Treatment Of Kidney Infection
Most kidney infections need prompt treatment with antibiotics to stop the infection damaging the kidneys or spreading to the bloodstream.
You may also need painkillers.
If youre especially vulnerable to the effects of an infection , you may be admitted to hospital and treated with antibiotics through a drip.
Most people who are diagnosed and treated promptly with antibiotics feel completely better after about 2 weeks.
People who are older or have underlying conditions may take longer to recover.
Surgical Approach: Laparoscopic Versus Open
Multiple randomized controlled trials have shown that laparoscopic colectomy is as good as the open approach in CRC in regard to the oncological results . The same has also been shown for rectal cancer . Therefore, also in UC, CRC can be operated by minimally invasive means without oncological disadvantage for the patient, provided the learning curve of laparoscopy has been overcome. Whether the typical short-term advantages as demonstrated for other laparoscopic colorectal procedures also hold true for restorative proctocolectomy remains controversial. Feasibility and safety of the laparoscopic approach have been shown in various studies nevertheless, clear evidence for the superiority of the laparoscopic compared to the conventional IPAA is not available. In 2009, a Cochrane review of 11 trials failed to demonstrate a difference between laparoscopic and open IPAA with regard to morbidity and mortality. However, some of the studies confirmed the most obvious advantage, i.e. a significantly improved cosmesis, if the patient had undergone laparoscopic surgery .
Fig. 4
Second postoperative day after laparoscopic restorative proctocolectomy .
People With Ulcerative Colitis Need To Be Screened For Colorectal Cancer More Thoroughly And More Often
The ACS recommends that people at average risk of developing colorectal cancer start getting regular screenings at age 45. Depending on the specific type of screening, regular might mean every year , or even every 10 years . A colonoscopy is the best tool to detect early cancer because we can directly look at the colon and find a suspicious lesion, Dr. Wang says.
People with IBD, on the other hand, are generally advised to get colonoscopy screenings every one to two years starting at an earlier age than 45, but the exact guidelines depend on the specifics of your case.
We need to individualize thescreening based on the course and extent of the patients colitis, Dr. Oberstein says, as well as any additional risk factors. For instance, people with a family history of colorectal cancer may need yearly screening, while people in remission who have clear screenings for several years may be able to space them out more, Dr. Wang says, adding that its key to have an ongoing discussion with your doctor about the right timeline for you.
To compensate for that, doctors often use special techniques that are more sensitive than the standard colonoscopy when examining someone with ulcerative colitis, Dr. Oberstein says. The most common is a chromoendoscopy, which uses dye to help identify subtle lesions in the colon lining better than just using light, Dr. Wang says. Another technique is biopsying, or taking tiny tissue samples to look for cancer in them.
Related:
You May Like: What Causes Mouth Ulcers On Gums
Symptoms Of Pagets Disease Of The Bone:
People who have Pagets disease of bone typically have no symptoms. When symptoms do occur, the most common complaint is bone pain.
Because this disease causes your body to generate new bone faster than normal, the rapid remodeling produces bone thats softer and weaker than normal bone, which can lead to bone pain, deformities and fractures.
The disease might affect only one or two areas of your body or might be widespread. Enlarged and misshapen bones can put extra stress on nearby joints, which may cause further pain and complications. Symptoms, depend on the affected part of your body.
- Pelvis. Pagets disease of bone in the pelvis can cause hip pain.
- Skull. An overgrowth of bone in the skull can cause hearing loss or headaches.
- Spine. When the spine is affected nerve roots can become compressed. This can cause pain, tingling and numbness in an arm or leg.
- Leg. As the bones weaken, they may bend causing you to become bowlegged.
Occult Colorectal Cancer In Ulcerative Colitis
Occult cancer is defined as a clinically inapparent malignancy which is incidentally discovered while the patient is examined for other reasons . The setting in which occult CRC is most likely detected in UC patients is surveillance colonoscopy with random biopsies. CRCs diagnosed during surveillance endoscopy have also been termed as interval CRCs . High-grade dysplasia confirmed by a reference pathologist or CRC diagnosed in an asymptomatic patient are absolute indications for elective oncologic resection.
Also Check: Ulcerative Colitis Surgery Pros And Cons
Why Does Kidney Disease Cause Weight Gain
Kidney disease doesnt just affect the kidneys, it affects the whole body. In the early stages, it can cause weight loss, while in the later stages it can cause weight gain. These variations are the result of different aspects of the disease. Heres some information to help you understand the issue of kidney disease and weight gain, courtesy of Dr. Allen Lauer, of Associates in Nephrology.
You May Like: What To Do For A Kidney Infection
The Risk Of Colorectal Cancer In Crohns Disease And Ulcerative Colitis Patients
Patients with ulcerative colitis and Crohns disease involving the colon need to be especially vigilant about screenings for colorectal cancer. These patients are at higher risk for developing colorectal cancer than the general population.
Inflammation of the colon can cause continuous turnover of cells in the intestinal lining, which increases the chance of irregularities that may lead to cancer. Though the vast majority of patients with Crohns disease and ulcerative colitis will never develop colorectal cancer, it is important to discuss the risk with your doctor. Colorectal cancer is a highly treatable disease when its found early.
Also Check: How To Check A Horse For Ulcers
Prostate Cancer And Radiation Colitis
Although technological advancements have made radiation therapy treatment more specific to the prostate, surrounding structures such as the bladder and rectum can still be affected.1 Close to 70% of all cancers are treated with radiation depending on the location of the involved organ, radiation colitis can be a common complication outside of prostate cancer.2 Yet up to 20% of patients with prostate cancer treated with RT will develop radiation colitis.3
Radiation colitis can present in 2 ways: acute and chronic .1-4 Patients with acute and chronic radiation colitis have similar symptoms, although chronic can cause more gastrointestinal bleeding. A patients bowel movements will contain more mucus and will be less formed they may experience diarrhea as well as urgency. Tenesmus is another common symptom.
Chronic inflammation of the rectum over many years can lead to stricturing of the left side of the colon, which may present with changes in stool caliber or constipation.
Getting Screened For Cancer
Because your risk for colorectal cancer increases over time if you have UC, its important to receive regular screenings for colorectal cancer.
People with UC should talk to their doctors about getting a colonoscopy, the main test used to detect this cancer.
Getting regular colonoscopies can help lower your risk for developing colorectal cancer or dying from colorectal cancer.
For people with IBDs who underwent regular screenings, the odds of developing colorectal cancer dropped by 42 percent. The odds of dying from the cancer dropped by 64 percent.
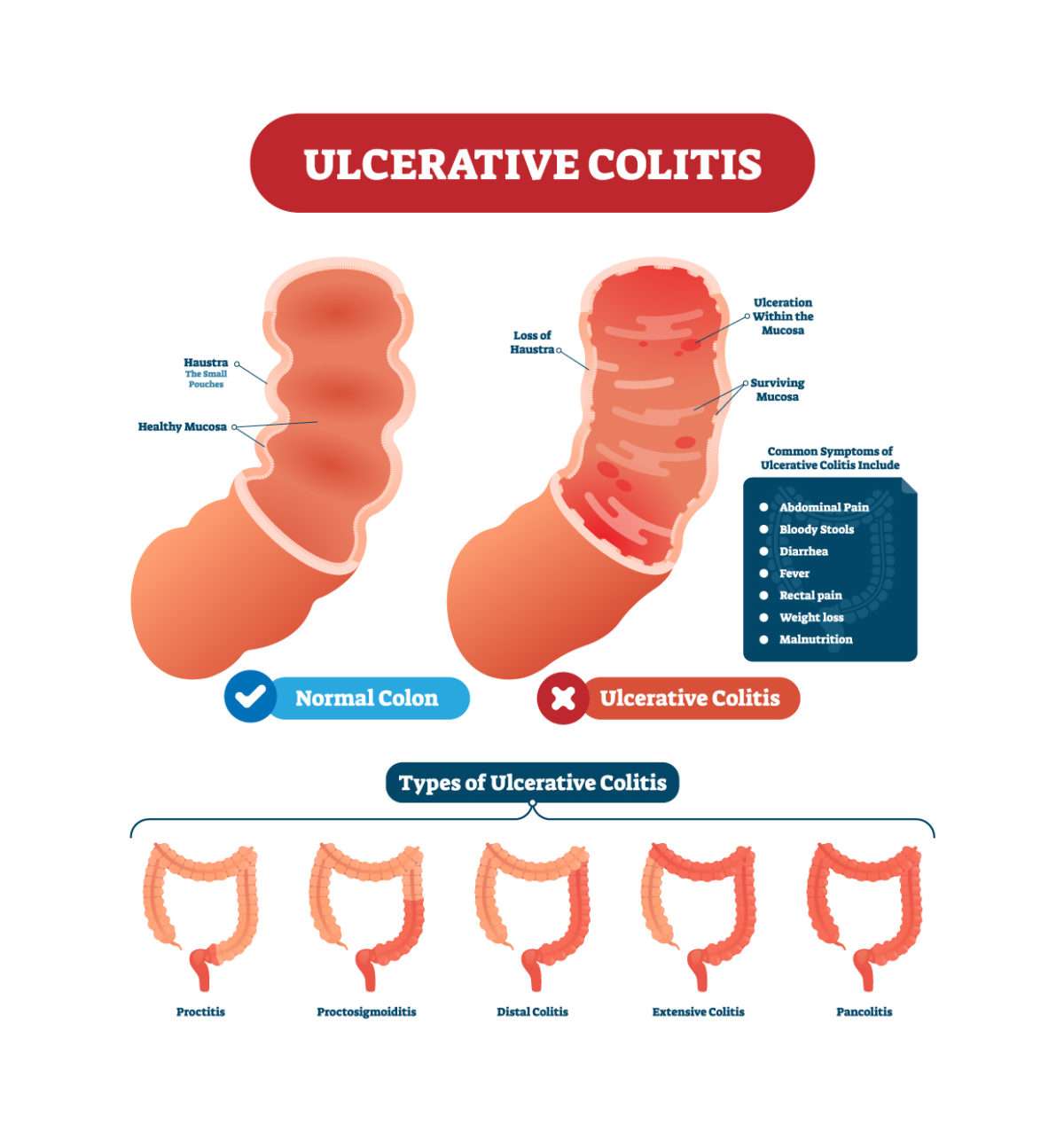
Also Check: Different Types Of Ulcerative Colitis
If You Have Dysplasia Consider Having Your Colon Removed
Patients with high-grade dysplasia may need to have a colectomy, a surgical procedure to remove some or all of the colon.
However, if the dysplasia is low-grade, the bumps and nodules can often be completely taken out during a colonoscopy.
Doctors may also choose to monitor low-grade dysplasia with more frequent colonoscopies to see if the inflammation regresses with treatment, says Dr. Ehrlich.
How A Colonoscopy Works
In a colonoscopy, a doctor uses a long, flexible tube with a camera at the end to see inside your colon. The test helps them detect polyps in your colon lining. The doctor can remove these growths to prevent them from turning into cancer.
Your doctor might also remove tissue samples during your colonoscopy and have them tested for cancer. This procedure is called a biopsy.
Recommended Reading: Wound Vac For Pressure Ulcers
How Can We Decrease The Risk Of Crc In Ibd
The positive association between UC and CRC raises several practical questions. The causes behind the changing trends in UC-related CRC epidemiology are complex. One key element may be the early diagnosis and treatment of precancerous lesions by colonoscopic surveillance or sometimes prophylactic colectomy, while the third option is primary chemoprevention. Nowadays, prophylactic colectomy is obsolete. Nonetheless, the high colectomy rate, especially in Scandinavian countries has been associated with lower CRC risks. There are however, obvious changes in the patient management, also in Scandinavia. In the new population-based cohorts, a decrease in the colectomy rate can be observed.
Identification Of Primary Studies
All published reports citing the risk of CRC in UC were collected by conducting a literature search on Medline using the following keywords: colorectal cancer, ulcerative colitis, surveillance studies, dysplasia, risk factors, and children. A comprehensive search of reference lists of all review articles and of the retrieved original studies was performed to find studies not identified by the Medline search. This identified 194 independent studies dating back to 1925.
You May Like: L Glutamine Ulcerative Colitis Dosage
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Inflammatory Bowel Disease May Increase Ckd Risk
Inflammatory bowel diseases , such as ulcerative colitis and Crohns disease, or their treatments may increase the risk for chronic kidney disease , according to new research published in Clinical Gastroenterology and Hepatology.
Ravy K.Vajravelu, MD, MSCE, of the University of Pennsylvania in Philadelphia, andcolleagues conducted a retrospective study comparing 17,807 IBD patients fromthe United Kingdom with 63,466 matched control patients. Stage 3 or higher CKD,assessed by repeat measurements of estimated glomerular filtration rate ordiagnosis code, developed in 5.1% of IBD vs 3.5% of control patients, with age-standardizedincidence rates of 130.3 vs 91.3 per 100,000 person-years. The risk of CKD inpatients with IBD diminished with age, from a 7.9-fold increased risk of CKD byage 16 years to a 1.13-fold increased risk at age 77 years. The risk was onlyslightly lower for ulcerative colitis compared with patients who had Crohns disease.Active flare did not appear to influence eGFR.
Previous studies havelinked common non-biologic IBD therapies with impaired renal function. In thisstudy, neither 5-aminosalicylate nor methotrexate was associated with reducedeGFR. Azathioprine was associated with a slightly higher eGFR . Biologic medications, such as infliximab, adalimumab, andvedolizumab, are not usually prescribed by general practitioners in the UK, butthese medications have not been associated with CKD among IBD patients in priorstudies, according to the authors.
Recommended Reading: What Foods Should I Avoid With A Stomach Ulcer
When To See A Doctor
People with UC should regularly check in with their doctor to discuss any changes in their condition, as well as any new changes in available treatments.
It is also important to have regular scans, as they may help detect early signs of damage that could be precancerous. Catching colorectal cancer early is crucial to effectively treating it.
Also, people who feel that their current treatment plan is not helping with their UC symptoms should see a doctor.
Unchecked damage from UC is a risk factor for colorectal cancer, so having an effective treatment plan is vital.
Technical Aspects Of Surgery In Crc In Uc
Patients with CRC in the colon require lymphadenectomy, which includes division of the ileocolic vessels at their origin. This reduces the options for lengthening the mesentery and may result in a slightly reduced chance of successful pouch formation, especially when performing a hand-sewn pouch-anal anastomosis. In experienced centers, however, this is very rarely a problem. In very obese patients, where obtaining length can be difficult in such a scenario, an S-pouch is an option.
Fig. 2
Preserved ileocolic vessels in restorative proctocolectomy , allowing more lengthening options.
There is still controversy on what type of anastomosis should be done in patients with CRC in UC: stapler anastomosis with a short rectal cuff or hand-sewn IPAA .
Fig. 3
a Stapler anastomosis in IPAA with short rectal cuff and b hand-sewn anastomosis in IPAA without cuff .
In case of rectal cancer total mesorectal excision has to be performed as radically as in sporadic rectal cancer. In case of cancer or dysplasia solely in the colon without detection of neoplastic lesions in the rectum on random biopsies, however, it seems reasonable to be a little less radical in order to better preserve the pelvic nerves and sexual function.
Read Also: Can I Eat Oatmeal With Ulcerative Colitis
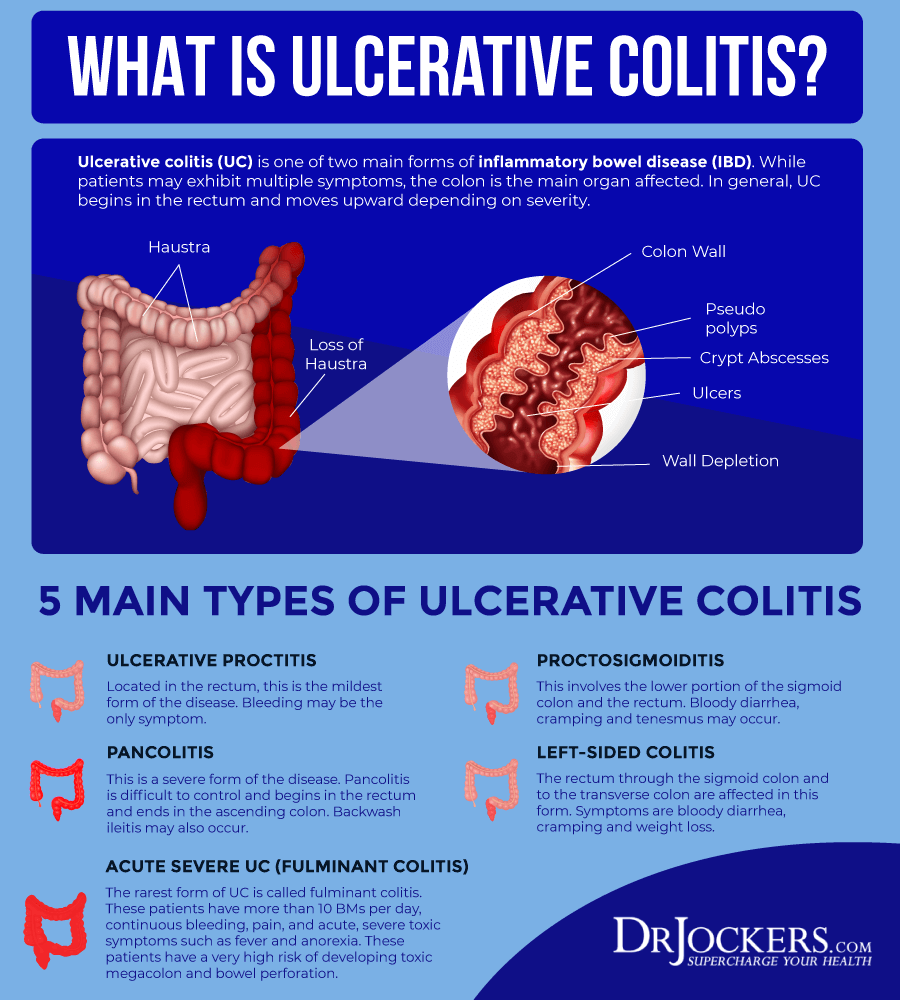
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
How To Reduce Your Colon Cancer Risk
With a chronic condition like UC, you should have regular checkups with your doctor to be sure that youre staying on top of controlling the disease, and to catch any warning signs of more serious complications, such as cancer. There are also other ways to reduce your risk, including:
Reducing your cancer risk when you have ulcerative colitis is all about minimizing inflammation. Talk to your doctor about the best way to manage the condition, says Chang.
Ask whether medications are working or if you should try something different, get your cholesterol tested, and pay attention to your diet. Our aim is to try to prevent problems before they start.
Also Check: Ulcerative Colitis And Lung Disease
Diagnosis Of Pagets Disease Of The Bone:
The cause of Pagets disease of bone is unknown. Scientists suspect a combination of environmental and genetic factors contribute to the disease. Several genes appear to be linked to getting the disease.
In addition to a physical exam, X-rays, and blood tests can help confirm the diagnosis of Pagets disease of bone. X-rays and bone scan may reveal changes in the bones. While, those with Pagets disease of bone usually have elevated levels of alkaline phosphatase in their blood, which can be discovered by a blood test.
Read Also: Which Side Is Your Kidney On
Q: Does Having Inflammatory Bowel Disease Affect My Risk For Developing Colon Cancer
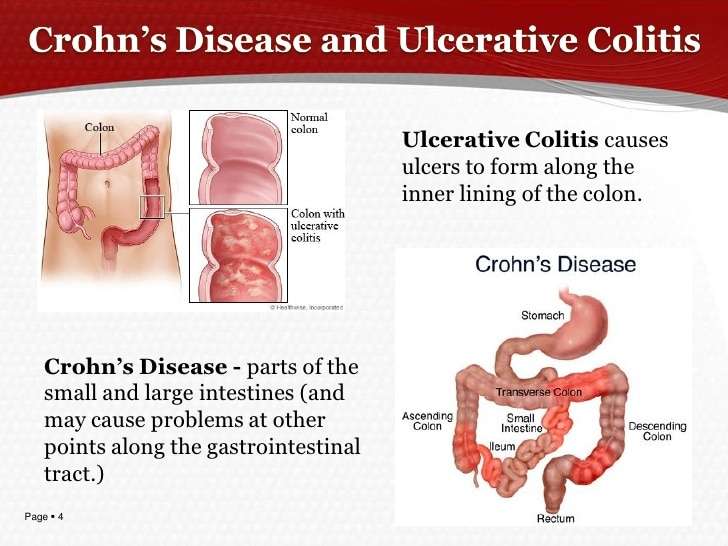
A: Yes. If you go back 20 years, the thinking was that just ulcerative colitis was associated with increased risk of colon cancer. But weve found more recently that inflammatory bowel disease does have a higher risk than the general population.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.Policy
There are two things we think about here when it comes to risk. The first one is the length of time that someone has had IBD. The second is the degree to which the bowel is affected. So patients that have had it longer and have more of their colon affected are at a higher risk and thats for both patients with Crohns and ulcerative colitis.
In people without inflammatory bowel disease, the pathway to cancer is pretty clear-cut, where you get a polyp, the polyp becomes dysplastic, and then ultimately you get cancer. But the IBD pathway can be different. So not only is it important that we control these patients inflammation, but also that we follow up with them at more frequent intervals to make sure they dont have cancer.
Also Check: How Long Does An Ulcerative Colitis Flare Up Last
What Are The Signs And Symptoms Of Colon Cancer Vs Ulcerative Colitis
Colon Cancer Symptoms and Signs
Some individuals with colon cancer have no symptoms, and if they do have symptoms they often are minimalized and overlooked until the cancer becomes more severe. Cancer screening tests for colon cancer thus are important in individuals 50 years of age and older. Colon and rectum cancer can have many different symptoms and signs. If you have any of these symptoms, seek immediate medical help. You may notice bleeding from your rectum or blood mixed with your stool. It usually, but not always, can be detected through a fecal occult blood test, in which samples of stool are submitted to a lab for detection of blood.
People commonly attribute all rectal bleeding to hemorrhoids, thus preventing early diagnosis owing to lack of concern over “bleeding hemorrhoids.” New onset of bright red blood in the stool always deserves an evaluation. Blood in the stool may be less evident, and is sometimes invisible, or causes a black or tarry stool.
Rectal bleeding due to colon cancer may not be noticeable or chronic, and may only show up as an iron deficiency anemia, not colon cancer. Colon cancer may be associated with fatigue and pale skin due to the anemia. Changes in bowel movement frequency also is a symptom of colon cancer.
If the tumor in the colon becomes large enough, it may completely or partially block your colon. Symptoms of bowel obstruction include:
Ulcerative Colitis Symptoms and Signs
Common symptoms of ulcerative colitis include: