When To See A Healthcare Provider
If you have already been diagnosed with a chronic disease that causes a high white cell count, you and your healthcare providers should discuss the signs that your condition is worsening and develop a plan for when you should get medical attention.
Get prompt medical attention if you develop any of the following:
- Sudden or rapidly worsening joint or skin redness, swelling, or pain
- Recurrent nausea, vomiting, or diarrhea
- Sweats or chills
- Dizziness, pale skin, rapid heart rate, or rapid breathing
What Are The Symptoms Of Microscopic Colitis
The trademark symptom of microscopic colitis is chronic, watery diarrhea. In the typical profile, diarrhea occurs frequently about five to 10 times a day, though some people may have it more or less. There have been rare cases reported of people who had microscopic colitis but had no diarrhea or had constipation instead. In these cases, microscopic colitis was found accidentally while looking for something else.
Common secondary symptoms include:
Also Check: Venous Stasis Ulcer Treatment Dressings
Differences Between Ulcerative Colitis And Crohns Disease
The differences between ulcerative colitis and Crohns disease are:
- In Crohns disease, there are healthy parts of the intestine mixed in between inflamed areas. Ulcerative colitis, on the other hand, is continuous inflammation of the colon
- Ulcerative colitis only affects the inner most lining of the colon while Crohns disease can occur in all the layers of the bowel walls
You May Like: How Do You Know You Have A Stomach Ulcer
Don’t Miss: Ulcerative Colitis Rectal Pain Relief
What Are The Complications Of Ulcerative Colitis
Direct complications of UC can include:
- Intestinal blockage and/or tearing
- Abnormal narrowing of the colon
- Slow growth and weight gain
- In the long term, people with UC have a higher rate of colon cancer
Complications outside of the intestine, also called extra-intestinal manifestations, can include:
- Skin: Unusual skin rashes
- Joints: Pain and swelling of joints ankylosing spondylitis
- Eyes: Inflammation of different parts of the eye
- Mouth: Oral sores , which may range in severity from painless to severe and are usually recurrent
- Bone: Reduced bone mineral density
- Blood vessels: Increased risk of blood clotting, especially in the setting of active disease and/or after surgery
- Liver: Inflammation of the liver may occur from IBD or from the associated conditions of autoimmune hepatitis and primary sclerosing cholangitis
- Kidney: Increased risk of kidney stones
- Psychological: UC is often associated with depression and/or anxiety, perhaps due to some combination of inflammation, anemia, malnutrition, and the stress of painful or disruptive symptoms
- Sleep: Increased risk of sleep disorders
There also are a wide range of complications that can be caused by different UC treatments, including drug allergies and side effects. It is sometimes difficult to know whether it is the UC itself or the medications that are the cause of a symptom or problem. If you are concerned that your child is experiencing a complication or a side effect, be sure to discuss it with your doctor.
What Are The Symptoms Of Ulcerative Colitis

Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Also Check: Ulcerative Colitis Is It Deadly
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Crohns Disease Vs Ulcerative Colitis: Differences In Symptoms Causes And Treatment
Crohns disease and ulcerative colitis are part of the group of conditions known as inflammatory bowel diseases . Prior to the 20th century, before the rise of hygiene and urbanization, inflammatory bowel disease was quite rare. Currently, IBD is found in developed countries and is believed to be caused by a lack of germ resistance development although the exact cause is still unknown.
For those living with IBD, their immune system mistakes food and bacteria in the gastrointestinal tract for an allergen or foreign substance, so it sends out cells to destroy it. The result of these attacks is chronic inflammation.
Although the exact causes of Crohns disease and ulcerative colitis are unknown, genetics and environmental factors are believed to play a role. Crohns disease and ulcerative colitis are often interchanged for one another, but we will outline the differences between the two, including symptoms, causes, and treatments in order to provide you with a better understanding of either condition. Continue reading
You May Like: Ulcerative Colitis Flare Up Length
Whats The Difference Between Inflammatory Bowel Disease And Irritable Bowel Syndrome
IBD is a disease IBS is a syndrome, or group of symptoms. The causes and treatments are different.
IBS is a type of functional gastrointestinal disease. It affects how the bowels function, causing them to contract more often than usual. IBS is also known as spastic colon or nervous stomach.
IBS doesnt inflame or damage the intestines like IBD, so imaging scans cant detect it and it doesnt increase the risk of colon cancer. People with IBS rarely need hospitalization or surgery.
You And Your Care Team Are In Control
While there is no cure for UCwhile also knowing it can progress and symptoms can get worse over timeits important to remember that you and your doctor can get your disease under control. Recognizing the signs early and getting treatment right away is key. Thats why having open conversations with your doctor and being prepared for every appointment is crucial to managing your UC.
Speak openly with your doctor about how much your UC is truly impacting you. Make a personal action plan to see how much of your time your disease is affecting and get customized steps to help you and your doctor get control of your disease.
You May Like: What Foods Not To Eat If You Have An Ulcer
Also Check: Symptoms Of Ulcer In Female
Ulcerative Colitis Vs Crohns Disease
Ulcerative colitis and Crohns disease share similar symptoms and they are both types of inflammatory bowel disease , but they are not the same illness and they affect different areas of the GI tract.
- Can affect the entire thickness of the bowel wall
- Only the colon and rectum are affected
- Affects the inner-most lining of the large intestine
- What is Ulcerative Colitis?
What Are The Symptoms Of A Flare
A flare is characterised by inflammation that damages the lining of the digestive tract. It causes lesions that can turn into open sores that heal leaving scar tissue.
| Whole digestive tract, mostly the small intestine | |
| Ulcerative colitis | Colon, starting at the rectum and moving inwards |
The most common Crohns disease symptoms and symptoms of ulcerative colitis are the same. Always consult a doctor if you are worried about your digestive health, especially if you experience chronic pain, weight loss and/or bleeding.
| Bloody stools |
| Frequent, urgent stools |
Factors that can trigger flares include missing IBD medication, taking non-steroidal anti-inflammatory drugs , antibiotics, stressful events and certain types of food. Smoking is a trigger for Crohns, but not for ulcerative colitis.
Also Check: What To Eat When You Have Ulcerative Colitis
Read Also: What To Do If You Have A Stomach Ulcer
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Diagnosing Inflammatory Bowel Disease

In inflammatory bowel disease, or IBD, there is persistent inflammation in the gastrointestinal tract. The condition causes symptoms such as abdominal pain, diarrhea, bloody stool, constipation, and an urgent need to have a bowel movement. The most common types of IBD are Crohns disease and ulcerative colitis.
Gastroenterologists at NYU Langones Inflammatory Bowel Disease Center are experts in the gastrointestinal tract and can recommend the appropriate diagnostic tests to determine the cause of your symptoms. There is no single definitive test to confirm the presence of IBD, so the condition is diagnosed based on a combination of tests, including endoscopy, biopsy, and imaging tests.
Read Also: How To Treat H Pylori Ulcer
This Factsheet Is About Ulcerative Colitis
Ulcerative colitis is a disease of the rectum and the large bowel, . Ulcerative colitis is thought to affect around 1 in 420. The peak age of incidence between 15-25 years old with a smaller peak occurring between the age of 55 and 65 years old. But it can occur at any age.
INFLAMMATORY BOWEL DISEASE
Ulcerative colitis is one of a group of conditions that are known as Inflammatory bowel diseases, which also includes Crohns disease. Inflammatory bowel disease is different to Irritable Bowel Syndrome , which can cause similar symptoms but does not involve inflammation. The term colitis means the large bowel has become inflamed and if this becomes severe enough ulcers may form in the lining of the large bowel.
Ulcerative Colitis Needs Innovation
UC is an ongoing type of inflammatory bowel disease that occurs because of an abnormal immune system response. The condition causes inflammation of the cells lining the colon and extends into the rectum. UC commonly affects adults aged between 30 and 40 years and can often results in disability.
A diagnosis of UC can be life changing, especially as many people are diagnosed as young adults 1 at a critical time in their lives, when they are moving away from home to study, starting a career, and embarking on their first serious relationships building an independent life. We have heard from those living with UC that they would rather not attend social occasions, parties with friends, but will stay at home to avoid getting into an embarrassing situation where they cant reach a toilet in time. For many of these young people diagnosed with UC, the idea that this is a life-long condition can make it more difficult to accept.
Living with ulcerative colitis is like having a dormant volcano existing inside me.
Ulcerative Colitis patient
My disease is under control, but my weight is out of control. I have lost all my confidence.
Ulcerative Colitis Patient, Italy
Around half of people living with moderate to severe UC or CD fail to achieve a sustained control of their disease on currently available therapies, indicating a need for new, alternative treatments. 2,3,4,5
Burden of UC
Ulcerative Colitis patient, UK
Our commitment to UC
Dr. Walid Abi-Saab
Recommended Reading: Best Foods To Eat When You Have A Stomach Ulcer
What Is Ulcerative Colitis
Ulcerative colitis is a long-lasting inflammatory bowel disease that causes inflammation and ulcers in the large intestine. The large intestine includes the rectum and colon. In patients with UC, the immune system mistakingly targets the lining of the large intestine. This can cause inflammation, ulceration, bleeding, and diarrhea in the colon and rectum.
Colon Cancer And Ulcerative Colitis
When you have ulcerative colitis, you may be more likely to get colon cancer. Your chances go up if you don’t get treatment for UC. That’s because unchecked inflammation can cause changes in the cells in your colon. These cells may turn into cancer down the road.
Your chances of getting colon cancer go up if you’ve had ulcerative colitis for 8 years or longer. The odds are also higher if:
- Your inflammation doesn’t go away.
- You have a liver condition called primary sclerosing cholangitis.
- You have a family member who’s had colon cancer.
Some research shows that people with UC may be less likely to get colon cancer now than in the past. Experts think it’s because doctors now have better ways to screen for colon cancer and they do it more often. It also helps that new medicines, like biologics, do a good job of curbing inflammation.
You May Like: How Long Ulcerative Colitis Flare Last
What Does Pancolitis Mean Causes Symptoms Treatment And Diet
Pancolitis refers to inflammation of the entire colon. The word is quite descriptive in itself as the word pan means all or entire, while the word colitis refers to inflammation of the colon. This is often a result of a medical condition, most commonly ulcerative colitis , which is a disease that is known for causing inflammation and ulcers in the lining of the large intestine. Approximately 2040 percent of UC patients suffer from pancolitis.
There are several different types or classifications of ulcerative colitis, all of which depend on the location of the inflammation. For example, UC patients with inflammation of the rectum would be classified as having proctitis, while UC patients with inflammation of the rectum and sigmoid colon would be referred to as having proctosigmoiditis. Those UC patients having inflammation of the entire colon may also be referred to as having pan-ulcerative colitis
Other inflammatory condition may also cause pancolitis and include autoimmune diseases such as rheumatoid arthritis and infections with bacteria such as Clostridium difficile. Continue reading
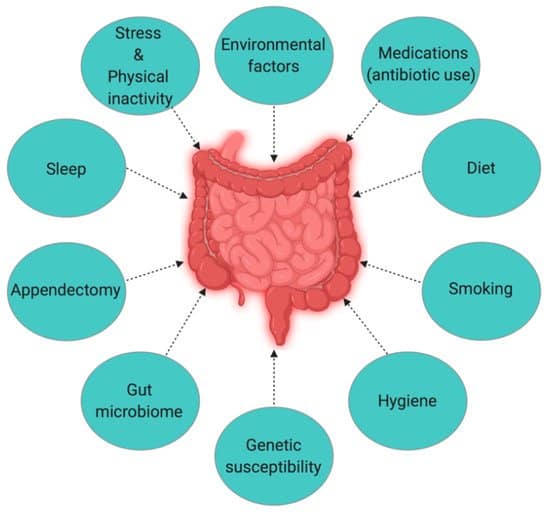
Causes Of Ulcerative Colitis And Crohns Disease
There are multiple contributing risk factors that can lead to ulcerative colitis and Crohns. Evidence does suggest that both are associated with an inappropriate immune response, which can arise from many different environmental factors, gut microbiome imbalance, as well as genetics .
The body creates temporary inflammation as part of a normal immune system response to threats and foreigners that may cause harm. An inappropriate immune response occurs when the immune system attacks something that is probably not harmful or overreacts to a possible pathogen. This creates unnecessary or excessive inflammation that can become chronic inflammation.
For example, in addition to toxins and infections, the immune system may attack food particles, beneficial gut bacteria, and, in the case of ulcerative colitis and Crohns disease, the lining of the digestive tract [1
What might be causing the inflammation of the digestive tract and an inappropriate immune response?
Some of the contributing factors in IBD are:
Don’t Miss: Ulcerative Colitis Biologics Side Effects
What Does Ulcerative Colitis Look Like
With UC there is a wide variation in the amount of inflammation from person to person, so that in mild cases the bowel can look almost normal but, when the inflammation is bad, the bowel can look very red and ulcerated. Ulcerative colitis usually affects the rectum, but occasionally there is no inflammation . Sometimes the inflammation is limited just to the rectum . However, the inflammation can involve varying lengths of the colon. When the whole large bowel is affected, this is called pan-colitis .
What Causes Infectious Colitis
Infectious colitis is not to be confused with other types of colitis, such as ulcerative colitis. Ulcerative colitis is an inflammatory bowel disease, but its causes are normally due to infections from bacteria, viruses, parasites, or fungus. The term colitis refers to the main symptom, which is diarrhea.
Infectious colitis is often linked with food poisoning, which is an infection of the stomach and rectum. The most common cause of a food poisoning type of infectious colitis is contaminated water, and it comes from a parasite called entamoeba histolytica. You can also experience sudden diarrhea after consuming food contaminated with bacteria. E-coli, salmonella, shigella, yersinia, or campylobacter are all bacterial intestinal infections. Continue reading
Read Also: Yea Sacc For Horses With Ulcers
Treatment Of Ibd Complications
Treatment depends on the particular complication, but may include:
- complications caused by nutritional deficiencies vitamin and mineral supplements , changes to diet or a liquid diet in severe cases
- inflammation in other body areas usually ease when the bowel inflammation is controlled with medication
- fistulas small openings that often heal by themselves, with treatment to ease the inflammation. A person may need surgery to close a larger fistula. Abscesses may need antibiotics and surgical drainage
- intestinal obstruction in some cases, medical treatment to ease the inflammation will clear the obstruction. In severe cases, the person will need surgery
- toxic megacolon the person goes to hospital, and receives fluids and nutrients intravenously instead of by mouth, plus antibiotics and steroids to reduce inflammation. Sometimes, the doctor will remove the contents of the persons stomach with a slender tube . A ruptured bowel needs surgical repair or removal. In severe cases, the whole of the large bowel may need to be surgically removed.
What Are The Signs And Symptoms Of Ulcerative Colitis
People with UC may have some or all of these symptoms:
- Abdominal pain: The pain may be in the lower left part of the abdomen or more generalized around the abdomen. This pain may be persistent, severe, and could possibly wake your child from sleep.
- Diarrhea: Passage of watery stool or frequent stool that is different from your childs normal pattern. It could be mild to severe and may frequently wake your child from sleep.
- Tenesmus: This is the sensation of fullness in the rectum, which may lead a person to feel that they still need to use the toilet even after they have passed a bowel movement.
- Blood in the stool
- Skin changes, which may look like sores, bruises, or large hives on the shins
- Constipation: Although not typical, some people with UC have constipation, although this is usually in combination with other symptoms.
Other symptoms, referred to as extra-intestinal manifestations, occur outside the digestive tract. These are detailed in the complications section below.
Your primary care physician will perform an initial evaluation if you are concerned that your child has UC. Ask your doctor for referral to a pediatric gastroenterologist if your child has blood in the stool, persistent diarrhea, persistent abdominal pain, weight loss, or slow growth.
Read Also: Support Surfaces For Pressure Ulcer Prevention
Don’t Miss: Ulcerative Colitis Diet During Flare