Risk Factors For Relapse
Choice of maintenance treatment is determined by disease extent , disease course , failure and adverse events of previous maintenance treatment , severity of the most recent flare , treatment used for inducing remission during the most recent flare , safety of maintenance treatment , and cancer prevention
Patients with disease requiring steroids probably have a different outcome compared with the overall population of patients with UC. In a population-based study, the outcome of 183 patients with UC diagnosed between 1970 and 1993 was analysed 1 year after a first course of steroids.236 Among the 63/183 patients treated with corticosteroids, 49% had a prolonged response, 22% were steroid dependent, and 29% came to colectomy, but only 3/183 were treated with thiopurines.
Lifestyle Changes For Ulcerative Colitis
While medical treatment can help control UC and keep it in remission, changing certain lifestyle factors can also help you live well with the disease.
These changes can help lessen the severity of UC. If your UC does worsen, being continuously monitored by your healthcare team can boost chances of early detection and improve colon cancer survival rates.
Lifestyle changes you can consider making include:
- Having regular cancer screening via colonoscopy
- Seeing your gastroenterologist annually, or more often as needed
- Eating a diet that is high in vegetables, fruits, and whole grains
- Limiting dairy product intake
- Reducing your intake of red meat and processed meats, which are connected to risk of colorectal cancer
- Limiting alcohol intake or avoiding it altogether
- Drinking a lot of liquids, all day long
- Eating smaller meals throughout the day
- Exercising regularly
Eating When You Are In A Flare
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
You May Like: Different Types Of Ulcerative Colitis
Treatment According To Site Of Disease And Disease Activity
11.2.1. Proctitis
A mesalamine 1-g suppository once daily is the preferred initial treatment for mild or moderately active proctitis . Mesalamine foam or enemas are an alternative , but suppositories deliver the drug more effectively to the rectum and are better tolerated . Topical mesalamine is more effective than topical steroids . Combining topical mesalamine with oral mesalamine or topical steroids is more effective
Refractory proctitis may require treatment with systemic steroids, immunosuppressants, and/or biologics
Topical mesalamine is the first-line therapy for proctitis. A Cochrane systematic review of 38 clinical trials of treatment of proctitis and left-sided colitis confirmed its superiority over placebo for inducing symptomatic, endoscopic, histological response and remission.5 The pooled odds ratio was: 8.3 for symptomatic remission 5.3 for endoscopic remission and 6.3 for histological remission . Suppositories are more appropriate than enemas in proctitis as they better target the site of inflammation and are more acceptable for patients.6 There is no dose response for topical therapy above a dose of 1 g 5-ASA daily.5,7 Once-daily topical therapy is as effective as divided doses.8,9
11.2.2. Left-sided ulcerative colitis
11.2.3. Extensive ulcerative colitis
As the majority of clinical trials in mild to moderate UC include patients with both extensive and left-sided colitis, much of the evidence base for this statement is discussed in section 11.2.2.
Acg Releases Updated Practice Guidelines For Ulcerative Colitis In Adults
KAREN HELLEKSON, PH.D.
Am Fam Physician. 2005 Feb 1 71:604-611.
The American College of Gastroenterology’s Practice Parameters Committee has issued updated practice guidelines for the treatment of ulcerative colitis in adults. The guidelines were generated by an expert panel’s review of published evidence and outline the preferred approaches to the treatment of patients with ulcerative colitis, a chronic disease characterized by diffuse mucosal inflammation of the colon and marked by bloody diarrhea, rectal urgency, and tenesmus. Ulcerative colitis affects 250,000 to 500,000 people in the United States each year resulting in steep hospital and drug costs as well as lost work. The full text of the updated practice guidelines, which originally appeared in the July 2004 issue of the American Journal of Gastroenterology, is available at http://www.acg.gi.org/physicians/guidelines/UlcerativeColitisUpdate.pdf.
The quality of evidence on which a recommendation is based is as follows:
Grade A: Homogenous evidence from multiple well-designed randomized or cohort controlled trials, each involving a number of participants to be of sufficient statistical power.
Grade B: Evidence from at least one large well-designed clinical trial with or without randomization, from cohort or case-control analytic studies, or well-designed meta analyses.
Grade C: Evidence based on clinical experience, descriptive studies, or reports of expert committees.
Don’t Miss: Support Surfaces For Pressure Ulcer Prevention
Surgery For Managing Uc Flare
Surgery may be used to manage the symptoms of ulcerative colitis when other treatments are unable to get the disease under control . While surgery can often eliminate UC entirely, it usually requires removing the entire colon and rectum in a procedure called a total proctocolectomy. Some people with UC later have another procedure to create a J-pouch .
Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
Read Also: Best Treatment For Diabetic Foot Ulcer
Complementary And Alternative Medicine
Probiotics may modestly reduce disease activity in active disease, but do not increase remission rates.34 However, Lactobacillus GG and Escherichia coli Nissle 1917 have been shown to be as effective as 5-ASA for maintenance therapy.16,17 Acupuncture has shown a small symptomatic benefit in active disease.35 Wheatgrass has also shown some effectiveness in reducing symptoms of active disease.36
Corticosteroids Vs Anabolic Steroids
Though corticosteroids are referred to as steroids, they are not the same as the steroids some athletes use for performance enhancement. These steroids, known as anabolic steroids, are human-made versions of testosterone. Taking corticosteroids for UC does not have any testosterone-producing effects on the body.
Recommended Reading: Ulcerative Colitis And Lung Disease
Canceling Plans Due To Ibd Flare
Trying to manage a social and work-life balance while also juggling inflammatory bowel diseases like Crohns disease and ulcerative colitis can be difficult. You may have found yourself canceling plans or avoiding making plans due to your symptoms, provoking feelings of anxiety, loneliness, and isolation.
It is estimated that 50 percent of people with IBD who receive medical or surgical treatment will remain in remission for five years. This promising data highlights the fact that with the right treatment plan and open communication with your doctors, family, and close friends, a robust and fulfilling life outside your house is possible.
Canceling plans may be unavoidable when you live with a chronic illness like Crohns disease or ulcerative colitis. However, planning ahead for social situations, managing your emotional stress, and taking steps to prevent flare-ups can help you feel more comfortable leaving the house, and may minimize the times you have to cancel.
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Read Also: Side Effects Of Ulcerative Colitis
How Do Steroids Work
Steroids work by stopping the production of certain chemicals in the body that produce inflammation.
The body naturally produces steroid hormones in the adrenal cortex. The adrenal cortex produces certain hormones to regulate a variety of bodily functions, such as the fight-or-flight response and the inflammation response.
Corticosteroids mimic these natural hormones to produce anti-inflammatory effects.
Active Uc Of Any Extent Not Responding To Aminosalicylates
In mild-to-moderate UC of any extent, aminosalicylates such as mesalamine are the preferred initial treatment . In patients with disease activity limited to the rectum, topical therapy alone might suffice, but combination therapy is more effective and is also recommended for left-sided and extensive UC . Table 2 gives an overview on current treatment options.
Table 2.
Medical therapy for UC
Fig. 1.
Active ulcerative colitis of any extent not responding to 5-aminosalicylates . MMX, multimatrix AZA, azathioprine 6-MP, 6-mercaptopurine.
Except in case of isolated proctitis, where topical corticosteroids alone may be considered, treatment with oral corticosteroids should be initiated in patients who do not respond adequately to 5-ASA . In case of isolated proctitis, topical corticosteroids alone might be considered. The introduction of corticosteroids should be a shared decision-making process that includes patients preference of therapy and tolerance to 5-ASA. It is, however, recommended to start corticosteroids in patients with sustained rectal bleeding for 2 weeks, persistent abdominal symptoms after 6 weeks of adequate therapy with 5-ASA or if symptoms deteriorate . In selected cases, a prolonged therapy with up to 16 weeks might still be able to achieve remission.
Don’t Miss: Surgical Management Of Ulcerative Colitis Ppt
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Recommended Reading: Food To Avoid For Ulcer Patient
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Indications For Urgent Hospital Referral
- Patients with severe colitis should be admitted to hospital for assessment and treatment.
- Patients with moderate disease, who fail to respond to steroids within two weeks, should be admitted to hospital.
- Patients who respond partially to treatment should be seen urgently in the outpatient department and treated for refractory colitis.
Also Check: How Can You Tell If You Have An Ulcer
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Medications For Managing Uc Flare
There are many medications used to manage UC flares.
Aminosalicylates
The first step in treating mild to moderate IBD is often 5-aminosalicylic acid . Commonly prescribed aminosalicylates include Azulfidine , Asacol HD or Delzicol , Colazal , Dipentum , Lialda or .
Corticosteroids
Corticosteroids, including prednisone, are used to treat moderate to severe ulcerative colitis. These are generally only given in the short term due to their side effects. If you have been on steroids for greater than three months, it is time to talk with your health care provider. In the setting of the COVID-19 pandemic, Dr. Kinnucan advises caution when using steroids, as they increase the risk for severe COVID-19.
Immunomodulators/Small Molecules
Like aminosalicylates and corticosteroids, immunomodulators or small molecule therapies reduce inflammation. Unlike those other drugs, however, immunomodulators work by suppressing the immune response that leads to inflammation. There are several types of immunomodulators that work in different ways to treat UC. Immunomodulators prescribed for ulcerative colitis include Imuran and Purinethol .
Zeposia is the first sphingosine 1-phosphate receptor modulator approved by the U.S. Food and Drug Administration to treat ulcerative colitis. It was approved to treat ulcerative colitis in 2021. Zeposia and other similar drugs are approved to treat multiple sclerosis.
Biologics
Don’t Miss: What Are Some Symptoms Of An Ulcer
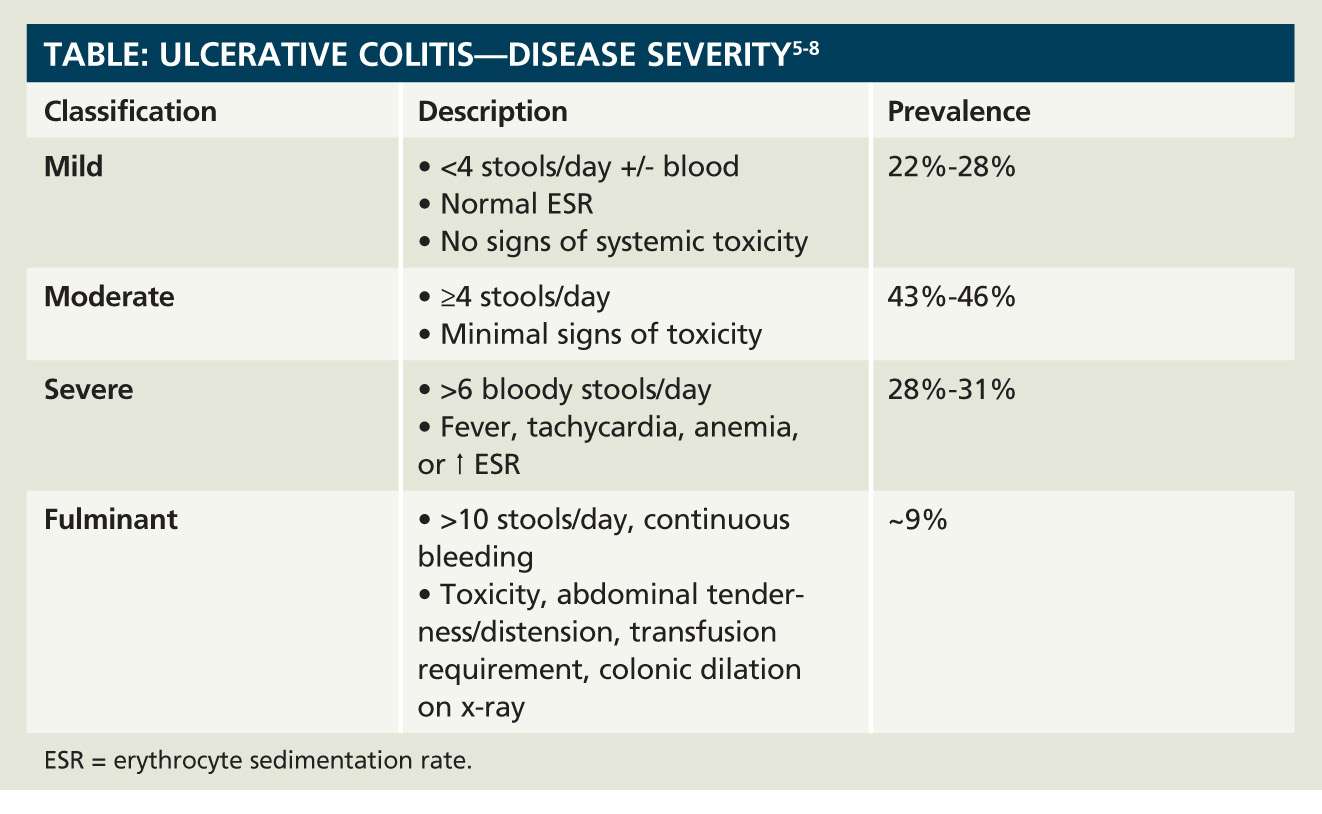
Disease Severity In Ulcerative Colitis
The National Institute for Health and Care Excellence uses the categories of disease severity of mild, moderate and severe, based on the Truelove and Witts’ severity index for adults and the Paediatric Ulcerative Colitis Activity Index for children and young people.
For adults:
- Mild: fewer than four stools daily, no more than small amounts of blood in stools, no anaemia, pulse rate not above 90, no fever and normal ESR and CRP.
- Moderate: four to six stools a day with more blood in stools than for mild disease. No anaemia, pulse rate not above 90, no fever and normal ESR and CRP.
- Severe: six or more stools per day, visible blood in stools and at least one feature of systemic upset .
PUCAI for children and young people includes scoring of the presence and severity of abdominal pain, rectal bleeding, stool consistency of most stools, number of stools per 24 hours, stools causing wakening at night and level of activity. Details can be found in the NICE guideline.
Subacute ulcerative colitis is defined as moderately to severely active ulcerative colitis that would normally be managed in an outpatient setting and does not require hospitalisation or the consideration of urgent surgical intervention.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health

Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Recommended Reading: Black Tarry Stools Ulcerative Colitis
Stress Anxiety And Depression
As with many chronic health conditions, UC can take a toll on mental health. This stress can, in turn, worsen UC symptoms and lead to flares. Studies have found that stress triggers a series of reactions in the body that suppress the immune system, causing inflammation of the intestines. Additionally, stressful emotions, such as anxiety and depression, have been found to cause abdominal pain in people with IBD.
Flare-ups can be exacerbated in the setting of recent life stressors, such as the loss of a job, Dr. Kinnucan said. Anxiety and depression can contribute to an increase in clinical symptoms in people with IBD, and may worsen quality of life, she added. It is important to address symptoms of anxiety or depression with your health care provider.