Ulcerative Colitis Can Take A Toll On Your Mental Health Too
Being told you have a chronic illness can feel like someone has just rerouted the course of your whole life. I went through my own acceptance process, Skomski says. I definitely went through a period of questioning if my life would ever be normal. With time, processing the reality of having ulcerative colitis became easier. I had to learn there’s nothing wrong with me it’s just part of who I am, Skomski says. You have to do a lot of mental work to flip the way you perceive it because otherwise it can really eat away at you.
Dealing with the symptoms can also be mentally and emotionally taxing. The psychological side of the pain is a lot worse than the actual physical sensation, Sam says. It’s when you feel like it’s never going to end, or you’re going to be stuck in that high level of pain for a long period of time, or that no one gets how hard it is to deal with it. This has led to constant vigilance about her health. It’s very hard for me to not be closely monitoring my body 24/7, Sam says. The catch-22 is that stress is definitely a trigger for me.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
How Common Is Cramping Among Those Who Have Uc
Inflammatory bowel disease, which includes both UC and Crohns, affects about 1.6 million Americans of all ages, according to the Crohns and Colitis Foundation. More than half of those with UC experience abdominal pain.
The frequency and persistence of cramping can help determine the severity of UC, according to Faten N. Aberra, MD, MSCE, co-director of the Inflammatory Bowel Disease Center at the Joint Penn-CHOP Center and an associate professor of medicine at the Hospital of the University of Pennsylvania, in Philadelphia. Pain that comes and goes with bowel movements may indicate a moderate level of UC. Constant cramping and frequent, bloody stools, on the other hand, may indicate a more serious condition, says Dr. Aberra, such as a dilated colon.
Also Check: What To Do When Ulcerative Colitis Flares
How To Calm An Ulcerative Colitis Flare
This article was co-authored by Peter Gardner, MD. Peter W. Gardner, MD is a board certified physician who has practiced Gastroenterology and Hepatology for over 30 years. He specializes in diseases of the digestive system and liver. Dr. Gardner earned his Bachelors degree from the University of North Carolina and attended Georgetown Medical School. He completed his residency in Internal Medicine and then his fellowship in Gastroenterology at the University of Connecticut. He is a previous Chief of Gastroenterology at Stamford Hospital and remains on the staff. He is also on the staff of Greenwich Hospital and New York Presbyterian Hospital. Dr. Gardner is an Approved Consultant in Internal Medicine and Gastroenterology with the American Board of Internal Medicine.There are 8 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 9,951 times.
What Can I Do About Pain When I Have Ibd
Being in pain can significantly affect your quality of life, especially if it is difficult to control or lasts for a long time. Make sure you tell your IBD team about any pain you are experiencing so they can work with you to find out what is causing it.
If it is a result of your disease activity, you might be asked to increase the dose of the medicine you are taking, or change to a different treatment. In many cases, this can reduce inflammation and symptoms, and so be effective in reducing pain.
However, if you are still struggling with pain and discomfort despite changing your treatment to manage your disease better, or if it is caused by something else, you may need to consider other ways to manage your pain.
There are a range of pain management options that dont involve medicines that you could explore, such as:
These can be particularly useful to help you feel in control of managing your pain, especially if it is causing anxiety, low mood and behaviour changes .
However, it is quite likely at some stage you may require medicine to help you with pain resulting from your Crohns disease or ulcerative colitis, even if just for a short period of time.
Don’t Miss: Different Types Of Ulcerative Colitis
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Be Consistent With Treatment Drugs
Take your medications consistently. Dont miss or skip a dose even when in remission. Dont try to wean yourself off of a treatment drug as these changes can all lead to flares.
Contact Digestive Health Services at if you have any changes to your flares, or if you think you might have ulcerative colitis.
Tags:
Also Check: How To Heal Mouth Ulcers Fast
Spend More Time In Delta Sleep
Sleep keeps my colitis in remission. When I travel, get jet lag, or even stay out past midnight, I know Im setting myself up for a painful flare up. So I always say that one of the best ways to keep ulcerative colitis or any inflammatory bowel disease in remission is to sleep, sleep, SLEEP. I get eight hours a night, and often take a 30 minute nap during the day. I also try to get at least three hours of sleep before midnight. Ive found that getting eight hours of sleep after midnight doesnt make me feel as rested as sleeping before midnight does.
Sleep can keep the symptoms of ulcerative colitis in remission for so many reasons, both physical and emotional. Sleep helps restore brain and cell energy, recharges our minds and bodies, increases protein buildup, helps maintain social and emotional functioning, helps encode memories, improves learning ability, and helps process memories.
If you have trouble sleeping, read Natural Sleep Remedies for Sleepless Nights.
Tylenol And Heat Therapy
Doctors frequently prescribe nonsteroidal anti-inflammatory drugs such as ibuprofen or aspirin to help manage back pain. However, NSAIDs arent typically a viable solution for people with UC, as the medication can cause symptoms to flare.
Those with ulcerative colitis can generally take the pain reliever Tylenol which is not an NSAID for minor aches and pains without side effects. Applying moist heat to affected areas may also reduce pain.
Also Check: Surgical Management Of Ulcerative Colitis Ppt
What To Do During An Ulcerative Colitis Flare To Minimize Symptoms
Youll inevitably experience another UC flare-up at some point, despite your best prevention efforts. When this happens, there are a few ways youll need to tweak your normal routine to minimize the severity of your symptoms and get back into remission ASAP. Even some of your typically healthy habits like loading up on veggies may be a no-go. Here are a few natural remedies that may help:
Use Prescription Medication For Painful Flare Ups
I rely on natural remedies to prevent my symptoms of ulcerative colitis from flaring, and I use prescription medication to ease the painful symptoms when my colitis actually flares. Ive learned how to recognize when my guts are gearing up to explode, and I try to head it off at the pass. How do I know when the colitis is about to flare? The very bottom of my rectum starts to feel swollen and slightly uncomfortable. I can literally feel it starting to swell! So I use an enema before bed Id rather prevent a flare than spend time trying to ease the pain of my ulcerative colitis symptoms.
Pentasa enemas work best for me. Ive tried all sorts of suppositories, oral medications, and enemas to ease the painful symptoms of ulcerative colitis. A liquid enema is my best friend before and during a flare up. Enemas are more effective than suppositories because the liquid soaks into the bowel quickly and easily. I used suppositories for eight years after I was diagnosed with colitis, until a new gastroenterologist recommended enemas instead.
While I wish my first way to keep my ulcerative colitis in remission wasnt with prescription medication, I havent found anything else that works as good as the drugs. It doesnt matter what I eat I can eat popcorn, nuts, caffeine, dairy but when my colitis wants to flare, the only thing that tamps it down is an enema.
Recommended Reading: Best Way To Treat Mouth Ulcers
Pineapple Juice For Ulcerative Colitis Relief
One of the main protagonists of these home remedies to control ulcerative colitis is pineapple juice. The bromelain in pineapples is great to treat digestive diseases, since it has anti-inflammatory properties. In fact, by drinking two classes of pineapple juice every day , youll feel relief from your symptoms.
What Causes Rectal Bleeding
In general, hemorrhoids and diverticular disease are the most common causes of rectal bleeding.2,5 Other common causes include:
- Angiodysplasia of the colon
- Colon inflammation from many causes
- Polyps
- Stomach ulcers
- Colorectal cancer
Bleeding in the lower digestive tract has been linked to taking non-steroidal anti-inflammatory drugs , such as Aleve, Advil, and Motrin.4 Once you have been diagnosed with IBD, NSAIDs are not recommended.6
However, research about the link between NSAIDs and IBD is ongoing and so far, inconclusive. No studies have shown that taking these medications is a cause of IBD.7
Recommended Reading: What Are The Symptoms Of An Ulcer In Your Stomach
What Pain Relief Medicines Are Used In Inflammatory Bowel Disease
There are a variety of pain relief medicines available which can help to control pain in Crohns disease and ulcerative colitis.
Paracetamol
Paracetamol is a commonly used over-the-counter painkiller you can buy without a prescription. It can be used to help with mild to moderate pain, and can also help to control a high temperature. Paracetamol can be used by adults and children and is available in a variety of forms, including:
- Tablets, capsules and caplets
- Soluble tablets
- Oral suspension
- Suppositories
Paracetamol works by blocking the production of chemicals in your body called prostaglandins, making your body less aware of any pain. It also reduces your temperature by acting on the part of your brain responsible for controlling it.
Paracetamol is often combined with other medicines, including other types of painkillers. Always check any additional medicines are also safe for you to use.
It is generally considered safe to take paracetamol if you have inflammatory bowel disease, however if you need to take paracetamol for longer than three days, or have a new pain, you should speak to your IBD team.
Two paracetamol tablets every four hours, up to four times a day is considered a safe dose for adults. Side effects are uncommon with paracetamol.
You should read the patient information leaflet in your medicine packet to check if paracetamol is suitable for you. Do not take more than the maximum dose in a 24 hour period as an overdose of paracetamol can be very dangerous.
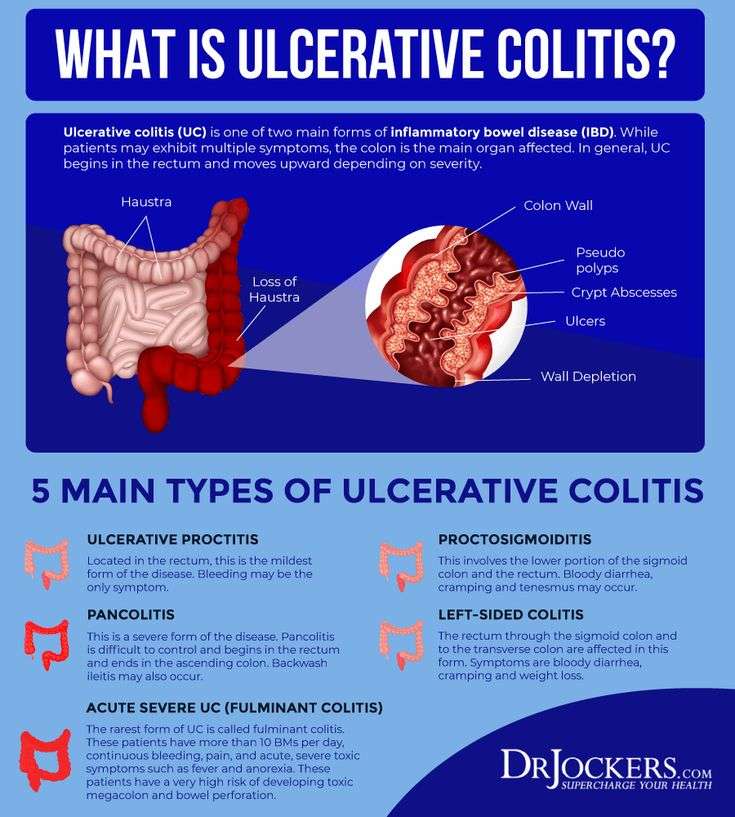
Ulcerative Colitis Causes And Risk Factors
Ulcerative colitis happens when your immune system makes a mistake. Normally, it attacks invaders in your body, like the common cold. But when you have UC, your immune system thinks food, good gut bacteria, and the cells that line your colon are the intruders. White blood cells that usually protect you attack the lining of your colon instead. They cause the inflammation and ulcers.
ishonestNo.361 – Acne Scars
Doctors arent sure why people get the condition. Your genes may play a role the disease sometimes runs in families. Other things in the world around you may make a difference, too.
Things that can affect your risk of getting ulcerative colitis include:
- Age. Its most likely if youre between 15 and 30 years old or older than 60.
- Ethnicity. The risk is highest in people of Ashkenazi Jewish descent.
- Family history. Your risk could be up to 30% higher if you have a close relative with the condition.
Food and stress dont cause it, but they can trigger a flare of symptoms.
Also Check: Can You Drink Coffee With Ulcerative Colitis
Could My Symptoms Be Ibs
Irritable Bowel Syndrome is a different condition from IBD, although some of the symptoms are similar. Like Crohn’s and Colitis, IBS can cause abdominal pain, bloating and bouts of diarrhoea or constipation. However, it does not cause the type of inflammation typical of Colitis, and there is no blood loss with IBS.
Some people with Colitis may develop IBS-like symptoms, for example experiencing diarrhoea even when their Colitis is inactive. These symptoms may need slightly different treatment from their usual IBD symptoms. IBS is more common in people with IBD than in the general population.
If you develop diarrhoea with bleeding and abdominal pain, your doctor may suspect you have Colitis, particularly if you are a young adult or have a family history of Crohn’s or Colitis. You will need tests and physical examinations to confirm a diagnosis. See Tests and Investigations for IBD.
You may need to have tests repeated from time to time to check on your condition and how your treatment is working.
Some drug treatments may also require a series of blood tests and, occasionally, x-rays or scans to check for any potential side effects. Your specialist will avoid giving you any unnecessary tests or investigations.
You may need more regular colonoscopies when you have had Ulcerative Colitis for a long time to check for any signs of cancer.
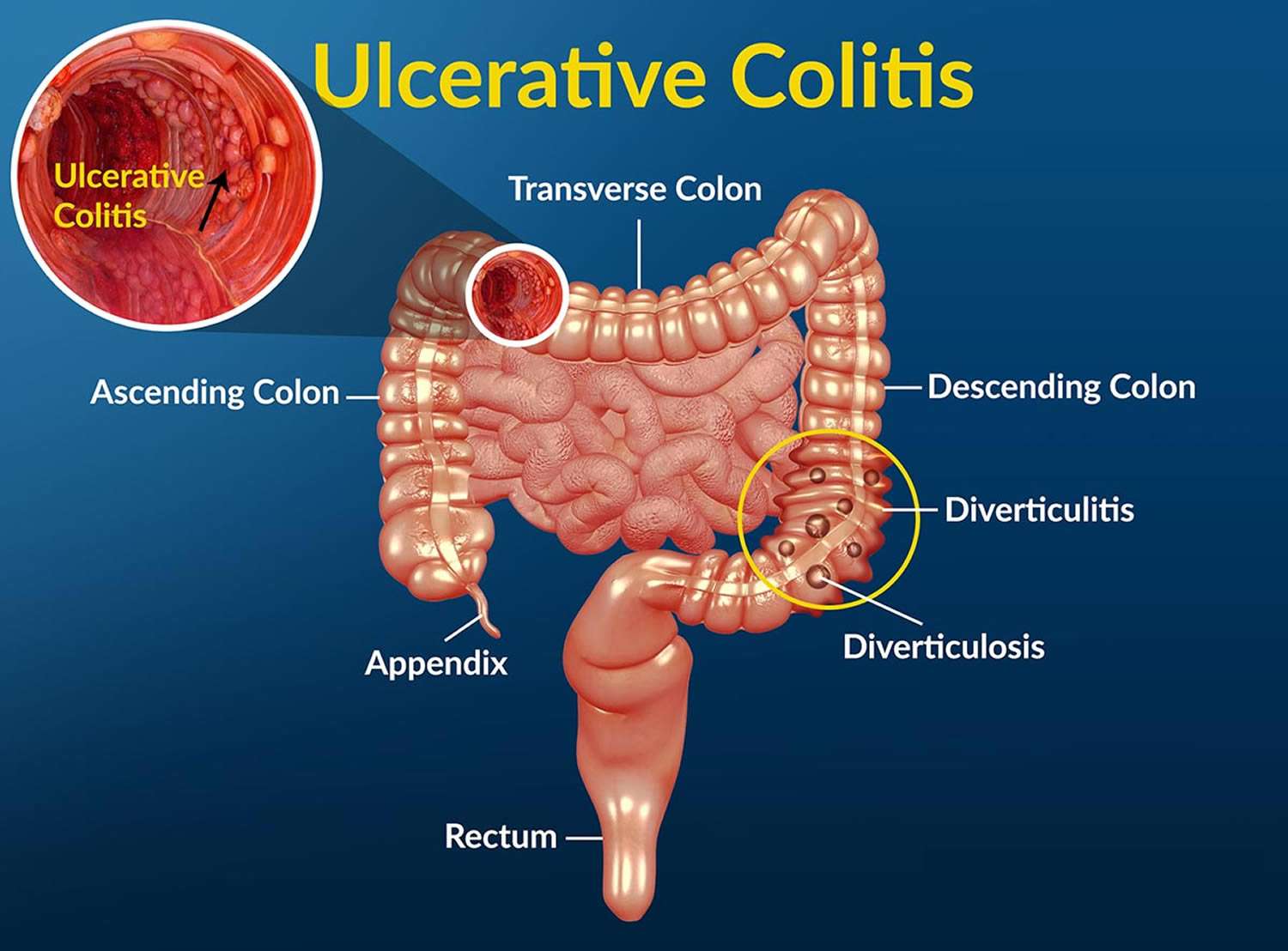
Signs Of Possible Colitis
General signs of colitis can include:
- Intense pain
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.
Recommended Reading: Side Effects Of Ulcerative Colitis
Why Working With A Qualified Care Team Is So Important When It Comes To Managing Ulcerative Colitis
People being treated for UC typically arent getting dietary or lifestyle advice, which is a huge disservice, says Cohen. But managing ulcerative colitis and preventing flare-ups can be done! You just might need a little help from the experts.
Because UC isnt one-size-fits-all and triggers are highly individual, enlisting the help of a care team like the clinicians at Parsley Health is wise. Providers can provide individualized supplement protocols based on lab testing, customized eating plans for periods of remission and flares, and communicate with your current GI doctor if necessary to streamline care.
Rice Water To Fight Ulcerative Colitis
One cup of rice water as soon as you wake up and another before bed will help control ulcerative colitis and its symptoms.
Ingredients
- 1 cup of rice
- 3 cups of water
Preparation
Preparing this drink is very simple.
You May Like: Foam Boots For Pressure Ulcers
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I can’t bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I can’t fully stand upright sometimes for a minute or so. It’s frustrating.