Risk Factors Of Ulcerative Colitis
- Age: While this disease can occur at any age, ulcerative colitis usually begins before the age of 30.
- Race or ethnicity: Although whites have the highest risk of the disease, it can occur in any race.
- Family history: Youre at a higher risk if you have a close relative, such as a parent, sibling or child with the disease.
- Isotretinoin use: Isotretinoin, formerly sold under the brand name Accutane, is a medication sometimes used to treat scarring cystic acne or acne that does not respond to other treatments. While there have been some connections between isotretinoin and ulcerative colitis, the reports are conflicting as to whether isotretinoin actually causes ulcerative colitis.
What Causes Stomach Ulcers
Your stomach normally produces acid to help with the digestion of food and to kill germs . This acid is corrosive, so some cells on the inside lining of the stomach and the first part of the gut known as the duodenum produce a natural mucous barrier. This protects the lining of the stomach and duodenum.
There is normally a balance between the amount of acid that you make and the mucous defence barrier. An ulcer may develop if there is an alteration in this balance, allowing the acid to damage the lining of the stomach or duodenum. Causes of this include the following:
Dont Miss: Can I Donate Blood If I Have Ulcerative Colitis
Treatment By Disease Severity And Location
Mild-moderate distal colitis
- Oral aminosalicylates, topical mesalamine, or topical steroids
- Combination of oral and topical aminosalicylates is better than either alone
For refractory cases, oral steroids or IV infliximab can be used
Mild-moderate extensive colitis
- Oral sulfasalazine 4-6 g/day or alternative aminosalicylate 4.8 g/day
- Oral steroids for patients refractory to above therapy + topical therapy
- 6-MP or azathioprine for patients refractory to oral steroids, but not so severe as to require IV therapy
- Infliximab in patients who are steroid refractory/dependent on adequate doses of 6-MP/thiopurine or who are intolerant to these medications
Severe colitis
- Infliximab if urgent hospitalization is not needed
- If a patient is toxic, should be admitted to the hospital for IV steroids
- Failure to improve in 3-5 days is indication for colectomy or IV cyclosporine
Indications for Surgery
- Absolute: Hemorrhage, perforation, documented or strongly suspected cancer
Also, surgery is recommended for severe colitis refractory to medical therapy
You May Like: How To Treat Oral Ulcers
What Research Is Being Done Regarding Ulcerative Colitis
Active research is also ongoing to find other biological agents that are potentially more effective with fewer side effects in treating ulcerative colitis including adalimumab, visilizumab, and alpha-4 integrin blockers.
Research in ulcerative colitis is very active, and many questions remain to be answered. The cause, mechanism of inflammation, and optimal treatments have yet to be defined. Researchers have recently identified genetic differences among patients which may allow them to select certain subgroups of patients with ulcerative colitis who may respond differently to medications. Newer and safer medications are being developed. Improvements in surgical procedures to make them safer and more effective continue to emerge.
Health Maintenance
It is recommended that adults with inflammatory bowel disease generally follow the same vaccination schedules as the general population.
Osteoporosis has also increasingly been recognized as a significant health problem in patients with IBD. IBD patients tend to have markedly reduced bone mineral densities. Screening with a bone density study is recommended in:
- postmenopausal woman,
How You May Feel
Ulcerative colitis attacks the lining of your digestive tract. It causes swelling and sores in the lining.
If youâve just been diagnosed with it, hereâs what might happen during a flare-up:
You might have some of those symptoms, but not all. And they may change over time. They can range from very mild to very bad.
Read Also: I Think I Have Ulcerative Colitis
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Symptoms Beyond The Intestine
When ulcerative colitis is raging, it can take its toll on more than just the GI tract.
The inflammation from ulcerative colitis can make patients feel very fatigued lead to blood loss, causing anemia and cause weight loss due to difficulty absorbing nutrients, says Dr. Ather.
Symptoms beyond the intestine affect mental health and quality of sleep, too. A study published in 2018 in the International Journal of Behavioral Medicine found higher rates of mental health and sleep disorders in people with ulcerative colitis.
It is important for us to screen for these issues and refer our patients to get the help they need, Dr. Ather says.
You May Like: How Do You Get Ulcerative Colitis
A Feeling Of Wooziness
On occasion, the person may experience a little more run down when engaging in exercises or exerting extra hard work. Perhaps the person feels an unusual feeling of wooziness especially when stands hurriedly after a long sit.
All these may be accompanied by a sense of fatigue which is often blamed on too much work performed by the person. The individual will be remarkably in distress, thinking it may be due to different sort of situations.
Only when the person visits a doctor for help will he be able to point clues about the problem. Stomach ulcer may be identified and can be drawn based on history of heartburns, diet, activities, and excessive intake of drugs which may be possibly taken by the person to help reduce aches of the body when feeling fatigue.
Taking Care Of Your Hair
For some people, simple dermatologist-recommended practices to increase scalp and follicle health may do the trick. These practices include:
- Limiting the use of heated styling tools, such as curling irons and hair straighteners
- Blow-drying infrequently or on low heat
- Avoiding chemical treatments, such as coloring and relaxing
- Using gentle or naturally derived hair products
- Avoiding hairstyles that tug on the hair follicles, such as tight ponytails
- Being gentle when combing or styling your hair
Recommended Reading: Holistic Treatment For Ulcerative Colitis
What Tests Diagnose A Peptic Ulcer
To confirm a person has an ulcer a diagnostic imaging test will usually be ordered. The two most widely used tests are:
- Upper GI series : This is a type of X-ray. The patient is given a chalky liquid to drink that increases the contrast on the X-ray, making certain features easier to see. Because this liquid contains barium, this test is sometimes called a barium swallow.
- Endoscopy : An endoscope is a thin, flexible tube with a tiny camera at the end. The patient is given a mild sedative, and then the tube is passed through the mouth into the stomach. The doctor can see the lining of the stomach to diagnose a peptic ulcer. Tiny samples of the tissue will be taken , which are examined under a microscope.
If a diagnostic imaging test reveals an ulcer, the patient will most likely have a test to see if H pylori bacteria are present.
- It is important to be certain about this, because treatment of the H pylori is likely to heal the ulcer.
- Ulcers caused by H pylori are treated differently than ulcers caused by medications.
Three types of tests are available to detect H pylori.
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
You May Like: Diabetic Foot Ulcer Early Signs
Rectal Bleeding Every Other Day
Hi, I would just like to start of with saying I have severe health anxiety so this constant bleeding for several months is driving me mad. Ive always had a little blood here and there since I was very young and never thought anything of it but now its every other day and Im so scared. I have been to the doctors and they have referred me for sigmoidoscopy but now I dont know when thats going to be happening cause of the Coronavirus. I am petrified, I dont know what to do.
It may be haemorrhoids, especially if bleeding is bright red.
If it is dark, it could be coming from further up, but you can always speak to your doctor over the phone, it will go a long way towards helping your health anxiety rather than stewing over it.
Im glad I forced myself to go about my mouth lump as I would have stewed and stewed and got worse while not doing anything about it.
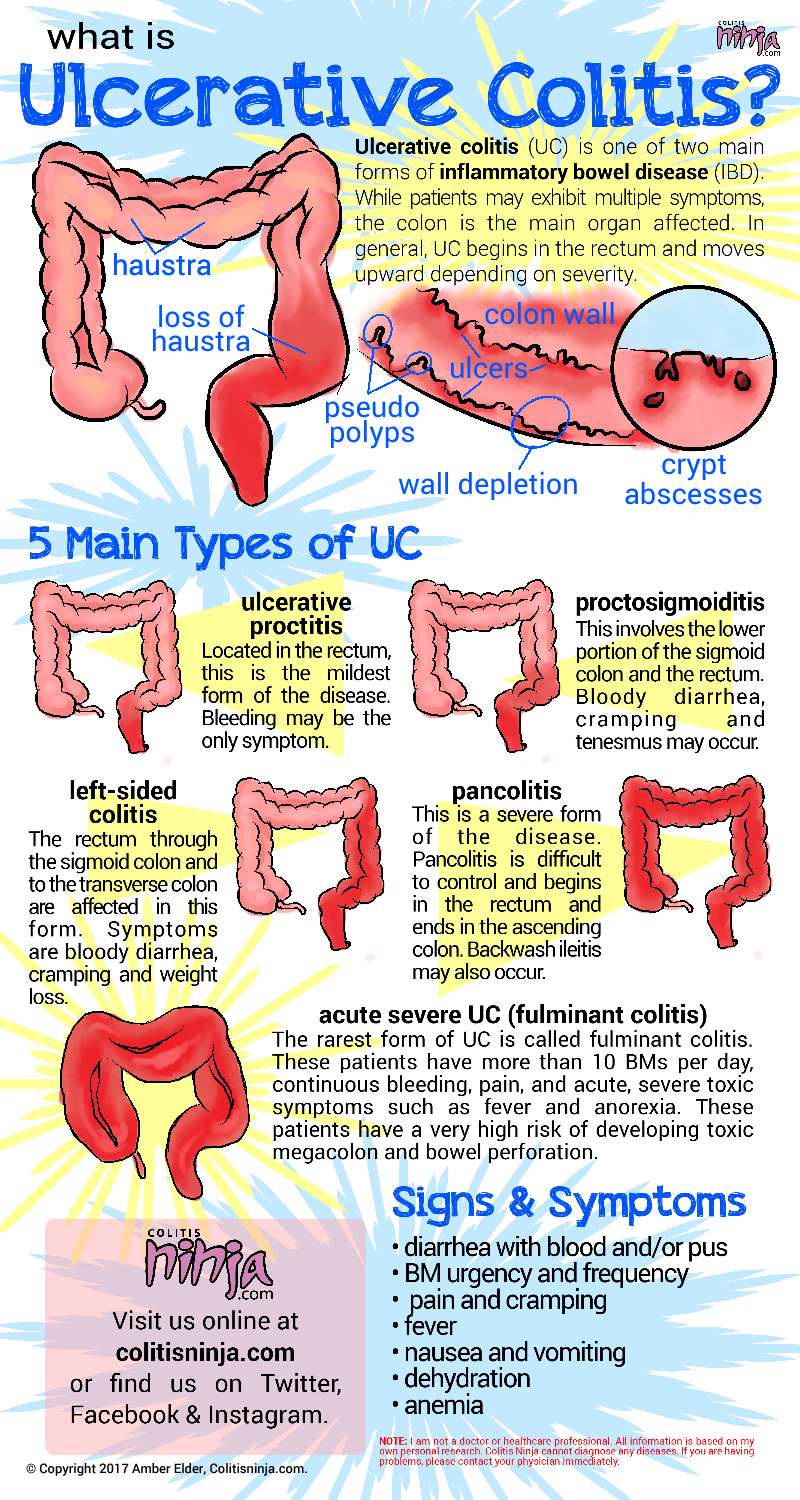
Classifications Of Ulcerative Colitis And Their Symptoms

- Ulcerative proctitis: Inflammation is confined to the area closest to the anus . For some people rectal bleeding may be the only sign of the disease. Others may have rectal pain and a feeling of urgency . This form tends to be the mildest.
- Proctosigmoiditis: Involves the rectum and the lower end of the colon, known as the sigmoid colon. Bloody diarrhea, abdominal cramps and pain.
- Left-sided colitis: Inflammation extends from the rectum up through the sigmoid and descending colon, which are located in the upper left part of the abdomen. Bloody diarrhea, abdominal cramping and pain on the left side and unintentional weight loss.
- Pancolitis: Affects more than the left colon and often the entire colon. Bloody diarrhea that may be severe, abdominal cramps and pain, fatigue and significant weight loss
- Fulminant colitis: A rare, life-threatening form of colitis affects the entire colon and causes severe pain, profuse diarrhea and, sometimes, dehydration and shock. People with this condition are a risk of serious complications, including colon rupture and toxic megacolon, a condition that causes the colon to rapidly expand.
Also Check: Can Ulcers Cause Black Stool
Skin Joint Or Eye Problems
When you have UC, the lining of your large intestine gets inflamed and sets off your symptoms. For some people, this inflammation also shows up in other body parts during a flare. Experts arent sure why.
You could have symptoms like:
Let your doctor know whenever you get new UC symptoms. That way, they can change your treatment plan if needed.
Growth And Development Problems For Children
You can get ulcerative colitis at any age, but its more common among 15- to 30-year-olds. A child with UC may:
- Be underweight
- Red or discolored
Continued
Talk to your doctor right away if youre worried that you might have DVT. Its possible for a deep-vein blood clot to break loose and get stuck in a lung artery. If that happens, its an emergency called a pulmonary embolism . You could have symptoms like shortness of breath, sharp chest pain, and a cough with or without blood. Call 911 if you have these signs.
Doctors can treat DVT and pulmonary embolisms with medications, a filter through a vein that removes the clot, or surgery.
You could be more likely to get DVT or PE if you:
- Have ulcerative colitis that flares often or affects a large amount of your colon.
- Get surgery for severe ulcerative colitis.
Some studies also link certain ulcerative colitis meds, like steroids or tofacitinib, to DVT and PE.
Also Check: Does Stress Cause Ulcerative Colitis
Lifestyle Changes To Treat Ulcerative Colitis
You can make dietary and lifestyle changes to help alleviate symptoms and lengthen time between flare-ups.
While there is no evidence that says certain foods cause ulcerative colitis, there are certain foods that can aggravate your symptoms. Limiting dairy products and avoiding problem foods may help improve your symptoms. Problems foods can vary for each person, but you should also avoid gassy foods such as beans, cabbage and broccoli, raw fruits and fruits, popcorn, caffeine and carbonated beverages. Experiment with fiber. For some, adding more high-fiber foods can help with bowel issues however, if you have an inflammatory bowel disease fiber may worsen your symptoms. Try eating five or six meals instead of two or three large ones and drink plenty of fluids, preferably water.
Avoiding stress is also a good way to alleviate your symptoms. Stress can aggravate your symptoms, so learning to better manage stress can help. Exercise, biofeedback, regular relaxation and breathing exercises are all ways you can manage stress.
When To Contact A Doctor
People need to discuss any blood in the stools with their doctor, even if they have experienced it before.
A person may also wish to monitor their UC symptoms, so they know what is usual for them to experience. People can then discuss any abnormal symptoms with a healthcare professional.
If individuals have ongoing diarrhea that lasts for a couple of weeks, they can contact their doctor to discuss concerns and treatment.
The Crohnâs and Colitis Foundation advises people to seek emergency medical attention if they experience any of the following:
- inability to keep down liquids due to nausea, vomiting, or pain
- rectal bleeding with blood clots in stools
- continuous pain
Managing UC with treatment may help reduce bleeding. There are medications that may reduce inflammation in the rectum and large intestines, which may, in turn, reduce bleeding.
Anti-inflammatory medications for UC can include:
- 5-Aminosalicylic acid: Medication that may help reduce acute inflammation and causes inflammation to become inactive over time.
- Corticosteroids: A short-term treatment to help reduce inflammation.
- Immunosuppressants: These medications can help suppress the immune response that can cause inflammation. However, they may take up to 6 months to be effective.
- Biologics: For treatment of moderate to severe UC, biologics help block molecules that trigger inflammation.
Read Also: Early Stage Venous Leg Ulcer
When Is Blood In The Stool A Cause For Concern
Although bleeding with UC is common, losing too much blood can have severe negative effects on the body. Its essential to recognize the warning signs of significant blood loss and seek help if you start to exhibit these symptoms.
Everyone with UC experiences this symptom differently. When present, bright red blood is often seen on the surface of the stool. However, it may also appear in the toilet bowl, turning the water red.
The amount of bleeding a person with UC experiences also depends on the severity of their condition. Those with mild to moderate UC may only see occasional blood in their stool, while those with severe or active UC may see blood frequently in their bowel movements. In extreme cases, some people may have more than 10 bloody bowel movements a day.
Seek immediate medical care if you experience any of the following while having bloody stools with UC:
- Infrequent or low urination
- Pale, cold, or clammy skin
- Nausea
- Lightheadedness or dizziness upon standing
- Blurry vision
- Severe abdominal cramping
- Heavy and continuous rectal bleeding
Its important to carefully monitor how much blood is normal for you to expect during a flare-up in order to understand what is out of the ordinary. If you do not have these symptoms but notice bleeding from your rectum for more than one or two days, are bleeding more heavily than normal, or are experiencing unusual flare-ups, contact a health care professional.
What Is Ulcerative Colitis Remission
Remission is the ultimate goal. In a given year, 1 to 2 percent of people with ulcerative colitis have severe disease activity, 20 percent have moderate activity, 30 percent have mild activity, and 48 percent are in remission, according to the Crohns and Colitis Foundation of America.
But what exactly is remission? There are two ways to know: symptoms and testing. Bowel movements should average one to three per day, none at night, says Fernando Velayos, MD, a gastroenterologist and director of the Inflammatory Bowel Disease Program at Kaiser Permanente in San Francisco. There should be no urgency, no blood in the stool, and the person should also subjectively feel well.
As symptoms vary among people, your doctor may elect to check objective tests of inflammation to determine if ulcerative colitis is in remission. These can include a stool test, a blood test, a flexible sigmoidoscopy, or a colonoscopy.
Remission is cause for celebration, but that doesnt necessarily mean you can toss out your medications for good.
Ulcerative colitis is a chronic condition characterized by periods of flares and remission, and most people will require some type of maintenance medication. It is important to continue maintenance medications to keep inflammation under control, Dr. Velayos says. Typically, over half of people in remission will relapse within a year if they do not continue with maintenance medication.
You May Like: Does Aleve Cause Stomach Ulcers