Dairy Is A Common Trigger Food For People With Ulcerative Colitis
Lactose intolerance is a common issue affecting the general population, as well as people with ulcerative colitis, says Themistocles Dassopoulos, MD, the director of the Baylor Center for Inflammatory Bowel Disease in Dallas. Lactose intolerance prevents you from properly digesting lactose, the sugar found in milk and dairy products, because the small intestine lacks the digestive enzyme called lactase. While dairy doesnt seem to cause UC flares, lactose intolerance can cause symptoms such as abdominal pain and diarrhea that can be mistaken for UC. Avoid dairy products or add lactase supplements to reduce these symptoms.
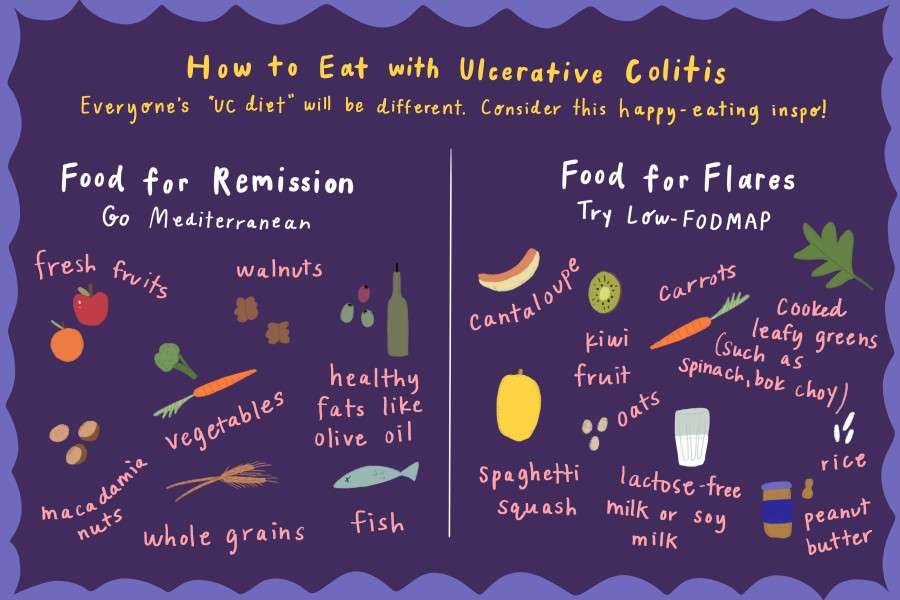
What Foods Should I Eat When My Ulcerative Colitis Is In Remission
You should try and maintain a diverse and nutrient-rich diet even when you are in remission and your symptoms have reduced or gone away completely. Keep a food diary and introduce new foods slowly, so you understand which ones trigger your symptoms. Keep well hydrated with water, broth, tomato juice, or rehydration solutions, and avoid making large changes in your diet without your doctors advice. Eat foods such as:
- Fiber-rich foods such as oat bran, beans, barley, nuts, and whole grains, unless your doctor has advised you to stick with a low fiber diet or you have an ostomy or intestinal narrowing
- Lean protein, which is found in fish, lean cuts of pork, chicken, soy, eggs, and firm tofu
- Fruits and vegetables of all colors remove the peel and the seeds if they trigger your symptoms
- Calcium-rich foods found in collard greens, yogurt, kefir, and milk
- Probiotic foods such as yogurt, kimchi, miso, sauerkraut, or tempeh.
What Foods Should I Not Eat If I Have Ulcerative Colitis
Again, each person who has ulcerative colitis will need to find their personalized diet. However, here are some of the most common types of foods that trigger ulcerative colitis:
Raw Green Vegetables
You should avoid foods that give you more stool. Foods that do this are most often foods with a lot of fiber.
Green or cruciferous vegetables contain a large amount of fiber, especially when they are raw. If you have ulcerative colitis, you should try to stick to fully cooked, skinless, and non-cruciferous vegetables.
Some examples of cruciferous vegetables are:
- Arugula
Read Also: How To Soothe Mouth Ulcers
Foods That May Help Avoid Flares
Some healthful foods may have anti-inflammatory effects that can help control the underlying inflammation of Crohns disease and ulcerative colitis. Many of these foods are unprocessed. They also tend to have lots of color. Some of the substances that give fruits and vegetables their color have anti-inflammatory and other healthful effects.
Eating this way helps support anti-inflammatory pathways in our bodies, which may be very helpful when managing an inflammatory disease like IBD. In addition, if you are not flaring, eating healthful foods will also help you avoid any deficiencies in vitamins, minerals, and other nutrients.
Dont Miss: What Is Best Medicine For Ulcer
What Should I Eat And Drink
Eat a high-calorie, high-protein diet. Strive for a balanced diet with foods from all food groups .
The food you eat should be based on what you like and what your body can handle.
Lactose intolerance is common in people with Crohns disease, but some people do not have issues when eating dairy products.
Try eating smaller, more frequent meals and snacks
If it is painful to eat or you are losing weight, try supplements like Boost, Ensure, and Breakfast Essentials .
Your fluid needs are increased with chronic diarrhea and acute flares. Drink more fluids during flares .
When your disease is active, a low-fiber, low-fat diet may reduce symptoms.
Also Check: What To Eat With Stomach Ulcer
Prep Your Meals In Advance
To stay on track, prepare everything in advance as much as possible.
If you don’t prepare beforehand, you’re more likely to make quick decisions when you’re hungry or thirsty that may lead to a flare-up.
You may have to spend a couple of hours planning your meals and reading nutrition labels, but you’ll save tons of time throughout the week.
The following tips can be helpful:
- Bulk-buying ingredients
- Batch cooking
- Preparing your meals in advance, then freezing or refrigerating them for easy reheating
Ulcerative colitis already requires much care and thought, and these steps will make food preparation easier.
At HealthierU, Dr. Donna Sergi uses Nutrition Response Testing and individualized nutrition therapy to help identify food triggers and keep you on track with good nutritional choices.
Contact us today to find out how we can help you combat ulcerative colitis symptoms.
Reintroducing Your Usual Diet
Your IBD team and dietitian will give you information about returning to your usual diet after youve finished enteral nutrition. They may suggest reintroducing foods slowly so you can see if any foods affect your symptoms and to help you feel more confident about eating again. There are three ways of doing this:
- the elimination diet after excluding all foods, they are reintroduced one by one every few days, to see if they cause problems
- the Royal Free method this is similar to the elimination diet but foods are reintroduced more quickly, over a period of days rather than weeks
- the LOFFLEX diet this excludes foods high in fat and fibre.
There isnt much evidence to show how well these diets work, or whether one works better than another. Your dietitian will explain the benefits and risks of all your options.
Ive found that you have to be very careful on the internet as there are many websites claiming to cure IBD through untested diets and supplements which are not properly regulated and could be harmful and also expensive.
Zaineb
This is an extreme form of low carbohydrate diet that limits:
Read Also: Ulcerative Colitis High Calorie Diet
Recommended Reading: Does Turmeric Help Ulcerative Colitis
Inflammatory Bowel Disease Management
Inflammatory bowel disease is not caused, nor can it be cured, by what you eat. Doctors and dietitians agree, however, that food may play some role in the underlying inflammatory process that causes IBD symptoms.
Certain foods may aggravate symptoms, while others may calm them and promote healing. Therefore, paying attention to what you eat and how your body responds to different foods is an important component of a total treatment plan for IBD.
A diet plan can supplement but should never replace medical treatment for IBD. Always take your medications exactly as prescribed by your doctor.
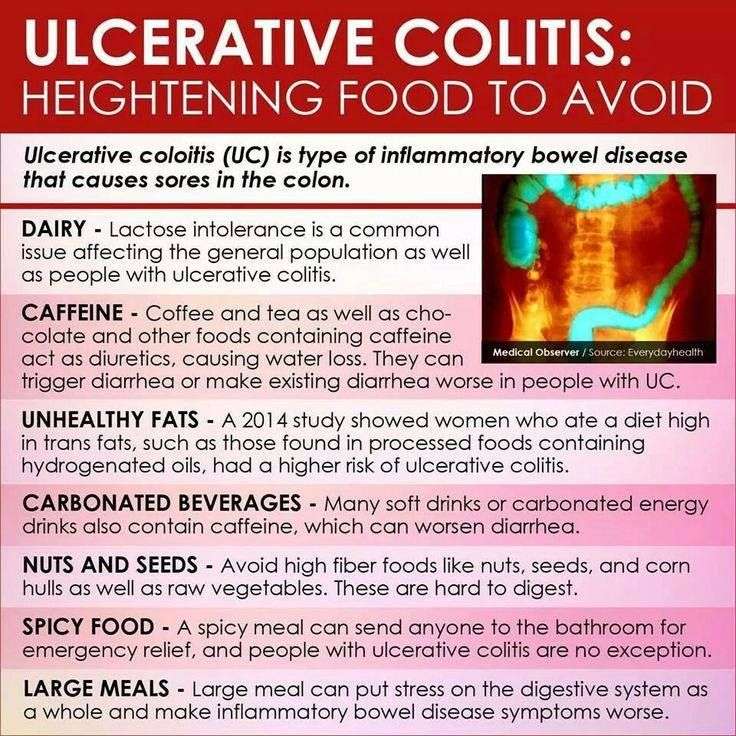
Foods To Avoid With Ulcerative Colitis
Although there are foods that are common triggers during both Ulcerative Colitis flares and remission, the list expands when youre experiencing active Ulcerative Colitis symptoms. Keep in mind that Ulcerative Colitis triggers differ from person to person, so the real key to long-term Ulcerative Colitis management is identifying what works for you. Easier said than done, right?
If youve ever searched on your own to figure out how to manage your Ulcerative Colitis, youve probably found a ton of information. The challenge is that the information on the internet can be contradicting and confusing. If youre struggling with Ulcerative Colitis, we recommend enlisting the help of a registered dietitian. They will be able to help you better understand your UC and determine what foods and behaviors most trigger your symptoms.
Remember to limit fiber when you are experiencing an Ulcerative Colitis flare. High fiber foods are part of a healthy, well-rounded diet. However, when UC symptoms are active, you may need to temporarily limit fiber intake to reduce inflammation and allow your gut to heal. High fiber foods are harder to digest and can trigger UC symptoms. High fiber foods include whole grains, fruits with skin and seeds, vegetables with skin and seeds, raw vegetables, cruciferous vegetables, nuts, seeds, beans and legumes.
Read Also:History Of Ulcerative Colitis Icd 10
You May Like: How To Tell If You Have A Stomach Ulcer
Quick Tips For Nausea
If youre really having trouble keeping things down, here are a few of my tips:
- Be cautious about how much volume youre putting in and what ingredients you may be substituting. If you’re you’re questioning if you’ll be able to keep it down at the rate that its dissolving, or wondering if it may just come right back up and leave you back to where you started … consider this.
- I’ve heard of others using cupcake wrappers to poke through and hold the contents that melt if not consumed quickly enough. Cool, huh? But, eating faster doesn’t mean better if you’re vomiting. If you find this to be true, consider putting less in each cube.
- Major nausea hack: In the past, I’ve taken a couple of tablespoons of the purée and placed pureed contents into one corner of a few small Ziploc bags. Freeze that, then cut off a very small tip of the corner of the bag, so when you’re ready to eat one, you can consume it at a slower rate.
Tips For Managing Ulcerative Colitis Symptoms
- Consult your healthcare provider or dietitian before making any changes to your diet
- Eat a well-balanced nutrient rich diet
- Eat more frequently. Eat five to six smaller meals over the course of a day
- Stay hydrated by drinking water and fluids with salt – like broth, tomato juice or rehydration solutions
- Drink slowly and avoid using a straw because these may cause gas due to taking in air
- Use a food diary to record the foods you eat and how these impact your symptoms
- Avoid your specific trigger foods
- Use simple cooking methods – boil, steam, grill, poach, broil or saute
Recommended Reading: How Do You Get Rid Of Stomach Ulcers
Fight Anemia And Fatigue With Iron
Flares wear you out. One reason can be anemia, when your body doesn’t have enough healthy red blood cells. If you have long-term, low-level bleeding from your colonâs lining or bloody diarrhea, you may get iron deficiency anemia and need iron supplements. Food sources include lean meats, seafood, spinach, raisins, and fortified breakfast cereals. Egg yolks and artichokes are other options that may be easier on your stomach.
3
Food Prep And Meal Planning

Although there is no cure for UC, meal planning and prepping food ahead of time can help people living with UC limit foods that trigger their symptoms.
Planning meals, snacks, and even your hydration efforts in advance gives you control over everything youll be consuming.
With preparation, you can avoid making quick decisions when youre hungry or thirsty that could result in a flare-up.
Taking the time to plan out your meals and read nutrition labels may take a couple of hours initially, but it can save tons of time throughout the week overall. Helpful steps include:
- buying ingredients in bulk
- cooking in batches
- preportioning your meals before storing them in the fridge or freezer, making them easier to reheat and eat
Not only will you have your meals prepared ahead of time, but youll also help limit food triggers, allowing you to feel better and be more productive overall. Buying and planning your snacks ahead of time is a good way to avoid reaching for trigger foods, too.
Additionally, because frequent diarrhea from UC can cause you to lose more fluid than you put into your body, planning water intake can help you avoid dehydration.
Constipation can be a symptom for some individuals, and their dietary needs may differ.
Don’t Miss: Ulcerative Colitis Probiotics Vsl 3
Directions For Ice Pops
What Advice Is There For When I Have No Active Disease
When you are in remission then it is essential to make sure you are well nourished and regain any lost weight you may have experienced during a flare. Good nutritional status also helps to prevent vitamin and mineral deficiency and infection, and maintain disease remission.
- Base meals on higher fibre starchy foods like potatoes, bread, rice or pasta.
- Have some dairy or dairy alternatives .
- Eat some beans, pulses, fish, eggs, meat and other protein.
- Choose unsaturated oils and spreads, and eat them in small amounts.
- Drink plenty of fluids .
You May Like: Antibiotics And Antiseptics For Venous Leg Ulcers
Nutrition Tips For Inflammatory Bowel Disease
Inflammatory Bowel Disease is a term used for two specific and separate diseases: Crohn’s disease and ulcerative colitis. Nutritional recommendations are different for each disease and for each individual patient. It is important to discuss the treatments that are right for you with a registered dietitian and with your doctor.
When Ibd Is Active It May Help To:
-
Limit dairy that is high in lactose.
-
You might be able to handle yogurt with live active cultures or Greek-style yogurts.
-
You might be able to handle hard cheeses like cheddar and Swiss.
-
Try almond or coconut milk, lactose free milk or use lactase pills.
Limit fructose.
High amounts are found in fruit juice, soda, honey, and dried fruit.
Limit sorbitol .
Limit high fat foods like butter, cream, red meats, chocolate, fried or fast foods.
Limit high fiber foods like whole grains, beans, and fruits and vegetables with skin.
You might be able to handle fruits and vegetable with skins peeled off.
Lower fiber fruits include cantaloupe, honey dew, mandarin oranges, fruit cocktail, and applesauce. For veggies, try zucchini, yellow squash, and bell peppers.
Try well cooked vegetables and vegetable juice.
Try low fiber grain products like white bread, white rice and pasta and low fiber cereal and crackers.
Caffeine, acidic foods, and alcohol may make flares worse.
It may help to keep a food log. Your dietitian can review your food log with you and help figure out food triggers as well as foods that may improve your symptoms.
Recommended Reading: What To Eat To Help Stomach Ulcers
Ulcerative Colitis Foods To Avoid
Now that we have looked at foods good for ulcerative colitis, well outline foods to avoid with ulcerative colitis. If you have received a diagnosis recently, you will likely find the list below helpful:
When you suffer from ulcerative colitis, you can feel desperate for relief, and it can be easy to get caught up in fad diets that claim to cure ulcerative colitis. Diet does not cure this inflammatory bowel condition but dietary changes can reduce symptoms. To find the best diet for your individual situation, it is best to talk to your gastroenterologist and a nutritionist who is familiar with UC. Again, there may not be a diet cure, but what you eat can make a big difference in your comfort level as you live with this chronic disease.
Also read:
Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
Don’t Miss: Does Aleve Cause Stomach Ulcers
Eating When You Are In Remission
While theres no cure for UC, you may experience periods of remission. During this time, youll be symptom-free and your UC wont interfere with your daily life.
Theres no definitive way to avoid flare-ups forever, but you can prolong your remission periods by maintaining a diverse and nutrient-rich diet that does not include trigger foods.
To stay symptom-free, it may be helpful to follow one of the diets that other individuals with UC find successful, as well as introduce new foods slowly and stay hydrated.
However, its important to consult with your doctor or dietician before making any changes to your diet.
Some foods that may help keep you feeling good and hydrated during remission
What Should I Eat
Its not always easy knowing what foods best fuel your body, especially when you have Crohn’s disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, the symptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.
Also Check: Booties To Prevent Pressure Ulcers
Managing Ulcerative Colitis With Diet
Dietary changes are among the best ways to control ulcerative colitis. The food you eat can affect the tissue inside your digestive system and trigger inflammation. Avoid trigger foods and replace them with foods that are easier to digest to reduce the chances of a flare-up.
Foods that are less likely to trigger ulcerative colitis symptoms
Foods that are generally easily tolerated include:
- Lean protein .
- Refined grains .
- Cooked vegetables if they are skinless and seedless.
- Calcium-rich foods such as yogurt, collard greens, certain dairy products.
- Food with probiotics such as kimchi, miso, and sauerkraut.
Foods more like to trigger ulcerative colitis symptoms
Foods that are more likely to cause a flare-up of symptoms include:
- Insoluble fiber .
- Lactose .