What Triggers Microscopic Colitis
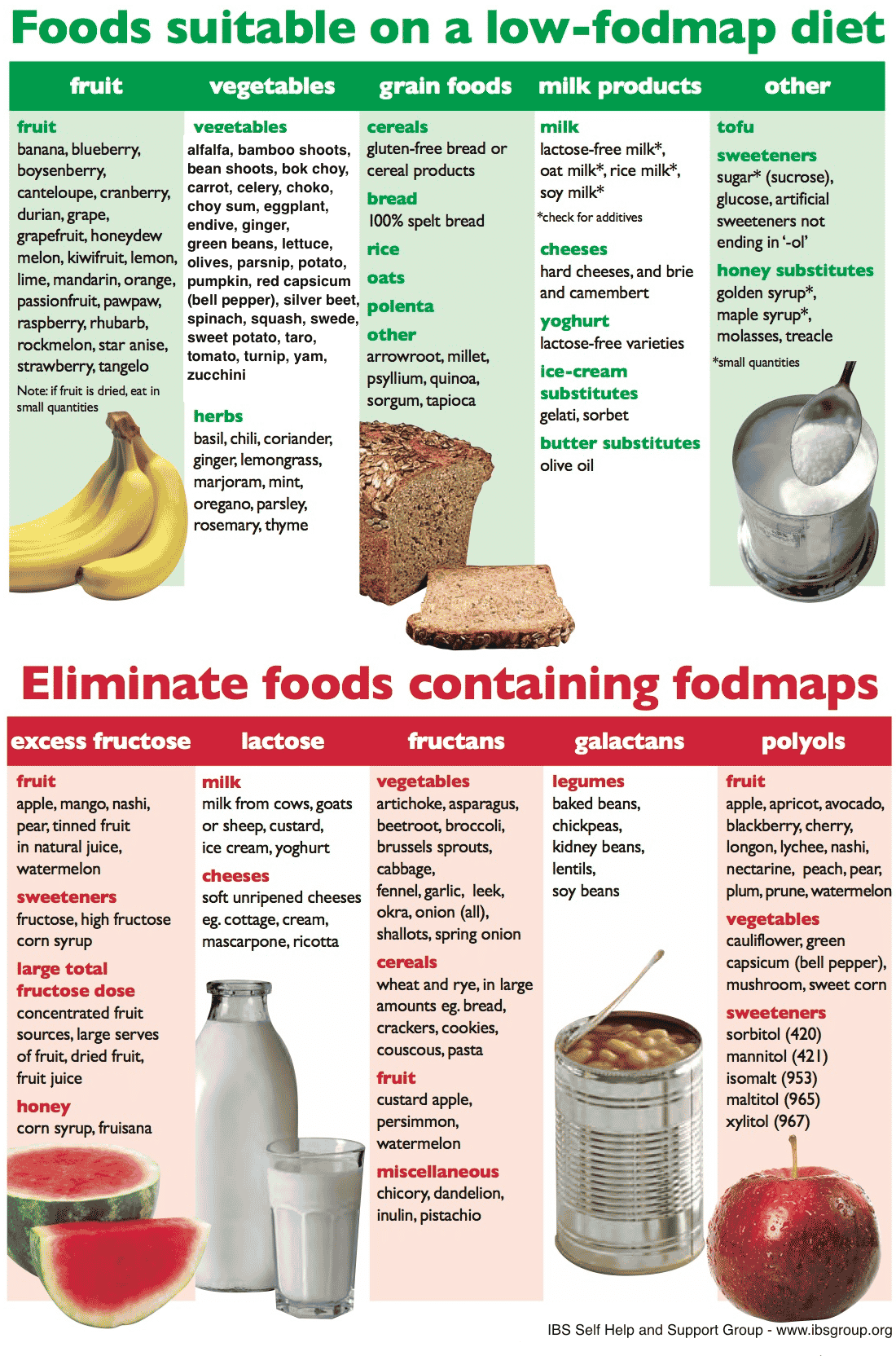
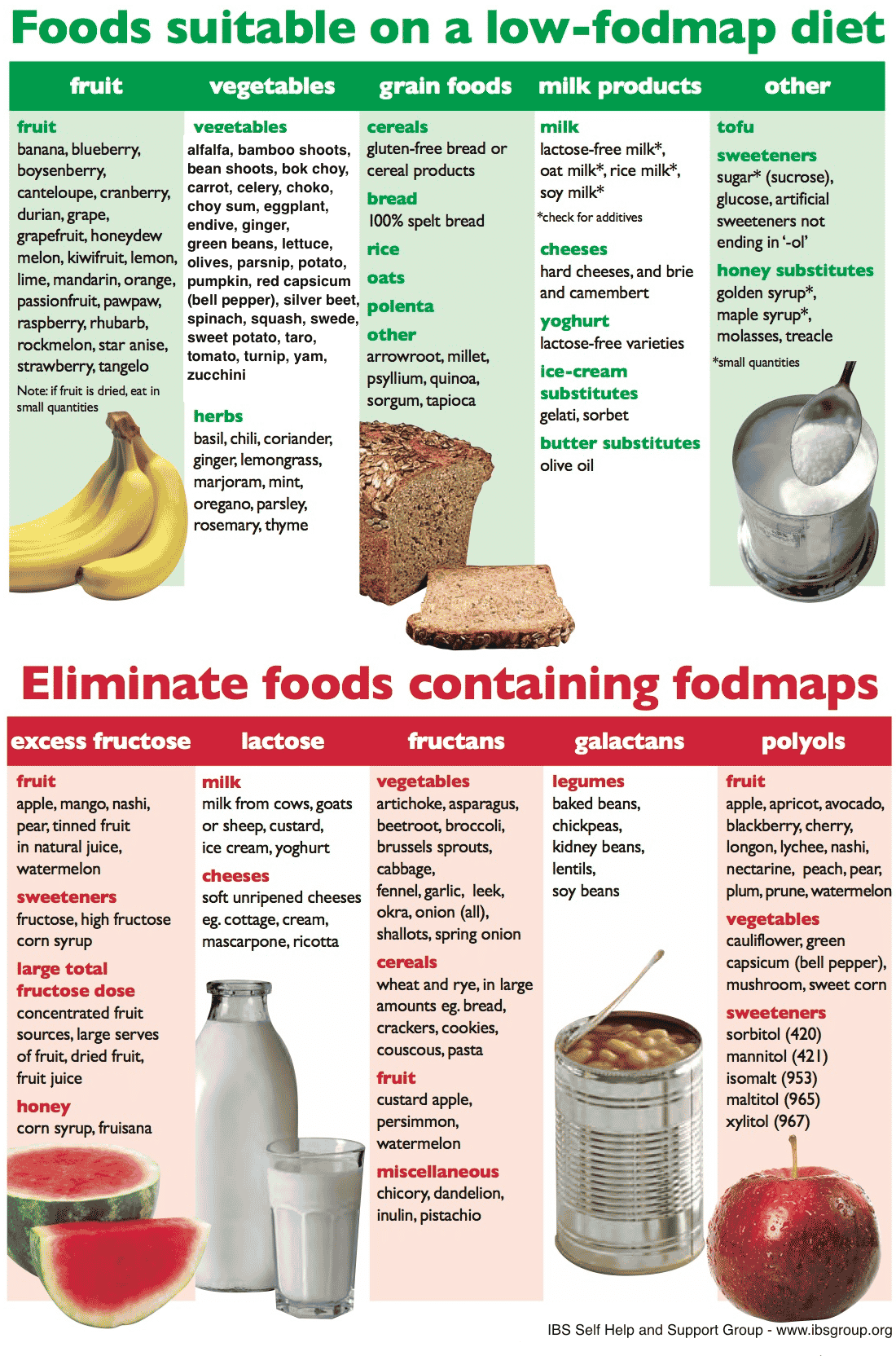
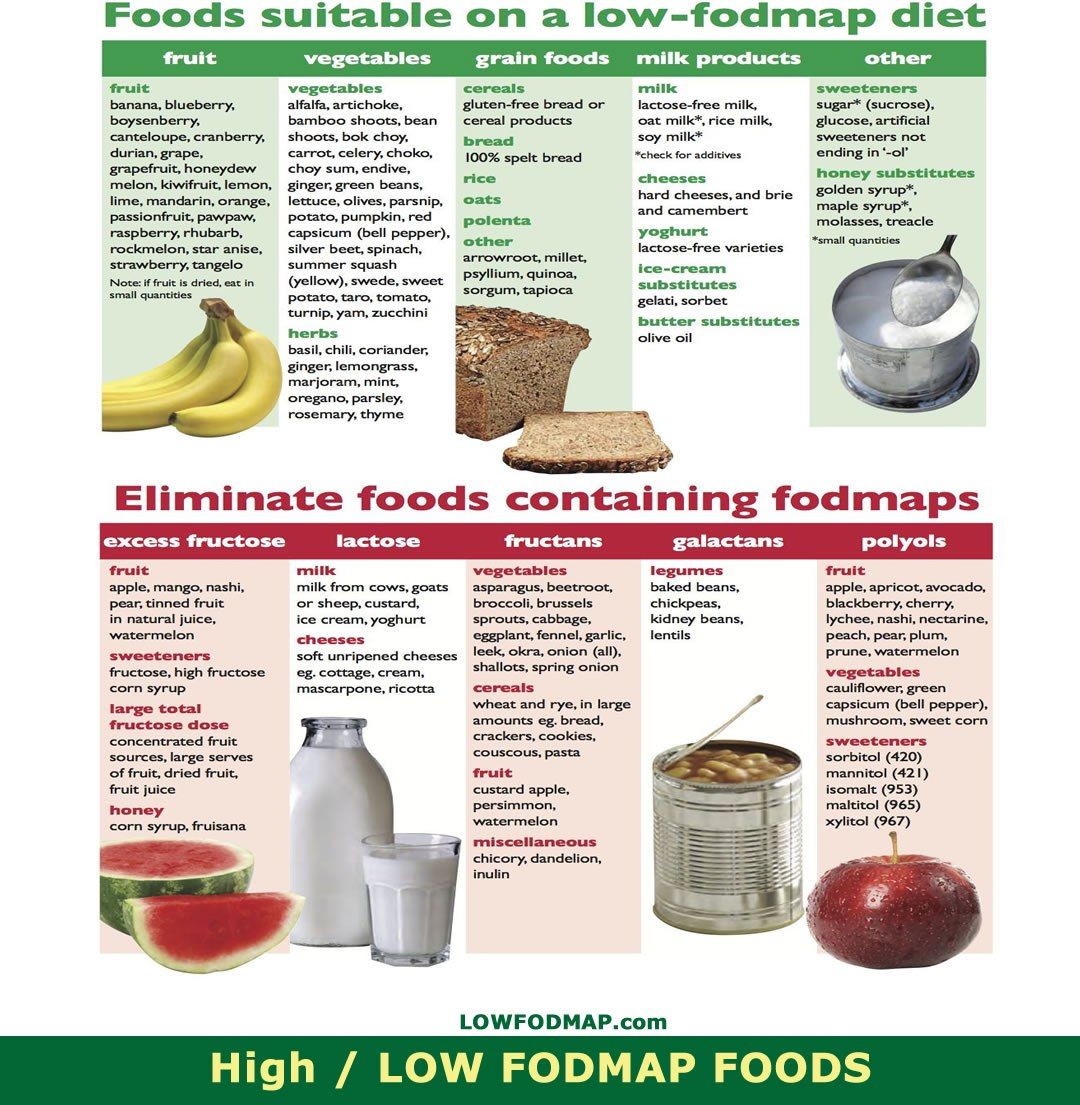
Although a low-FODMAP diet is not very useful in treating microscopic colitis, several foods and lifestyle activities can trigger the condition, and avoiding them is useful.
Fatty, high-fiber foods, dairy products, gluten-containing items, caffeine, sugar, inadequate hydration, spicy foods, and eating large meals can all make microscopic colitis worse. If you have the condition, consider avoiding the following items:
- Raw veggies
Many patients with microscopic colitis also have celiac disease. If you have microscopic colitis, your chances of developing celiac disease are higher than the average population. In celiac disease, your body is intolerant to a protein called gluten. Gluten is found in bread, pasta, breakfast cereal, and cakes.
If you develop abdominal symptoms after eating gluten-containing items, you may have celiac disease on top of microscopic colitis. The only treatment for celiac disease is lifelong avoidance of gluten.
Note that food sensitivities vary between patients. What worsens your symptoms might be completely fine for another patient and vice versa. Instead of eliminating everything in this list, keep a food diary.
In a food diary, you write everything you eat, the serving size, and the how you feel after eating a particular food. At the end of a month or two, you can analyze the diary and identify the foods that trigger your microscopic colitis. You can then avoid those items.
The Specific Carbohydrate Diet
The Specific Carbohydrate Diet was specifically designed to help treat Celiac disease, but it has since been recommended for Ulcerative Colitis, Irritable Bowel Syndrome, Inflammatory Bowel Disease, and Crohns Disease. The main takeaway from this whole article should be some of our intestines dont digest grains or sugars well!
The Specific Carbohydrate diet, like the Low-FODMAP diet is considered an elimination diet, which is a diet where you eliminate trigger foods during flare-ups to help battle your painful symptoms. On this diet, you eliminate carbohydrates that are complex to digest. You may be tired of hearing this, but the top two foods you need to quit on the SCD are grains and dairy. This diet can be hard to follow long-term since there are so many foods you have to eliminate, so dont feel bad if you feel like you cant keep up. Long-term diets arent really sustainable, which is why I suggest a trial period to see how your gut is feeling, but also to see how youre managing mentally.
Ulcerative Colitis Vs Crohns Disease
Crohns Disease is another inflammatory bowel disease that shares similarities to ulcerative colitis, with a few key differences. The first is that Crohns disease can technically occur along the entire length of the GI tract, as opposed to ulcerative colitis occurring exclusively in the colon. Crohns disease also presents in discontinuous patches as opposed to the continuous diseased areas in ulcerative colitis. Imbalances in gut bacteria tend to be more pronounced in Crohns disease than ulcerative colitis. Finally, the inflammation in ulcerative colitis typically does not go as deeply into the gut tissue layers as in Crohns disease, but both diseases show evidence of gut barrier dysfunction, or leaky gut.
Don’t Miss: Succeed For Horses With Ulcers
What Is Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease that affects that affects the colon, or large intestine. Typically, the inflammation starts in the rectum and then extends continuously throughout the colon. It is commonly diagnosed in your thirties, and takes a flare and remission pattern where sometimes you feel okay and other times you dont.
Diet Types To Consider For Ulcerative Colitis
What diet type is best for those who suffer from Ulcerative Colitis? This is a question many have pondered on and struggled with throughout the history of irritable bowel diseases. There is no single diet proven to aid in decreasing UC symptoms. We definitely know its NOT a diet filled with inflammatory foods, but a diet filled with easily digestible nutritious food for your gut. There are a plethora of recommended diet types for those who suffer from UC. Theres the Mediterranean diet, the Low-FODMAP diet, the gluten-free and dairy-free diet. The only way to know what works best for you is to try an elimination diet or stick with a diet that prevents flare-ups and doesnt upset your gut. How do you know what foods dont upset your gut, you ask. Simply put, going through a period following one diet, meal planning, tracking your symptoms, and food intake with a food diary or food journal tracker will help you pinpoint what foods make you feel good , and what foods make you feel bad.
You mightve read food diary, and immediately gotten anxious at the complexity of tracking your food and figuring out what your body can tolerate. Dont be worried, or scared! Logging your food with a food diary isnt as complex as it sounds.
These tips should not be used for anything other than educational purposes. To develop a safe, personalized meal plan, you MUST work with your doctor or a dietitian.
Read Also: Is Okra Good For Ulcerative Colitis
Effect Of Increasing Fodmap Intake
The final aspect is whether increasing FODMAP intake, specifically with oligosaccharides for their putative prebiotic effect, is of value in patients with IBD. It was noted previously that patients with Crohn’s disease tended to eat fewer fructans than did healthy controls. In a pilot study, supplemental fructans had promising anti-inflammatory effects, but a well-powered subsequent study had no impact on inflammation and induced greater symptoms. The interpretation of those results is confounded by the fact that background diets were not assessed for prebiotic intake. High doses of inulin were evaluated in a blinded cross-over study of 20 patients with pouch inflammation. While symptoms did not improve, inflammatory activity in the pouch did. Hence, the value of supplementing prebiotic oligosaccharides, either as supplements per se or by food choice warrants further study.
Scd And Low Fodmap Diet For Ulcerative Colitis
There is a lot of interest but limited clinical evidence for the use of the specific carbohydrate diet and low FODMAP diet for ulcerative colitis.
In one trial, a low FODMAP diet did appear to improve quality of life and symptoms of ulcerative colitis, without improving fecal calprotectin or C-reactive protein, two markers of inflammation. If you are experiencing a lot of IBS-like symptoms, it may be a temporary option to help get symptoms under control.
I have also used low FODMAP foods as a lower fermentation framework for increasing fruit and vegetable intake for those who are currently eating a low fiber diet. I worry about the adoption of a long-term low FODMAP diet in ulcerative colitis as I believe that it might be simply tamping down symptoms by further altering the gut microbiomewhich could be detrimental for long term gut health.
The specific carbohydrate diet is based on a decades-old book called Breaking the Vicious Cycle. To my mind, it is similar to a low FODMAP approach in that it alters the types of carbohydrates available for fermentation in the gut.
It is not uncommon for those who have UC to feel that an SCD diet is helping if that is the case, we will support our client on that chosen path however, I dont believe it is a solution for long term gut health and wont advocate for it in practice. It is a complex diet to follow and isnt supported by the evidence.
Don’t Miss: Best Cure For Mouth Ulcers
When Should You See A Doctor About Ulcerative Colitis Food Triggers
According to Dr. Schwimmer, seeing a doctor at the first sign of ulcerative colitis symptoms is your safest bet, especially if youve never been formally diagnosed. Concerning, unexplained symptoms like bloody stool, diarrhea, and abdominal cramping shouldnt be ignored, because even if its not ulcerative colitis, you might be dealing with something else that needs proper treatment.
After youve been diagnosed, your doctor might recommend making diet adjustments as a part of your ulcerative colitis treatment plan. But ultimately, FDA-approved medications, which help control the inflammation that sets off GI pain, are going to be the main course of treatment that your doctor suggests for the long haul of this chronic condition.
There is no secret treatment for inflammatory bowel disease. Everybodys looking for the secret pills. What diet can I follow? What supplement can I take? What probiotic can I take? Unfortunately, it just doesn’t exist, Dr. Schwimmer says. But the medicines we have work and they work better than anything else.
Thats why doctors who specialize in IBD caution that self-treatment with diet is not enough. If you arent working within the framework of a plan that includes proven, FDA-approved medication, you are at a higher risk of complications from your ulcerative colitis, including malnutrition.
Effects On Gut Microbiota
Table 4 details all changes in fecal bacteria abundance following the LFD intervention compared with the control diet. No differences were noted in the total species abundance or the total Bifidobacteria sp. in either trial where this was studied . Cox et al. showed no differences in the gene count, phyla distribution, α and β-diversity, nor in targeted Bifidobacteria including animalis, bifidum, breve, and pseudocatenulatum species. On the other hand, a reduction in the relative abundance of Bifidobacterium adolescentis, dentium, and longum was recorded in the LFD group compared with the controls . The Halmos and Cox RCTs were unable to reach a unanimous finding concerning the total Faecalibacterium prausnitzii abundance post LFD intervention. Finally, Halmos and associates suggested a reduction in the absolute and relative fecal content of Clostridium cluster XIVa, Akkermansia muciniphila, and the relative abundance of Ruminococcus torques following the LFD, and a lack of significant difference concerning Roseburia, Lactobacilli sp., Ruminococcus gnavus, and Clostridium cluster IV.
Also Check: Best Diet For Gerd And Ulcers
Studying This Diets Effect On Ibd
An initial study, conducted in London, involved the participation of patients with IBD who were in remission but had symptoms of IBS. It was found that the patients had all experienced improvements in their symptoms after following a low FODMAP diet. However, instead of testing this analysis further, the researchers aimed to determine whether high doses of FODMAPs aggravated their symptoms. Each patient received a three-day plan, including three various types of FODMAPS. It was found that one type of FODMAP in particular, known as fructans, was associated with more severe symptoms, including stomach pain, bloating, gas, and urgency. As a result, the researchers concluded that eliminating FODMAPS in patients with IBD could prove effective in alleviating symptoms and improving quality of life.
Low Fodmap Diet And Ibd
Evidence has been found to show that a low FODMAP diet helps to relieve symptoms of irritable bowel syndrome 1 but there is currently no evidence to suggest that it works for people with inflammatory bowel disease , although some people with IBD do find it helpful in controlling some of their symptoms.
References
Also Check: Low Dose Aspirin Ulcerative Colitis
Dairy Products To Eat And Skip
Cowâs milk, ice cream, yogurt, and many dairy foods have a FODMAP called lactose. Trade them for lactose-free versions or for almond milk. Hard cheeses like cheddar and aged cheeses like brie also are low in lactose. What about soy milk? Read the label. Skip those from whole or hulled beans. Look for brands made with soy protein, which are low in FODMAPs.
Are Food Triggers The Only Cause Of An Ulcerative Colitis Flare
Regardless of your diet, there may be times when your ulcerative colitis symptoms seem to disappear completely for months at a time before making a dramatic reappearance. When this happens, its .
But the foods youre eating arent the only possible culprit. Emotional stress, not taking medications as prescribed, and use of certain medications, like steroids and antibiotics, can also trigger ulcerative colitis flares, according to the Cleveland Clinic.
Flares take different forms for different people, and theres no formula that predicts what will bring them on. Different people will claim a medicine or anxiety will set their symptoms off. But some people just seem to have had flares when they have flares, and you can drive yourself crazy trying to find the cause, Dr. Schwimmer says.
Don’t Miss: Orange Juice And Ulcerative Colitis
Food Prep And Meal Planning
Although there is no cure for UC, meal planning and prepping food ahead of time can help people living with UC limit foods that trigger their symptoms.
Planning meals, snacks, and even your hydration efforts in advance gives you control over everything youll be consuming.
With preparation, you can avoid making quick decisions when youre hungry or thirsty that could result in a flare-up.
Taking the time to plan out your meals and read nutrition labels may take a couple of hours initially, but it can save tons of time throughout the week overall. Helpful steps include:
- buying ingredients in bulk
- cooking in batches
- preportioning your meals before storing them in the fridge or freezer, making them easier to reheat and eat
Not only will you have your meals prepared ahead of time, but youll also help limit food triggers, allowing you to feel better and be more productive overall. Buying and planning your snacks ahead of time is a good way to avoid reaching for trigger foods, too.
Additionally, because frequent diarrhea from UC can cause you to lose more fluid than you put into your body, planning water intake can help you avoid dehydration.
Constipation can be a symptom for some individuals, and their dietary needs may differ.
Fodmap Diet For Obesity
The Fodmap Diet for Obesity is a way of eating that is designed to help people with obesity control their food intake and their weight. The diet is based on the idea that foods that are high in FODMAPs can cause problems for people with obesity because these foods are difficult to digest.
The Fodmap Diet for Obesity is based on the idea that foods that are high in FODMAPs can cause problems for people with obesity because these foods are difficult to digest.
The Fodmap diet is a way of eating
Also Check: Best Probiotic For Ulcerative Colitis
Can A Low Fodmap Diet Help My Ibd
As a dietitian specializing in inflammatory bowel disease , one of the most popular questions patients ask me is Can a low FODMAP diet help my IBD?
The low FODMAP diet is an enticing option thanks to its rise in popularity and success in treating patients with irritable bowel syndrome . For many with IBS, a low FODMAP diet is an obvious choice. But its role in helping those with IBD is less clear.
Unlike IBS, IBD causes chronic and relapsing inflammation of the gastrointestinal tract. The two key types of IBD include Crohns disease and ulcerative colitis. For a thorough comparison of IBS vs IBD, read What If I Have Both IBS and IBD?.
Back to the question at hand: Can a low FODMAP diet help people with IBD?
Effect Of The Lfd In Qol
The Bodini, Cox, and Pedersen trials reported an improved QoL according to IBD-specific tools following the adoption of the LFD . Cox and colleagues additionally reported significant improvements, specifically in the Bowel II domain score of the IBD-Q. However, the QoL, as judged by IBS-related questionnaires , failed to improve according to Pedersen .
Recommended Reading: Can Ulcerative Colitis Cause Bad Breath
What To Eat As Your Symptoms Ease
As your symptoms improve, you can begin to add more fiber and variety to your diet to keep your gut healthy. Low FODMAP fruits and vegetables that are high in fiber include broccoli, cucumbers, squash, tomatoes, leafy greens, blueberries, strawberries, and kiwi fruit. Whole grains like high-fiber gluten-free breads and cereals can also boost your fiber intake. You should continue to avoid foods high in saturated fat , sugary beverages , and other processed foods, since research suggests that these foods can increase UC symptoms.
Fodmap Diet For Alzheimers Disease
FODMAPs are short-chain carbohydrates that are difficult for the body to digest. This can cause problems for people with Crohns disease, irritable bowel syndrome, or ulcerative colitis. FODMAPs can also be a problem for people with Alzheimers disease, as they can cause stomach pain and diarrhea.
The FODMAP diet is a way of managing these problems. Its based on the idea that people with Alzheimers disease are especially prone to problems with the gut, and that a low-FODMAP diet can help to improve symptoms.
To follow the FODMAP diet, youll need to keep a food diary. This will help you to see which foods are causing problems,
Recommended Reading: Different Stages Of Pressure Ulcers
Risk Of Bias And Quality Of The Rcts
The Cochrane Risk of Bias 2.0 tool was used to assess bias in the retrieved RCTs, with judgments falling in the categories of âlow risk of biasâ, âsome concernsâ, or âhigh risk of biasâ. Two independent researchers assessed RoB and a senior researcher intervened when an agreement was not reached. In parallel, the quality of the included studies was evaluated by two reviewers using the Oxford quality score .
Whats The Timeline Involved
The general idea behind the FODMAP diet is to avoid or reduce the consumption of foods high in FODMAP for around 3-8 weeks , in an attempt to assess which foods are not tolerated by the body. After the 3-8 weeks, small amounts can be reintroduced to reach a level that will be well-tolerated by the individual. For instance, fructose can be reintroduced the first week and if it does not trigger any symptoms, lactose can be reintroduced as well and so on.
Recommended Reading: Acupuncture For Ulcerative Colitis Treatment