Protect The Periwound Skin
Askina® Barrier Cream acts as a protectant and moisture barrier against maceration caused by incontinence or body fluids, to protect sensitive, fragile skin and severely dry skin, including periwound areas. It is indicated for use on intact skin.
Askina® Barrier Film Swab andAskina® Barrier Film Spray are sterile liquid dressings which form a transparent film when applied to the skin. The film possesses good oxygen and moisture permeability. Both dressings are indicated for use on intact or damaged skin.
Negative Pressure Wound Therapy
This is an invaluable tool in the management of pressure sores and involves the application of sub-atmospheric pressure to a wound using a computerised unit to intermittently or continuously convey negative pressure to promote wound healing. NPWT, is effective for deep, cavitating, infected and copiously discharging pressure ulcers, particularly with exposed bone. With growing clinical experience it can be said with certainty that it assists wound healing, and its benefits can be summarised thus:
-
Assists granulation.
-
Applies controlled, localised negative pressure to help uniformly draw wounds closed.
-
Helps remove interstitial fluid allowing tissue decompression.
-
Helps remove infectious materials and quantifies exudates loss.
-
Provides a closed, moist wound healing environment
-
Promotes flap and graft survival.
-
Both hospital and domiciliary use.
-
Reduces hospital/dressings/nursing cost .
Can Pressure Sores Be Prevented Or Avoided
The best way to prevent pressure sores is to avoid spending long periods of time in a chair, wheelchair, or bed. If youre unable to move on your own, make arrangements for somebodysuch as a family member, friend, or caregiverto help you move.
If you must spend a lot of time in a chair, wheelchair, or bed, check your entire body daily. Look for spots, color changes, or other signs of sores. Pay attention to the pressure points where sores are most likely to occur. Again, if youre unable to look on your own, ask someone to help you.
Another way to avoid pressure sores is to keep your skin healthy. This includes keeping it clean and dry. Wash it with mild soap and warm water. Dont use hot water. Apply lotion often.
Even small amounts of exercise can help prevent pressure sores. Thats because exercise improves blood flow, strengthens your muscles, and improves your overall health. Talk to your doctor if physical activity is difficult. They can suggest certain exercises. Your doctor also may refer you to a physical therapist. They can show you how to do exercises that fit with your current health condition.
Lastly, if you smoke, quit. Smoking increases your risk of pressure sores.
Read Also: Does Ulcer Pain Come And Go
Whos At Risk Of Stage 4 Bedsores
Anyone with a lower-stage bedsore is at risk of a stage 4 sore. However, some patients may be more prone to this type of injury.
At particularly high risk are those:
- With Limited MobilityMovement is the key to preventing bedsores of any stage. If an older person cannot move on their own, they may sit or lie in the same position for hours. This can cut off blood flow to their skin and cause a bedsore.
- Who Are In Understaffed Nursing HomesNursing home residents with mobility issues must rely on staff members to prevent bedsores. Sadly, some care facilities may fail to prevent bedsores due to issues like understaffing and poor training.
- Who Have Alzheimers or DementiaIf residents with mental impairments develop a bedsore, they might not be able to tell anyone due to their condition. Theyll need to have someone else find it and help them get the proper care. Residents with these conditions may also have trouble sensing pain.
- Other FactorsResidents are at higher risk of bedsores if they have blood flow or circulation problems, diabetes, or poor nutrition or if they wear a cast.
Our trusted advocates can help you and your loved one take legal action. Call us today at .
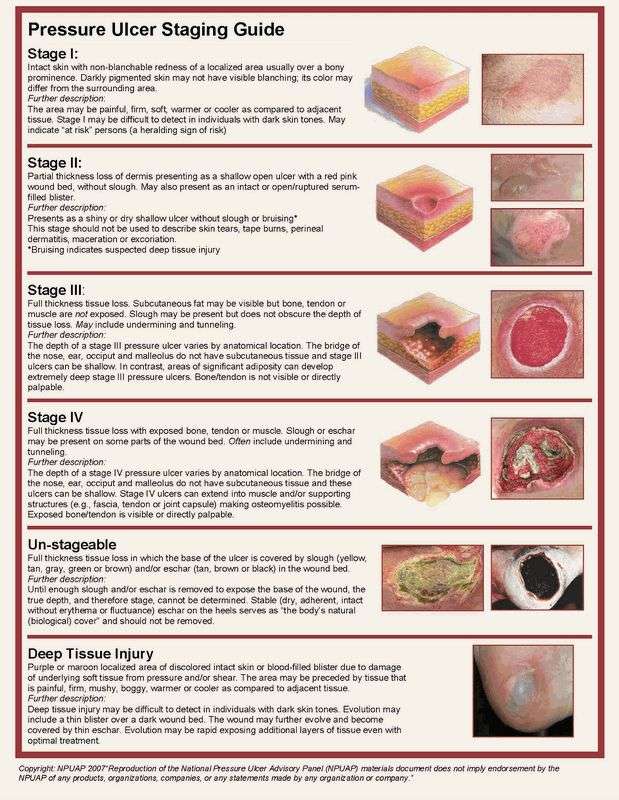
Severity Of Pressure Ulcers
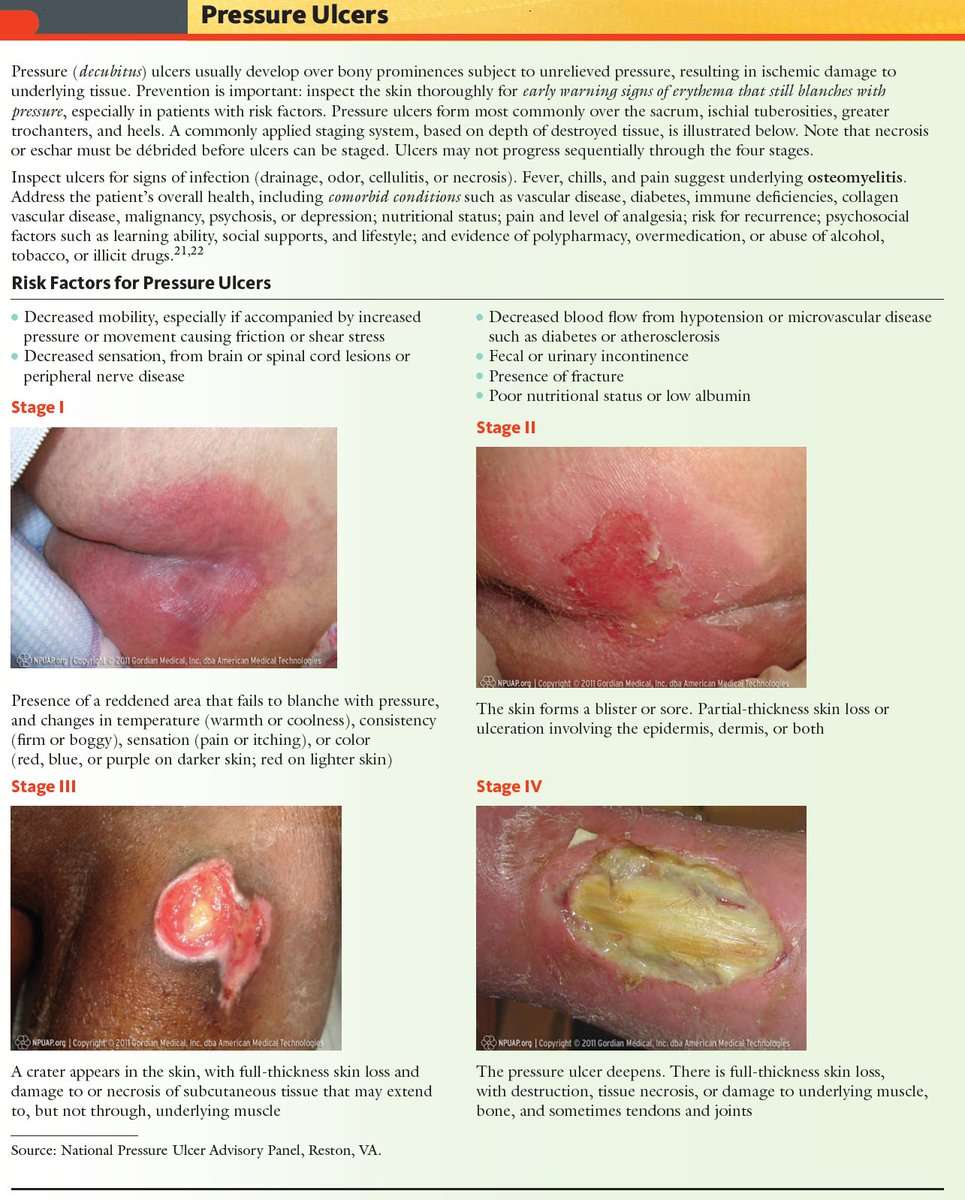
Healthcare professionals use several grading systems to describe the severity of pressure ulcers most common is the EPUAP grading system. Pressure sores are categorised into four stages corresponding to the depth of damage. It must however be emphasised that when an eschar is present, accurate staging is not possible.
You May Like: Diet For People With Stomach Ulcers
Complications From Stage 4 Bedsores
Those with a stage 4 bedsore are at high risk of life-threatening complications.
If left untreated, a stage 4 bedsore may lead to:
- AmyloidosisThis is an incurable condition where protein builds up in the body and prevents organs from functioning properly.
- InfectionThose with a stage 4 bedsore are at a very high risk of infections, according to Johns Hopkins Medicine. These infections can affect the skin, bones, blood, and other organs.
- Renal FailureThis occurs when the kidneys can no longer remove waste from the body, causing damage. It can be fatal if left untreated, but recovery may be possible.
- Sepsis may occur when the body overreacts to a serious infection, such as an infection stemming from a stage 4 bedsore. The immune system gets overstimulated and attacks healthy body parts. Severe cases of sepsis can lead to septic shock, which occurs when blood pressure drops due to an infection. Septic shock can be deadly as major organs may shut down.
- DeathMany of the conditions listed above can be fatal if left untreated. According to an article in the Western Journal of Medicine, renal failure and amyloidosis are the most common causes of death for patients suffering from chronic bedsores.
It may be considered a if a nursing home patient dies from an untreated bedsore.
When To Get Medical Advice
If you’re in hospital or a care home, tell your healthcare team as soon as possible if you develop symptoms of a pressure ulcer. It’ll probably continue to get worse if nothing is done about it.
You should be regularly monitored and offered advice and treatment to reduce the risk of pressure ulcers, but sometimes they can develop even with the highest standards of care.
If you’re recovering from illness or surgery at home, or you’re caring for someone confined to bed or a wheelchair, contact your GP surgery if you think you or the person you’re caring for might have a pressure ulcer.
Get medical advice immediately if there is:
- red, swollen skin
- pus coming from the pressure ulcer or wound
- cold skin and a fast heartbeat
- severe or worsening pain
- a high temperature
These symptoms could be a sign of a serious infection that needs to be treated as soon as possible.
Don’t Miss: Ulcerative Colitis When To Go To Er
Who’s Most At Risk Of Getting Pressure Ulcers
Anyone can get a pressure ulcer, but the following things can make them more likely to form:
- being over 70 older people are more likely to have mobility problems and skin that’s more easily damaged through dehydration and other factors
- being confined to bed with illness or after surgery
- inability to move some or all of the body
- medical conditions that affect blood supply, make skin more fragile or cause movement problems such as diabetes, peripheral arterial disease, kidney failure, heart failure, multiple sclerosis and Parkinson’s disease
What Are The Risks Of This Treatment
Problems can happen during any surgery, even with the best treatment. Your surgeon will talk with you to explain what problems might happen. It is up to you to decide whether the benefits of the surgery outweigh the possible risk for problems. Here are a few examples of the more potential serious problems you will talk about with your doctor:
- The wound comes back
- The wound either does not close properly or breaks open along the row of stitches holding the flap edges together
- Harmful bacteria get into the body through an opening in the skin and leads to an infection
- The skin and tissue used for the flap dies
- Bleeding occurs under the flap that may need emergency treatment to drain
You May Like: What Not To Eat With Bleeding Ulcers
What Are Pressure Ulcers
Skin is the largest organ system in the body. The skin is tough and durable to protect the subcutaneous tissue against air, water, foreign matter, and bacteria. Our skin is sensitive to injury and this organ has special healing abilities. However, even with elasticity, skin cannot withstand the excessive pressure, stretching or scrubbing. Continuous pressure on the skin tightens the blood vessels, which are responsible for providing nutrients and oxygen to the skin. When the skin is too long anemic, tissue will die, causing the formation of pressure ulcers. Also known as bedsores or decubitus ulcers, pressure ulcers are a common skin condition people have to cope with.
More specifically, it is one of the major complications of a person with paralysis. For example, according to experts’ estimates, about one third of patients with spinal cord injury will have pressure ulcers in the early days after injury, and about 50-80% of the remaining patients may develop this problem later. Most types of ulcers can be prevented but they may even occur in patients who are well cared for and are supported by appropriate equipment .
To heal these ulcers, the patient needs a lot of time, money and good care. Patients may have to lie down for up to a month because of a pressure ulcer, especially an ulcer due to surgery. All these conditions can cost you thousands of dollars and cause you to lose valuable time for work, school or family.
Did You Know That
Pressure ulcers can occur quickly – between the first hour and 4 to 6 hours after sustained loading.
A. Gefen
One to four of every ten hospitalized patients develop pressure ulcers.
Range varies among settings and classification method.
In areas affected by COVID-19 lockdown only 22,6% of patients with chronic wounds went to the wound clinics as usual, and 1 in 10 did not change the wound dressing at all during that whole period.
Tinelli, G. et al.
Read Also: Can You Take Imodium If You Have Ulcerative Colitis
Review Question: What Are The Most Reliable Techniques/tools To Measure The Dimensions Of A Pressure Ulcer
One systematic review looked at the performance of instruments designed for measuring the dimensions of pressure ulcers. This systematic review was included in the current evidence review and it was subsequently updated to include 1 other study . Overall 13 studies were included in the evidence review.,,,,,,,,,,,, Evidence from these is summarised in the clinical GRADE evidence profile below. The quality of these studies is outlined in .
The OMeara review looked at studies of any design which reported an evaluation of a pressure ulcer measurement instrument as the main focus of the investigation. The authors did not include assessment checklists where the focus was the performance of the tool overall rather than the measurement of pressure ulcer dimensions.
Recommended Reading: Are Eggs Bad For Ulcerative Colitis
What Are The Long
If the wound becomes infected, the infection can spread to other parts of the body. Several conditions that may occur if an infection spreads include:
- Cellulitis: An infection of the skin.
- Osteomyelitis: An infection of the bone.
- Bacteremia: An infection of the blood.
- Meningitis: An infection of the brain and spinal cord.
- Endocarditis: An infection of the heart.
Read Also: Pressure Ulcer Prevention Care Plan
Analysis Of Existing Evidence
The effect of pressure ulcers on patients, nurses, and hospitals is outlined in academic literature. Qaseem et al. find that the prevention of bedsores is much more beneficial than their treatment. First of all, pressure ulcers are dangerous to the health of patients as it is described above. Skin damage and the following infections increase morbidity and mortality, putting patients at increased risk of complications and prolonged length of stay at the hospital .
Second, clinicians also encounter challenges in dealing with bedsores as the latter require adequate assessment and difficult treatment. Prevention, on the other hand, can be performed in steps that have been tested and documented. Finally, the rate of ulcers affects hospitals and units as it is one of the factors of healthcare organizations ratings. The high incidence of bedsores implies the poor quality of service, low rating of the unit, and decreased financial support.
In order to adequately address the issue, it is necessary to understand how pressure ulcers can be measured. According to Fletcher and Hall , nurses may face many challenges due to hospitals having different records of patients with pressure ulcers. Some of the wounds may be called bedsores, while others may have names such as moisture-associated dermatitis or sacral and gluteal lesions .
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
-
the Cochrane Wounds Specialised Register
-
the Cochrane Central Register of Controlled Trials
-
Ovid MEDILINE
Searching other resources
Recommended Reading: Best Vitamins For Ulcerative Colitis
Diagnosing A Stage 4 Bedsore
A doctor determines the by its appearance. In the case of a stage 4 bedsore, the large wound has passed the bodys fatty tissue layer, exposing muscles, ligaments, or even bone.
In some cases, however, health care professionals may not be able to immediately diagnose a late-stage bedsore by examining it.
A stage 4 bedsore may be initially diagnosed as:
- UnstageableWhen a doctor cannot see the bottom of an open sore, they must clean it out to properly stage it.
- Suspected Deep Tissue Injury This diagnosis happens when the surface of a patients skin looks like a stage 1 or 2 sore, but it is actually affecting deeper tissues underneath.
These Are The Signs Of Stage Four Ulcer Development
In hospitals and healthcare institutions worldwide, the topic of pressure injuries comes up frequently when discussing patient care and risk management. This makes sense. Pressure injuries have the potential to cause significant problems for both patients and healthcare professionals. In the United States, 2.5 million people experience pressure injuries each year, and 60,000 of those die annually. These particular injuries, also known as hospital acquired pressure injuries , can develop in hospital beds or in operating rooms. In fact, up to 45% originate on operating tables. When left untreated, pressure sores can result in severe tissue damage and even death. These statistics offer a stark reminder that comprehensive treatment for pressure injuries is vital. And beyond thatprevention methods should be integrated at the beginning of patient care.
Over the last year, weve watched and learned as hospitals have undergone serious strain due to COVID-19. With staffing efforts redirected to address the virus, inefficiencies in routine patient care have become more obviousparticularly care that tends to be manual and labour-intensive, such as monitoring for pressure injuries. In a world grappling with this global pandemic, we have a responsibility to help alleviate pressure on our valued healthcare workers by integrating smart, sustainable technology that prevents injuries efficiently, with far less work required.
What are the stages of a pressure sore?
Also Check: Does Smoking Cause Ulcers After Gastric Bypass
How Can I Tell If I Have A Pressure Sore
- First signs. One of the first signs of a possible skin sore is a reddened, discolored or darkened area . It may feel hard and warm to the touch.
- A pressure sore has begun if you remove pressure from the reddened area for 10 to 30 minutes and the skin color does not return to normal after that time. Stay off the area and follow instructions under Stage 1, below. Find and correct the cause immediately.
- Test your skin with the blanching test: Press on the red, pink or darkened area with your finger. The area should go white remove the pressure and the area should return to red, pink or darkened color within a few seconds, indicating good blood flow. If the area stays white, then blood flow has been impaired and damage has begun.
- Dark skin may not have visible blanching even when healthy, so it is important to look for other signs of damage like color changes or hardness compared to surrounding areas.
- Warning: What you see at the skins surface is often the smallest part of the sore, and this can fool you into thinking you only have a little problem. But skin damage from pressure doesn’t start at the skin surface. Pressure usually results from the blood vessels being squeezed between the skin surface and bone, so the muscles and the tissues under the skin near the bone suffer the greatest damage. Every pressure sore seen on the skin, no matter how small, should be regarded as serious because of the probable damage below the skin surface.
How To Assess Wounds For Tunneling And Undermining
As part of a thorough wound assessment, in addition to noting location and measuring size, the entire wound bed should be probed for the presence of tunneling and/or undermining. If you are unsure what tunneling and undermining are and how to recognize these phenomena, heres an explanation of these terms and how to assess wounds for their presence.
Read Also: What To Avoid Eating With Ulcerative Colitis
Information Sources And Searches
Guidelines, systematic reviews, reports, online documents, and books were searched as long as they met the inclusion criteria. A combined search of the Embase and Medline databases was conducted via OVID . Available systematic reviews22, 23 were used to search for the original publications. In addition, numerous databases and websites were searched, including: