Why Is It Important
Almost half of IBD patients have at least one flare a year.
This can have a huge impact on their physical and emotional wellbeing. For the NHS, the major impact is financial as its 2-3 times more expensive to treat a patient with active disease compared to someone in remission.
When someone has a flare, the GP is often their first port of call. But 52% of GPs say they are less than confident or not confident if an IBD patient comes to their clinic with a flare-up1.
This is why flare pathways are so important. Co-produced by a working group of health professionals and patients as part of the RCGP and Crohns & Colitis UKIBD Spotlight Project, and approved by the British Society of Gastroenterology, they give primary care health professionals accessible guidance on steroid intervention, dose escalation, and when to refer to secondary care.
With these pathways, suitable patients can be managed appropriately. This means better and more confidence in responding to flares effectively, including rapid access to advice from the IBD team.
Understand That Flares Happen
UC flare prevention didnt work? That happens, says Rudolph A. Bedford, M.D., a gastroenterologist at Providence Saint Johns Health Center in Santa Monica, CA. Sometimes, quite frankly, youre going to flare no matter what we do, and no matter whats happening, he points out. UC is an autoimmune disease, meaning the bodys immune system is attacking the large intestine. We dont know all the reasons why this happens, so sometimes flares can surprise us at any time, for seemingly no cause. Making peace with this can be helpful, as well as being proactive about seeking treatment to relieve symptoms.
Talk To Your Doctor Asap
Heres the thingUC treatment for mild disease is typically oral medication and for moderate to severe disease, often biologics. But medications can stop working for many reasons, says Andrew Boxer, M.D., a gastroenterologist at Jersey City Medical Center – RWJBarnabas Health Medical Group, Jersey City, NJ. Or you might have an infection. Both scenarios can cause a UC flare. So its key that you tell your doctor as soon as you experience symptoms, he says. If a flare is caught early, treatment may help stop the flare, Dr. Boxer explains.
Recommended Reading: Foam Boots For Pressure Ulcers
Are Your Ulcerative Colitis Symptoms Under Control
She emphasizes that your doctor will likely be just as focused on ensuring your treatment also leads to endoscopic remission and histologic/deep remission .
Studies show that those who are in endoscopic and deep remission do best long term, as far as lower chances of hospitalizations for flare-ups and lower chances of complications, including surgery, she says.
Still, your doctor will also recommend that when you do feel your digestion is off that you recognize it and react as quickly as possible.
Pay extra attention if you are exposed to any potential ulcerative colitis triggers. For example, some common medications may prompt flares. The two biggest culprits are antibiotics and nonsteroidal anti-inflammatory drugs , such as ibuprofen, aspirin, and naproxen. Other triggers may include stress and foods that aggravated your symptoms in the past.
Make Time For Activities That Make You Happy
Tip number three to help you prevent an ulcerative colitis flare-up: Always make time for things that make you happy. For me, its dancing. I have been taking dance classes since my pre-school years and continues to do so to this day. Its wonderful exercise, I have met amazing friends through this hobby, and it is also my favourite form of exercise. When I am in the dance studio, I forget about everything else in the world and focus on being in the present. So, whether it be dance, a sport that you love, or something as beautiful as painting, make time to feed your hobbies with your time and hopefully you will feel more fulfilled and less stressed!
Also Check: Ulcerative Colitis Surgery Pros And Cons
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you haven’t been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If you’ve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you can’t contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
Read Also: Ulcerative Colitis And Lung Disease
Managing Ulcerative Colitis Flares: The Most Important Step
The key to managing an ulcerative colitis flare is to get a confirmed diagnosis and begin treatment as soon as possible. But doing so can be tricky, because people with the condition may attribute their symptoms to other GI problems, says Oriana Mazorra Damas, MD, an assistant professor of gastroenterology at the University of Miami Miller School of Medicine in Miami.
The goal for remission is to feel well enough that you forget that you have the condition for most of the day in other words, you experience few, if any, symptoms, Dr. Damas explains.
What Is A Uc Flare
A UC flare is an acute worsening of the symptoms of bowel inflammation. Flares may occur weeks, months, or even years apart, with different levels of severity.
Medication, your lifestyle, diet, and other factors may contribute to flare-ups. In the same way, taking all prescribed medications, eating balanced meals, and avoiding known triggers can often help prevent flares.
Ulcerative colitis symptoms change based on the severity of a flare-up and the location of inflammation in the intestine. Symptoms often include:
- moderate to severe abdominal pain or cramps
- persistent bowel movements
You May Like: Wound Vac For Pressure Ulcers
Easing Symptoms During A Flare
The below suggestions can also help ease symptoms or help keep your body healthy during a flare-up.
Drink water: In UC, the large intestine can have a hard time absorbing water and salt, which can contribute to diarrhea and dehydration. Drinking plenty of water or an electrolyte replacement drink can help avoid dehydration if you’re experiencing a flare.
Eat plain, easy-to-digest foods: During a UC flare, it’s common to lose your appetite. To keep your energy levels up and avoid malnutrition and weight loss, it’s important to continue to fuel your body with food. Unfortunately, fruits and vegetables, particularly when raw, are bothersome for many people with UC. Avoid fatty and greasy foods as well. Your doctor may also suggest meal replacement drinks if you’re losing weight from UC flare-ups.
Get some exercise: If you’re experiencing symptoms like stomach pain and diarrhea, exercise may sound like the last thing you want to do. But in addition to the well-known mood and health-boosting benefits of exercise, a workout can also have specific benefits for UC symptoms. Uncontrolled inflammation in the intestinal tract leads to UC symptoms. Exercise has an anti-inflammatory effect that can help these symptoms.
Foods To Eat During An Ulcerative Colitis Flare
Avoiding certain foods is only half the battle. Heres how to get the nutrients you need during an ulcerative colitis flare.
Jeff Wasserman/Stocksy
If you have ulcerative colitis, you may already know which foods worsen your flares. But figuring out what to include in your diet is equally important, because the right foods will provide you with key nutrients without aggravating your symptoms.
Most experts recommend that you limit your fiber intake when youre having an ulcerative colitis flare. A general rule is to replace high-fiber foods, such as nuts, seeds, and raw fruits and vegetables, with more easily digestible fare. Here are eight foods to eat during an ulcerative colitis flare and the reasons they can help.
1. Applesauce: Since your gastrointestinalsystem is experiencing a lot of irritation during a flare, you may want to stick to soft, easily digestible foods like applesauce. Be sure to choose an unsweetened variety though, because added sugar can cause more inflammation. You can also make your own sugar-free applesauce by cooking peeled, sliced apples with some water and then pureeing the mixture.
3. Cooked vegetables: Soft, cooked veggies like carrots and spinach can provide important nutrients, such as vitamins A and K. Just make sure the vegetablesare thoroughly cooked until they can be mashed with a fork, Szeles says so that any potentially irritating fiber is broken down.
Additional reporting by Nina Wasserman
Also Check: What Are The Symptoms Of An Ulcer In Your Stomach
When To Call Your Doctor About A Flare
Flares come with different levels of intensity. You may be able to manage a mild flare-up of symptoms on your own. But a more severe flare may be a warning sign of an ulcerative colitis complication that needs immediate attention.
Theodore J. Saclarides, MD, a colon and rectal surgeon at Rush University Medical Group in Chicago, suggests calling your doctor if you have any of these ulcerative colitis symptoms:
- Severe abdominal pain that lasts more than 24 hours
- A decrease in bowel movements along with abdominal pain
- Abdominal pain with a high fever
- Blood during a bowel movement that is too thick to see through
Ulcerative Colitis Flare Symptoms
Flare-ups indicate that the disease is in an active state, which means the rectum and colon are becoming more inflamed or sores are worsening or spreading. Symptoms of flare-ups include:
- Experiencing frequent or urgent bowel movements
- Diarrhea, which may include blood or pus
- Stool thats bloody
- Vomiting
- Weight loss
The pattern of UC flare-ups is unpredictable. The disease is considered active when symptoms are present, and in remission when no symptoms are present. Some people may spend years in remission, while others may have more frequent flare-ups.
Also Check: How To Heal Mouth Ulcers Fast
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Ulcerative Colitis Questions To Ask Your Doctor
Whether youre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
Also Check: How To Cure Gastritis And Ulcers Naturally
Make Sure Youre Getting Enough Probiotics And Prebiotics
Whether you take probiotics tablets, eat fermented vegetables or other fermented products, or take kefir, I personally try to intake something with probiotics and prebiotics at least a few times a week. My personal favourite is a kefir smoothie its an excellent combination of probiotics and prebiotics! Learn more about how to choose the right probiotics here.
How To Reduce Flare
While flare-ups often dont have a single, identifiable cause, several factors may contribute to them or make them worse, including:
- Missing your UC medications or taking the wrong dose
- Taking non-steroidal anti-inflammatory drugs or antibiotics
- Smoking
- Stress
- Certain foods
If flares occur even when a patient takes their medications as prescribed, it may be a sign that a change in medication type, dosage or frequency is needed.
Read Also: L Glutamine Ulcerative Colitis Dosage
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
Ways To Manage Symptoms And Flares Of Ulcerative Colitis
A flare of ulcerative colitis can be painful and embarrassing not only for you, but for those around you. Once you have one flare, are you going to have more? That anxiety can make you feel even worse and trigger one. Lets investigate 6 ways to manage symptoms and flares of ulcerative colitis.
Also Check: What Foods Should I Avoid With A Stomach Ulcer
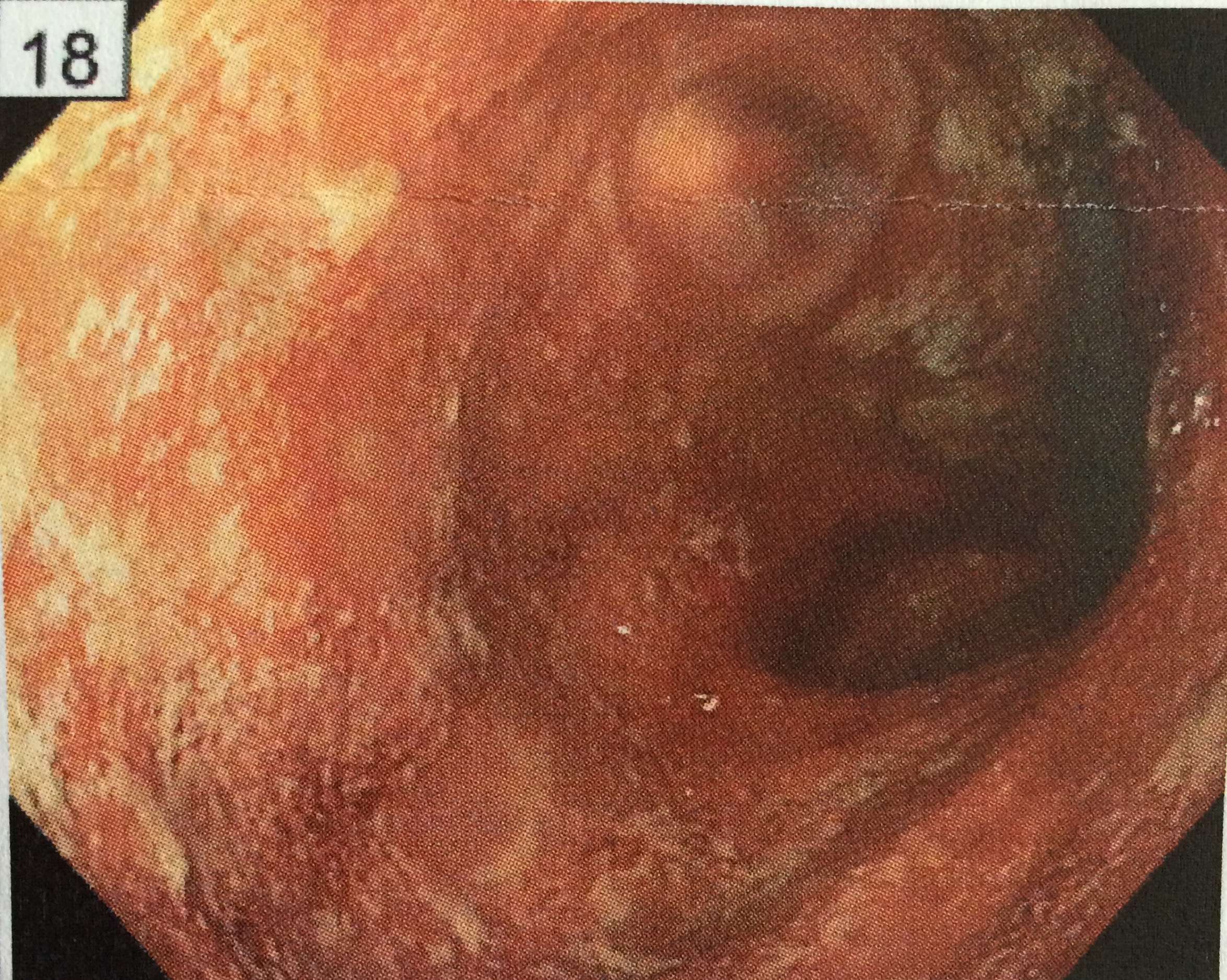
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Continue To Eat And Drink

If your symptoms are severe, you may not feel like eating or drinking. However, this increases the risk of becoming dehydrated. Instead, try to follow a healthy diet, but avoid high-fiber foods for a few weeks. These include bread and cereal made with whole grains, fresh and dried fruit, raw vegetables, seeds and nuts. Eating smaller meals may also help. Also avoid drinking carbonated drinks, which can worsen your symptoms. Instead, drink small amounts of water throughout the day to stay hydrated.
Read Also: Different Types Of Ulcerative Colitis
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Know When To Call Your Doctor
If youve been diagnosed with ulcerative colitis, its important to talk with your doctor about which symptoms require medical attention. These include fever, intense abdominal pain and a feeling of extreme fatigue. If youre having these symptoms, call your doctor.
Its important to know your body so you can recognize the early signs of flare-ups. Talk to your doctor about steps you can take to reduce your symptoms and make sure youre not taking any medication that your doctor doesnt know about. You may not be able to avoid flare-ups completely, but you may be able to lengthen the amount of time between episodes and make flare-ups less intense.
1 Available at http://www.ccfa.org/assets/pdfs/flares_brochure_final.pdf. .
Also Check: What Are The First Signs Of A Stomach Ulcer
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.