Supplements For Ulcerative Colitis
Because ulcerative colitis may interfere with your ability to absorb nutrients, its important that you use supplements to ensure that your body gets the vitamins and minerals that are necessary. Some supplements that may be helpful when combating the symptoms of ulcerative colitis include:
Practical Advice For What To Eat On An Ulcerative Colitis Diet
Many organizations post food shopping lists for Ulcerative Colitis Disease. These resources are a good starting point. Download a list and make it your own. Mark off your trigger food and add foods that you can safely eat.
Plan ahead and enhance your weekly menus with MealPro Ulcerative Colitis meal delivery service. These anti-inflammatory meals are designed to eliminate known trigger foods and reduce flares.
Roasted salmon: This meal is full of flavor while providing healthy omega-3s with a portion of asparagus and yellow bell peppers. Roasted potatoes round out the meal for a satisfying choice in carbs.
Turmeric Turkey: Lean turkey seasoned with the anti-inflammatory spice turmeric. Served with fresh green beans and bake yams. Rice is the foundation of this meal.
So, can Ulcerative Colitis symptoms change the way you eat? Yes. Although it is possible to adjust the foods you eat to improve and enhance your quality of life.
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Don’t Miss: How Do You Heal An Ulcer
What Should I Eat During A Flare
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Its best to work with a professional when making changes to your diet, as they can ensure that you are getting the nutrients that you need, help you assess your trigger foods, and address any underlying history of disordered eating or dietary changes that could trigger those behaviors.
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
You May Like: How Can You Cure An Ulcer
Can Food Cause Crohn’s Or Colitis
We dont know what causes Crohns and Colitis but we do know that a combination of the following factors are likely to play a part:
- Genetics
- A problem with the immune system, where the body attacks its own cells
- Changes in the bacteria in the gut.
These, together with environmental factors, like food and stress, may trigger the conditions.There isnt any clear evidence that specific foods cause Crohns or Colitis. Some researchers think a diet low in fruit and vegetables may increase the risk of Crohns and a low intake of vegetables may increase the risk of Colitis for some people. Theres also some evidence that eating a lot of meat or table sugar, called sucrose, may increase the risk of Crohns and Colitis. But there isnt enough evidence yet to say for certain whether food affects the risk.
Dietary Advice For Ulcerative Colitis
Please note, this page is printable by selecting the normal print options on your computer.
What is Ulcerative Colitis?
Ulcerative Colitis is a form of Inflammatory Bowel Disease . IBD is a term used to cover a number of inflammatory conditions of the gastrointestinal tract. UC causes inflammation in the large bowel and can affect the rectum, part of, or the entire colon. If you have UC this diet sheet may help you.
Can diet help?
Diet is not a cause of UC however diet can help to relieve symptoms such as diarrhoea during a flare up and maintain good health including healthy bones. You may find as time goes by you begin to notice that certain foods aggravate your symptoms of UC and so they are best avoided. However, do not remove whole food groups as this could mean you lose some vital nutrients. The main food groups are demonstrated below in the Eatwell Guide.
What foods are beneficial for UC during a flare up?
Soluble FibreDietary fibre can be categorised into two forms, soluble and insoluble. Soluble fibre is partially digested in the large intestine to form a glue like substance, which helps to produce soft/formed stools, without causing inflammation. Examples of foods rich in soluble fibre are:
- Oats e.g. Porridge oats/Ready Brek ®, oatcakes
- The body of fruits and vegetables e.g. peeled apples and pears, tinned fruit, peeled root vegetables such as carrots, parsnips, turnip
What foods may worsen UC during a flare up?
Dairy foods
Spicy foods and fatty foods
Also Check: Symptoms Of Ulcer In Female
Foods To Eat During Ulcerative Colitis Flares
A bland diet is best during periods of active ulcerative colitis, when you may experience abdominal discomfort, blood in your stool, loss of appetite, fatigue, weight loss, vomiting, nausea, abdominal pain, and diarrhea. A safer diet during flares might include dry toast, applesauce, and white rice. Although some foods are more likely to be safe for those with UC, individual experiences can vary, especially during flares.
Here are some safer foods to try during ulcerative colitis flares:
- Low-fiber refined grains, such as oatmeal, potatoes, and sourdough bread
- Well-cooked vegetables that are easier to digest
- Vegetable broth, which can be added to grains like rice for additional nutrients
- Fruits or vegetables that contain more soluble fiber than insoluble fiber, such as bananas, carrots, and apples
- Bland protein, such as nut butters, eggs, tofu, and chicken
Diarrhea specifically raises concerns for loss of nutrients, such as potassium, sodium, magnesium, and phosphorus, through bodily fluids. If you choose to drink an electrolyte beverage, choose low sugar versions such as G2, Propel, or BodyArmor Lyte. You can also cut regular Gatorade or BodyArmor with water, diluting it by half.
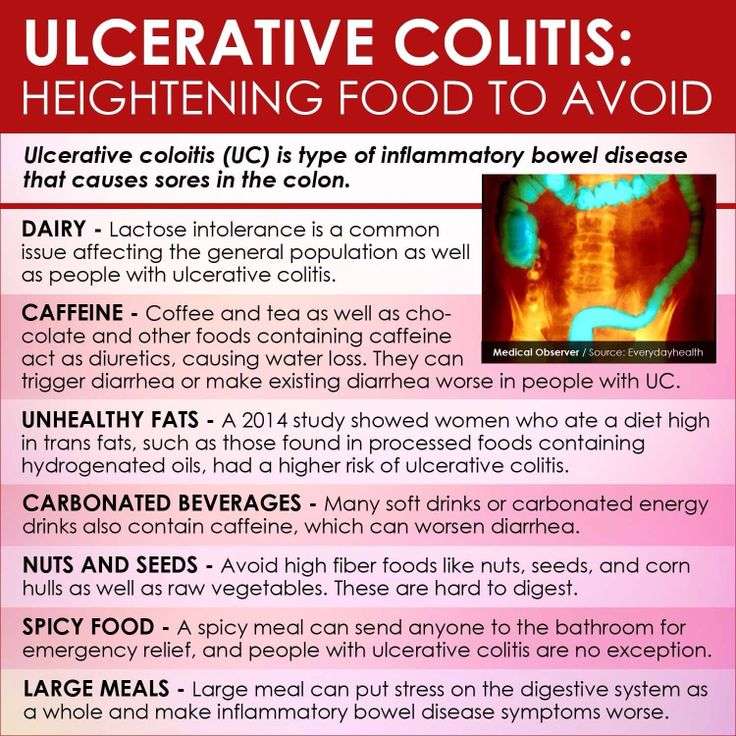
The Worst Foods For Those With Ulcerative Colitis
Ulcerative colitis is an inflammatory chronic disease of the colon and rectum where ulcers develop inside the lining of the large intestine. It is an inflammatory bowel disease along with Crohns Disease which causes a multitude of painful and unpleasant symptoms. Since dietary habits can contribute to ulcerative colitis symptoms, lets look at the worst foods for those with ulcerative colitis.
You May Like: Is Kimchi Good For Ulcerative Colitis
Can Veganism Really Benefit Ulcerative Colitis
We hear all the time how going vegan is better for you and the environment. Many say it can give you more energy, especially for those with chronic illness. It may not be a diet that is appealing to our cheese lovers of the world, but perhaps there is some truth to it. Dairy can be a bit too harsh on the digestive tract for many people, even those without UC, and meat takes a lot of work for the body to digest. For people with UC, these foods can be even more harsh on the body. Avoiding dairy and meat can give your digestive tract a much-needed rest.
One article also suggests that eliminating foods that contribute to inflammation is also key. This makes sense as UC is an inflammatory disease, but what are foods that contribute to inflammation? The Arthritis Foundation highlights some ingredients that are considered inflammatory. Since both arthritis and UC are autoimmune inflammatory diseases, these foods could have an effect on both conditions. The ingredients that they discuss are commonly found in processed foods such as breads and cereals, as well as animal product and dairy products. They include saturated and trans fats, sugars, gluten, and more. Alcohol is another product that can cause inflammation.
Should People With Ibd Be Concerned About Fluid Intake
Yes. In a condition with chronic diarrhea, the risk of dehydration always exists. If fluid intake does not keep up with diarrhea, kidney function may be affected. Patients with Crohn’s and other diarrheal diseases have an increased incidence of kidney stones, which is related to this problem. Furthermore, dehydration and salt loss create a feeling of weakness. For these reasons, people with IBD should consume ample fluids-especially in warm weather when loss of salt and water through the skin may be high. A good rule of thumb is to drink one half ounce per day for every pound of body weight. That means that if you weight 140 pounds, you should drink at least 70 ounces a day — or eight and three-quarters glasses. Sip your beverages, rather than gulp them. By introducing air into the digestive system, gulping can cause discomfort.
Read Also: How To Stop Ulcerative Colitis Pain
What To Eat During Flare
Low-fiber foods are easiest to digest and are less irritating to the gut, especially with symptoms like abdominal pain or diarrhea. Choose:
- Grains/starches: White foods, instead of wheat or whole-grain, and those with less than 2 grams of fiber per serving
- Cooked vegetables: Well-cooked vegetables such as green beans, carrots, mashed potatoes without skin, steamed asparagus tips and pureed squash.Use fresh or frozen.
- Canned or soft fruits: Peeled apples, ripe bananas, cantaloupe, honeydew, watermelon, and canned fruit in fruit juice or light syrup
Be sure to eat enough protein — Inflammation causes increased protein needs. Choose:
- Tender, well-cooked meats: Poultry, salmon or other fish, lean beef and pork prepared without added fat
- Deli meats: Low-sodium and low-fat varieties
- Eggs: Well-cooked
- Tofu
- Smooth nut and seed butters: Peanut, almond or sunflower seed
Drink plenty of fluids — Aim for eight cups a day, and consider using oral rehydration beverages as needed. Try to limit caffeinated, sugar drinks and beverages made with sugar substitutes.
Limit added fats and oils — Focus on oils instead of solid fats, and limit intake to less than eight teaspoons per day.
Consume adequate calcium, vitamin D, probiotics, and prebiotics — Sources include:
The Nutritional Impact Of Uc

Changes in diet and nutrition are one part of a multifaceted approach for treating ulcerative colitis and other IBD conditions. Your doctor also will likely prescribe medication. In more severe cases, surgery may be needed, to repair or remove damaged portions of the colon.
Malnutrition, dehydration, and weight loss are major health risks of UC. When the colon becomes inflamed and ulcerated, its less able to absorb fluids and nutrients needed to help sustain your body.
Diarrhea, a symptom of UC, also increases loss of fluids and nutrients, such as sodium, potassium, magnesium, phosphorus, and zinc.
In severe cases, people with UC may need IV fluids to replace these lost nutrients and fluids.
Other UC symptoms, such as abdominal pain and nausea, can further rob you of nutrition as they reduce your appetite, so you consume fewer calories and nutrients.
Recommended Reading: Herbal Medicine For Ulcerative Colitis
Ulcerative Colitis In Children
Without proper care, pediatric ulcerative colitis will result in slower than normal growth and/or stunted growth.Intestinal inflammation lowers a childs appetite, which mean less food is eaten resulting in fewer nutrients to support healthy growth. Supplements are often a good idea as is making sure that enough calories are consumed, which sometimes requires a high-calorie diet for some kids. Additionally, a therapy or counseling may be sought to help a child develop the tools to cope with their disease.
Scd And Low Fodmap Diet For Ulcerative Colitis
There is a lot of interest but limited clinical evidence for the use of the specific carbohydrate diet and low FODMAP diet for ulcerative colitis.
In one trial, a low FODMAP diet did appear to improve quality of life and symptoms of ulcerative colitis, without improving fecal calprotectin or C-reactive protein, two markers of inflammation. If you are experiencing a lot of IBS-like symptoms, it may be a temporary option to help get symptoms under control.
I have also used low FODMAP foods as a lower fermentation framework for increasing fruit and vegetable intake for those who are currently eating a low fiber diet. I worry about the adoption of a long-term low FODMAP diet in ulcerative colitis as I believe that it might be simply tamping down symptoms by further altering the gut microbiomewhich could be detrimental for long term gut health.
The specific carbohydrate diet is based on a decades-old book called Breaking the Vicious Cycle. To my mind, it is similar to a low FODMAP approach in that it alters the types of carbohydrates available for fermentation in the gut.
It is not uncommon for those who have UC to feel that an SCD diet is helping if that is the case, we will support our client on that chosen path however, I dont believe it is a solution for long term gut health and wont advocate for it in practice. It is a complex diet to follow and isnt supported by the evidence.
Read Also: What To Eat When You Have Ulcers And Acid Reflux
Elemental Diet For Ulcerative Colitis
For nearly 10 years, I have been managing two chronic health issues, ulcerative colitis and hydrogen sulfide SIBO. In an effort to reduce the symptoms, which include severe stomach pain and frequent bathroom visits, among other things, my practitioner suggested we try the Elemental Diet to give my digestive system a break.
I used Physicians Elemental Formula . The goal was to drink at least six scoops per day. At 150 calories each , there was no way in hell I was going to survive. I aimed for 10-12 scoops per day and added MCT oil to each one , so I was getting over 2,000 calories each day. I was also allowed black coffee and salt, so I often mixed decaf with my morning shake. It was actually really tasty! I used a blender bottle/shaker to mix up my drinks.
I also kept a journal for the full eleven days of my diet. I thought it would be a good way to remember everything, so I could easily share with my practitioner. If youre on any type of health protocol, I highly recommend writing down your daily experiences so that you can clearly communicate with your doctor. Sometimes we forget small details that are important for your doctor to know.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Don’t Miss: Ulcer On Eye From Contact Lens
What You Should Know About Strictureplasty
Any surgery is concerning, but learning about the procedure can lessen your concerns and give you information to discuss with your healthcare team.
-
Strictureplasty is a generally safe procedure. It is most effective in the lower sections of the small intestine, called the ileum and the jejunum.
-
Strictureplasty is less effective in the upper section of the small intestine, called the duodenum.
-
Strictureplasty avoids the need to remove a section of your small intestine. It is preferred when possible, because removing portions of your small intestine cause sometimes cause other complications, including a condition called short bowel syndrome which occurs when large sections of the small intestine are removed due to surgery and the body is unable to absorb adequate amounts of nutrients and water.
During the procedure
-
Your surgeon will make cuts lengthwise along the narrowed areas of your intestine, then sew up the intestine crosswise.
-
This type of incision and repair shortens and widens the affected part of your bowel, allowing food to pass through.
-
Your surgeon may repair several strictures during the same surgery.