Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Iatrogenic Complications Adverse Drug Reactions And New Pathologies
Despite the similar use of steroid therapy in the two groups, iatrogenic complications were more common in the elderly . In particular, the most frequent ones were steroid diabetes and osteoporosis .
Unexpectedly, adverse drug reaction were less common in the elderly . . However, if we exclude patients on biological therapy, they were similar in the two groups . Globally, 10 adverse drug reactions developed in the elderly and 16 in the adult group, and the most frequent ones were skin reactions.
Fig. 3
During follow up, some conditions typical of old age were considered. A higher number of elderly patients developed cognitive impairment . Malignancy , deep vein thrombosis/pulmonary embolism , myocardial infarction , stroke and depression were also more frequent .
How Is Inflammatory Bowel Disease Diagnosed
Your doctor will give you a physical exam and listen to you describe your symptoms. To help diagnose the problem your doctor may order a number of tests, including blood tests and stool samples. Your doctor may also order one or more procedures to help them view your colon. Lower GI endoscopy procedures include colonoscopy and flexible sigmoidoscopy. During these procedures, your doctor uses a narrow, flexible tube to look directly inside your large intestine. Upper GI endoscopy allows a look at your stomach and small intestine for ulcers. For this type of endoscopy, you may swallow a small camera . If not, your doctor inserts a scope into your GI tract through your mouth.
Your doctor may also order other imaging tests such as X-rays, a CT scan, or an MRI.
Also Check: Can Ulcers Cause Chest Pain And Shortness Of Breath
What Else Should I Know About Ulcerative Colitis
Poor appetite, diarrhea, and poor digestion of nutrients can make it hard for teens with ulcerative colitis to get the calories and nutrients the body needs. Be sure to eat a variety of foods, get plenty of fluids, and avoid foods that make your symptoms worse. Some teens may need supplements, like calcium or vitamin D. Someone who isn’t growing well may need other nutrition support.
What Is The Outlook
With modern medical and surgical treatment, there is just a slight increase in the risk of death in the first two years after diagnosis, compared with the general population. After this there is little difference in life expectancy from that of the general population. However, a severe flare-up of ulcerative colitis is still a potentially life-threatening illness and needs expert medical attention.
As mentioned, if you do not take medication to prevent flare-ups, about half of people with ulcerative colitis have a relapse on average once a year. This is much reduced by taking regular medication. However, even in those who take regular medication, some people have frequent flare-ups and about a quarter of people with ulcerative colitis eventually have an operation to remove their colon.
A year from diagnosis, about 9 in 10 people with ulcerative colitis are fully capable of work. So, this means that, in the majority of cases, with the help of treatment, the disease is manageable enough to maintain a near-normal life. However, the condition can cause significant employment problems for a minority.
Treatment for ulcerative colitis is an evolving field. Various new medicines are under investigation. These may change the treatment options over the next ten years or so and improve the outlook .
Don’t Miss: How Long Does Prednisolone Take To Work For Ulcerative Colitis
Celiac Later In Life: Can You Become Gluten Intolerant
Research shows that celiac disease can strike at any age, even in people who have tested negative in the past. Whats behind the rise in celiac among seniors?
Jose L. Pelaez/Corbis
Celiac disease can strike at any age, even in people who once tested negative for the condition.
The digestive disease is being diagnosed more frequently in everyone including the elderly, says Joseph Murray, MD, a gastroenterologist at the Mayo Clinic in Rochester, Minnesota, and author of the book Mayo Clinic Going Gluten Free: Essential Guide to Managing Celiac Disease and Other Gluten-Related Conditions.
Celiac disease is an autoimmune condition that tends to run in families. People with celiac cant tolerate gluten, a protein found in wheat, barley, and rye, according to the National Institutes of Health . In these people, gluten damages the part of the small intestine that helps absorb nutrients. Signs and symptoms may include pain, diarrhea, malnutrition, anemia, and osteoporosis, the NIH says. In older people, cognitive impairment can also be a symptom, Dr. Murray says.
The Future Of Celiac Treatment
Clinical trials now under way are looking at different treatments to make gluten less harmful to people with celiac. One drug involves two manmade enzymes that would digest gluten before the body could react to it. Another being developed in Europe, Murray says, would bind gluten in the gut so that the body would get rid of it in a bowel movement. Unfortunately these treatments are years from becoming available and would not be a passport to eating gluten with impunity, he cautions.
Still, there may be a game-changer down the road. Scientists are working on a vaccine that could make a person fully resistant to the effects of gluten. If it works, Murray says, that could be a home run.”
Recommended Reading: Carbohydrate Diet For Ulcerative Colitis
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Homeopathy Medicines For Ulcerative Colitis
The common Homeopathy medicines that our specialists have prescribed for ulcerative colitis at our clinics over the last 18 years are
SILICEA , PHOSPHORUS, COLCHICUM, TEREBENTHINA, MERCURIUS , ARSENIC, ALUMINA , SULPHUR, THUJA, AND NITRIC ACID.
Meet our specialists at any Welling Clinic or consult online to know about your custom-made Homeopathy medicines for ulcerative colitis and get started with your Homeopathy treatment for ulcerative colitis.
Don’t Miss: Diabetic Ulcer On Big Toe
How To Support Someone Living With Ulcerative Colitis
UC is an invisible illness that many still struggle to understand, including the people living with it. Therefore, it may be difficult to know how to support your loved one with UC.
Our first tip? Ask them questions! Thats the best way to learn about their unique experience with ulcerative colitis. Doing your own UC research is also a great step educating yourself helps you grasp the basics of ulcerative colitis and how it can present itself.
At the end of the day, one of the best things you can do is show up. Your presence whether its in person or virtually says, I may not fully understand your experience but I believe you and Im here for you in whatever ways I can be.
Mighty contributor Grady Stewart said it best:
Having an invisible illness can make it exhausting to keep up the façade of feeling well, or to not believe that youre not doing well. Having people in your support squad who understand this alleviates the fatigue of explaining this disconnect between the visible and invisible.
For insight on living with an invisible illness and how to support someone experiencing UC, check out these Mighty stories:
Ulcerative Colitis Vs Crohns Disease
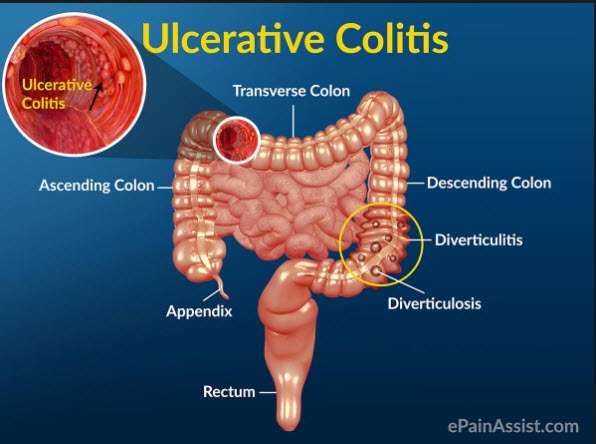
Ulcerative colitis and Crohns disease share similar symptoms and they are both types of inflammatory bowel disease , but they are not the same illness and they affect different areas of the GI tract.
- Can affect any part of the GI tract from the mouth to the anus
- Can affect the entire thickness of the bowel wall
- Only the colon and rectum are affected
- Affects the inner-most lining of the large intestine
- What is Ulcerative Colitis?
Recommended Reading: Pressure Ulcer Prevention Care Plan
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
What Is Crohns Disease

Crohns disease can attack any part of the gastrointestinal system between the mouth and the anus. Crohns is most often found at the end of the small intestine and upper part of the large intestine, or colon. Crohns disease can appear anywhere in the GI tract, in patches between healthy sections of the intestine. Damage and inflammation from Crohns can penetrate deep into all layers of the bowel wall. Disease can recur even if the affected portion of the bowel is surgically removed. There are multiple types of Crohns.
You May Like: Service Dog For Ulcerative Colitis
What Causes Ulcerative Colitis
Ulcerative colitis is thought to be an autoimmune condition.
This means the immune system, the body’s defence against infection, goes wrong and attacks healthy tissue.
The most popular theory is that the immune system mistakes harmless bacteria inside the colon for a threat and attacks the tissues of the colon, causing it to become inflamed.
Exactly what causes the immune system to behave in this way is unclear.
Most experts think it’s a combination of genetic and environmental factors.
Who Develops Ulcerative Colitis
About 2 in 1,000 people in the UK develop ulcerative colitis. It can develop at any age but most commonly first develops between the ages of 10 and 40. About 1 in 7 cases first develop in people over the age of 60 years. Non-smokers are more likely than smokers to develop ulcerative colitis. However, smoking brings other dangers to health which far outweigh this benefit.
You May Like: Best Medicine For Stomach Ulcer Pain
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
What Is Ulcerative Colitis And Who It Affects The Most
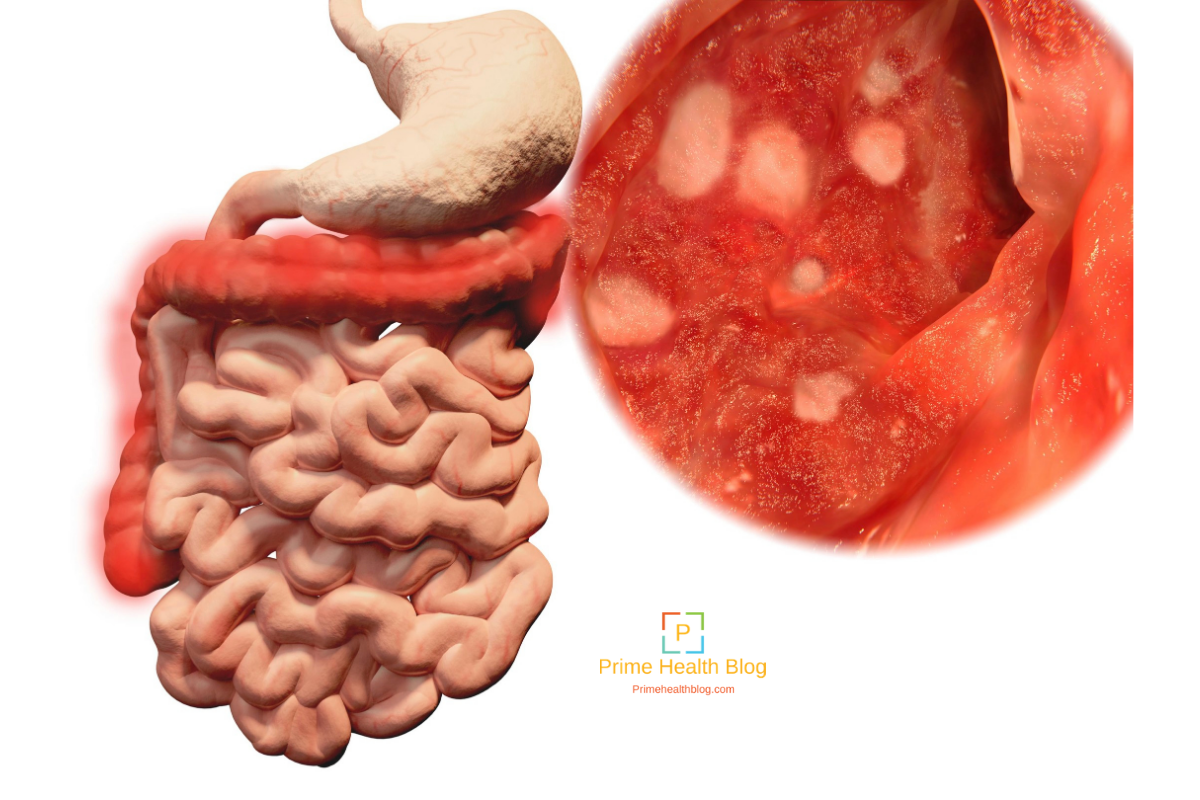
Falling under the category of inflammatory bowel disease, ulcerative colitis is when the lining of your rectum and large intestine become red and swollen, this is also known as inflammation.
In most instances, the inflammation can move to your colon. The inflammation will then cause symptoms such as belly pain and diarrhea. This can lead to an extremely empty colon, which can lead to the death of your colon cells.
Once your colon cells die, youre subjected to open sores also known as ulcers, which can cause pus and bleeding.
You May Also Like
If you have a family history of people living with ulcerative colitis, then you may be at a higher risk of developing this chronic disease.
When diagnosed, most people are usually between ages 15 and 30.
White and Jewish people are known to be diagnosed with this inflammatory bowel disease the most, but that does not mean it cant affect people of other ethnicities and races. It affects all races and ethnicities.
RELATED: 7 Proven Ways To Soothe An Upset Stomach
Read Also: Doctors Specializing In Ulcerative Colitis
Demographic Information And Risk Factors
94 patients who have been diagnosed with UC after the age of 65years were compared with 94 patients who have been diagnosed with UC between 40 and 64years. The demographic characteristics of both group are shown in Table . Median age at diagnosis was 71.5±5years and 50.1±6.7years in E-O and A-O, respectively . Male patients were more frequent in both groups . Family history for UC was similar in the two groups . Difference in smoking habits, althoughs not statistically significant was reported. Time between onset symptoms and UC diagnosis was similar in the two groups, 5.8±4.6months in the elderly and 6.2±4.7months in adults respectively. 34% of the elderly and 19% of the adults received a different diagnosis before UC diagnosis. The most frequent one was diverticular disease in the first group , while infectious colitis was the most common in the second group .
Table 1 Demographic characteristics of UC by age
Median follow among elderly patients up was 8.1years and 5.7years in the control group. Mortality was 20.5% in the elderly and 3.9% in adults. p< 0.0005. Main causes of death were cardiovascular disease , sepsis , extraintestinal neoplasia and respiratory failure in the elderly cardiovascular disease , sepsis and extraintestinal neoplasia in adults.
How Ulcerative Colitis Is Diagnosed
To make a correct diagnosis, your doctor will use several tests to determine what areas of your digestive system are impacted. Doctors can see how much area of the digestive tract is affected through a colonoscopy and an upper endoscopy . Depending on your symptoms, a doctor might order other tests as well, such as imaging studies like radiography or an MRI as well as testing stool samples.
Getting a UC diagnosis can feel scary at first. If youre feeling overwhelmed by a UC diagnosis, Mighty contributor Grady Stewart wants you to know that its OK:
Allow yourself to process your diagnosis. A new diagnosis comes with a range of emotions. Theres no correct or incorrect to respond to such a life-changing event. Feeling sad, angry or anxious are all totally normal reactions to being diagnosed with a chronic condition. Its also acceptable to feel undisturbed, or even relieved by a diagnosis. Recovery and acceptance are a process and not an end goal. Paying attention to your physical and mental health can help you figure out what makes living with ulcerative colitis easier, and what makes it harder. Ultimately, it does get easier.
Read more about life with ulcerative colitis from fellow Mighties here:
You May Like: Indian Diet For Ulcerative Colitis
Little Girl Visited By Gary Neville At Children’s Hospital Ends Up Working For Footy Legend 15 Years Lateryour Browser Indicates If You’ve Visited This Link
A woman who was visited in hospital by Gary Neville 15 years ago has shared the inspirational story of how she now works alongside the football legend. Jenny Byrne, 21, from Stockport, was rushed into hospital at the age of six and was later diagnosed with UlcerativeColitis – an inflammatory bowel disease.
Manchester Evening News on MSN.com
Taking Care Of Yourself
Its natural that living with ulcerative colitis can make you feel stressed at times. Stress can sometimes trigger flare-ups so you may find it helpful to try some relaxation techniques. These may include deep breathing, meditation, yoga and mindfulness.
Regular exercise can also help to give you a boost and make you feel better. It can also improve your general health and help to keep your bones and muscles strong. This is important because some medicines for ulcerative colitis may affect your bone health.
Read Also: Best Way To Heal Stomach Ulcers