulcerative colitis flare-ups
Ulcerative colitis is a long-lasting condition that causes inflammation and ulcers in your digestive tract. It usually affects the innermost lining of your large intestine and the rectum. Symptoms of ulcerative colitis develop over time, rather than all of sudden.
The food you eat has a great impact on the severity of your Ulcerative colitis symptoms. If you have ulcerative colitis, you may already identify various foods as triggers. But figuring out what foods to eat is also equally important as the right foods will provide you key nutrients without irritating your digestive tract.
I Have Heard That Fiber Is Good For Ulcerative Colitis What Does Onpoint Say
-
We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well
-
If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently
-
You may find a “Low Residue” approach helpful. We have seen it work well for some people
-
Increase or be aware of hydration and fluid intake. Try to drink at least 64 oz of water per day
-
Some studies show that a higher fiber diet can improve IBD conditions
You May Like: Sacral Dressings To Prevent Pressure Ulcers
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
To Avoid: High Fiber Foods
Foods that are high in fiber might be a challenge during an IBD flare-up. Most Americans don’t get enough fiber and need to eat more. During an IBD flare-up, however, fiber might not be tolerated well. High fiber foods include brown rice, wild rice, popcorn, barley, oats, and anything made with whole wheat. These foods could be added back into the diet when a flare-up is over but might need to be excluded for a time while a flare-up is going on.
Don’t Miss: Natural Treatment Of Ulcer In Hindi
Medical Treatment For Ulcerative Colitis
The key to successful UC treatment is with medications medications are selected based on the severity of the disease, Dr. Abramowitz says.
Patients who are symptom-free are said to be in remission. When symptoms do occur, its called a flare or flare-up. For a mild flare-up, budesonide MMX is recommended. For a moderate-to-severe flare-up, Dr. Abramowitz says a typical treatment includes a course of prednisone that is tapered off over six to eight weeks.
Are There Common Foods To Avoid If You Have Ulcerative Colitis
Okay, so weve established that there are no surefire foods to avoid that will reduce or eliminate ulcerative colitis symptoms. But there are some foods that you could try to avoid during a flare-up until your bowels calm down. Those include:
Many people hail fiber as a magical nutrient that can lower your risk of developing heart disease, type 2 diabetes, and potentially offer some protection against Crohns disease flaresanother type of IBD. And, well, loading up on fiber can aid in all of those things.
However, some people with ulcerative colitis may want to avoid a high-fiber diet, depending on their symptoms, according to the Crohns & Colitis Foundation. If diarrhea is a hallmark of your ulcerative colitis, you may want to eat less insoluble fiber because it moves food through the intestine quicklywhich only makes the problem worse. To reduce your insoluble fiber intake, you may want to lay off beans and other legumes like chickpeas or lentils, cruciferous vegetables like cauliflower or kale, nuts, and whole wheat flour in your diet to see if your symptoms improve3.
Initially, the low-FODMAP diet is very restrictive: The idea is to cut out all FODMAPs before slowly reintroducing some to determine which you can tolerate. So, its important to work with your health team when making any dietary change to avoid nutritional deficiencies.
Recommended Reading: Is Ulcerative Colitis The Same As Diverticulitis
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Recommended Reading: Hind Gut Ulcers In Horses Symptoms
Gluten And Dairy Foods To Avoid

- Any product that contains gluten. Make sure to read the ingredients list before purchasing a product.
- Any product that contains dairy. Make sure to read the ingredients list before purchasing a product.
- Dairy products like milk, ice cream, cheese, and yogurt
- Cereal, white bread, wheat bread, and any bread that isnt gluten-free
- All alcohol except some wines, seltzers, and ciders
Read Also: Is Milk Good For Ulcers