What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
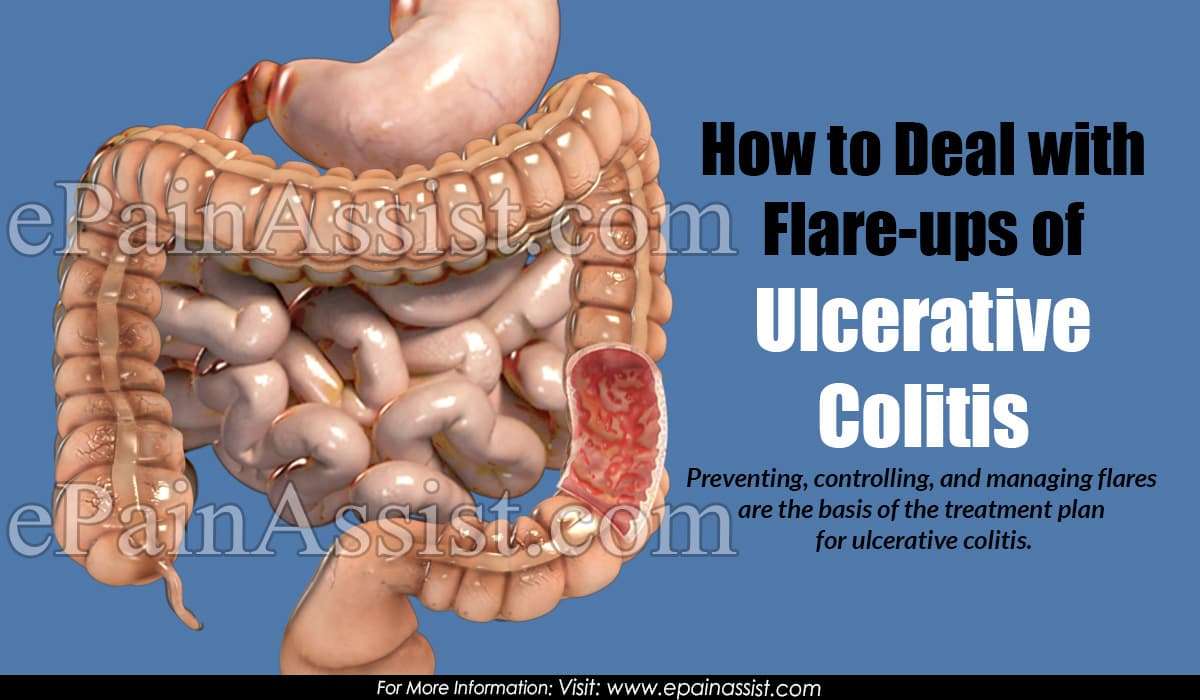
Tips To Control Your Ulcerative Colitis Flares
You want to calm the flares that strike when you have ulcerative colitis . And if you keep your disease in check, you may also have fewer symptoms over time.
Your flares might be different from someone else’s. Symptoms can range from mild to severe and are often unpredictable. You might get diarrhea and feel an urgent need to go to the bathroom. You could have blood in your stool and be tired a lot.
Use these five tips to keep your flares in check.
What Are Ulcerative Colitis Treatment Options
Depending on the location and severity of your case of ulcerative colitis, there are different treatments that can help you feel better. For a long time, corticosteroids were the main form of medical treatment for IBD, but they can potentially have adverse effects when used long-term. With more research, options like immunosuppressants arrived. According to the Centers for Disease Control and Prevention , the newest type of medication approved for the treatment of IBD is biologics. These medications are made from living thingsrather than chemical compoundsand work to target proteins made by the immune system to reduce inflammation. If medication isnt effective, surgery is also an option.
Dr. Sinha emphasizes that keeping your health care team informed is key to managing ulcerative colitis. Having this regular communication helps facilitate labs, imaging, or endoscopy that may be necessary, he says. It also allows the providers to understand many other facets of the disease’s impact on the patient, such as the psychosocial impact.
Don’t Miss: Corneal Ulcer Dog Home Remedy
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Also Check: What Foods To Eat With A Peptic Ulcer
The Ability To Differentiate Gas From Liquid Or Solid In The Rectum When Urgency Occurs
Participants can be greatly affected by a loss of the ability to differentiate rectal urgency due to gas from rectal urgency due to stool, mucus, or blood. They usually lose this ability during a flare, and need to go to the toilet anytime they have urgency, to avoid the risk of incontinence.
If I do have gas, I dont dare let it pass because all sorts of other stuff could come with it.
When Im having a flare, I cant tell if its gas or not. Gas can carry some other stuff with it. When theres a flareup, I think gas counts because theres no such thing as just gas.
Read Also: Do You Still Have Ulcerative Colitis After Colectomy
Symptoms Of Ulcerative Colitis
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience extreme tiredness , loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is.
For some people, the condition has a significant impact on their everyday lives.
I Take Medication Regularly Can A Flare
Unfortunately, yes. Ulcerative colitis is a chronic condition. Medications and lifestyle changes can help reduce the intensity and frequency of ulcerative colitis flare-ups, but not stop them completely.
Regular flare-ups may indicate a problem with your current treatment. If you are taking your medications as prescribed and still experiencing flare-ups, you should contact your physician who may adjust your medication or suggest other treatment options.
Recommended Reading: Side Effects Of Ulcerative Colitis
Your Uc Flare Management Plan
Your doctor may help you deal with a flare by changing your medications or offering new ones. Treatment of flares can include mesalamine products and usually a steroid, such as prednisone, says Desi.
There are also some things you can do at home to temper a flare. These include:
During an ulcerative colitis flare, its recommended that you schedule regular visits to see your doctor, at least once every three months until the symptoms go away. After the flare has subsided, physicians recommend one or two checkups a year to manage the disease.
When an ulcerative colitis flare strikes, you have options for getting your life back on track. Its important to learn what you can about maintaining your health and work with your doctor to find the best ways to safely control UC. And remember to always let your doctor know when new or persistent symptoms arise.
Correlation Between Disease Activity And Endoscopic Findings
There was a consensus that endoscopic findings would usually affirm patients own assessment of their level of disease activity.
Testing has always been pretty much a confirmation of how Im feeling at the time.
The colonoscopy reports and photos are basically, well, heres what this looks like and this looks like and heres the issue. So, theyre pretty in synch.
You May Like: Vsl 3 And Ulcerative Colitis
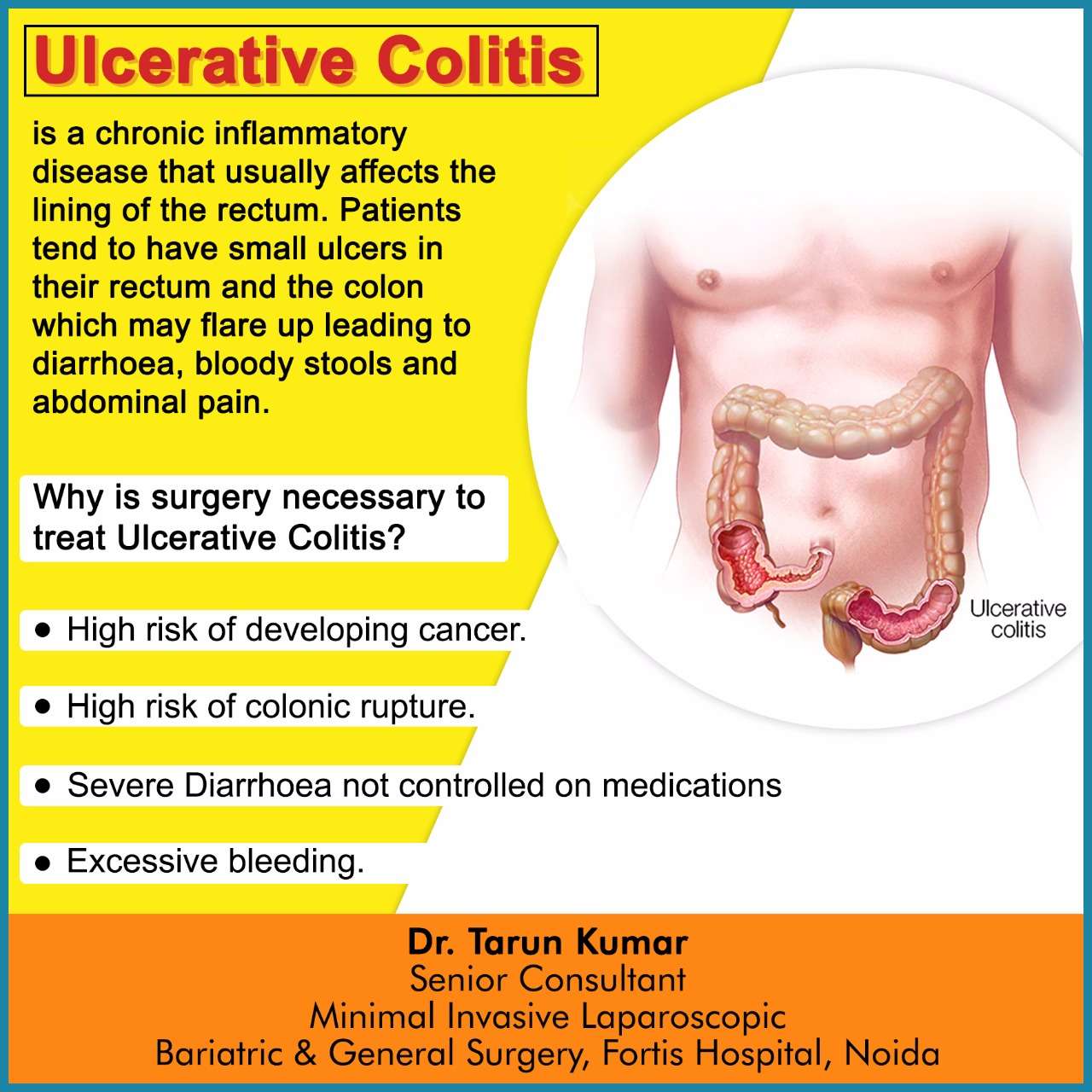
What Causes Ulcerative Colitis
Ulcerative colitis is thought to be an autoimmune condition.
This means the immune system, the body’s defence against infection, goes wrong and attacks healthy tissue.
The most popular theory is that the immune system mistakes harmless bacteria inside the colon for a threat and attacks the tissues of the colon, causing it to become inflamed.
Exactly what causes the immune system to behave in this way is unclear.
Most experts think it’s a combination of genetic and environmental factors.
How Do You Calm A Colitis Flare Up
You May Like: How Do You Cure Ulcerative Colitis
Whats The Difference Between Ulcerative Colitis Vs Crohns Disease
The list of symptoms for ulcerative colitis and Crohns disease are very similar, including diarrhea, abdominal pain, and rectal bleeding. The biggest difference can be found in the location of the active inflammation. Since Crohns can appear anywhere in the gastrointestinal tract, you might see things like inflammation of the small bowel that you wouldnt see with ulcerative colitis. Another difference is that Crohns doesnt stop at the intestine lining. It can actually affect the entire thickness of the bowel wall.6
Southern Cross Medical Library
The purpose of the Southern Cross Medical Library is to provide information of a general nature to help you better understand certain medical conditions. Always seek specific medical advice for treatment appropriate to you. This information is not intended to relate specifically to insurance or healthcare services provided by Southern Cross. For more articles go to the Medical Library index page.
Read Also: Is Ginger Tea Good For Ulcerative Colitis
Why Working With A Qualified Care Team Is So Important When It Comes To Managing Ulcerative Colitis
People being treated for UC typically arent getting dietary or lifestyle advice, which is a huge disservice, says Cohen. But managing ulcerative colitis and preventing flare-ups can be done! You just might need a little help from the experts.
Because UC isnt one-size-fits-all and triggers are highly individual, enlisting the help of a care team like the clinicians at Parsley Health is wise. Providers can provide individualized supplement protocols based on lab testing, customized eating plans for periods of remission and flares, and communicate with your current GI doctor if necessary to streamline care.
Dont Miss: How To Check A Horse For Ulcers
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Don’t Miss: Is Colitis And Ulcerative Colitis The Same Thing
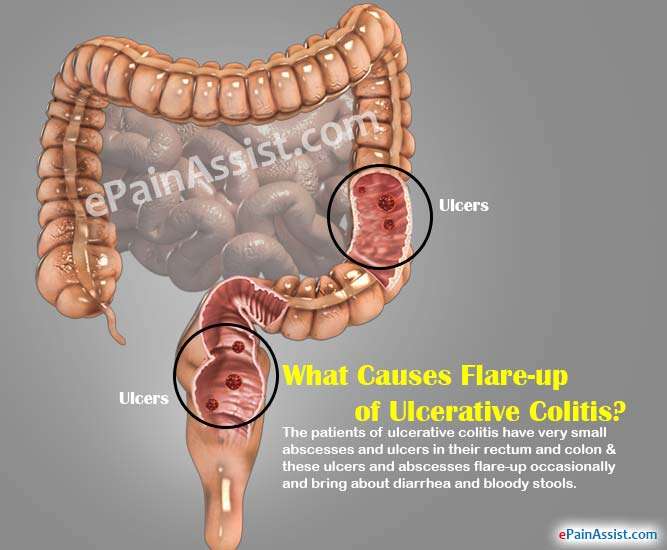
Diarrhea And Rectal Bleeding
People with ulcerative colitis often experience watery diarrhea as well as frequent and sudden urges to have a bowel movement. For some people, the urge to have a bowel movement may occur so suddenly that it significantly disrupts their daily life. Some people need to have a bowel movement more than 10 times per day.
You may notice blood, pus, or mucus in your stools. You may also experience rectal bleeding if youre having a flare-up. Blood comes from ulcers along the surface of your rectum.
If you have uncontrollable diarrhea or notice blood in your stool, you should see a doctor. Diarrhea caused by ulcerative colitis can lead to medical emergencies like severe dehydration, a perforated colon, or .
What Is Ulcerative Colitis Exactly
Ulcerative colitis is one of the two main forms of inflammatory bowel disease . The other is Crohns disease. U.C. occurs when the immune system malfunctions, causing inflammation and ulcers to appear on the inner lining of the large intestine, according to the National Institute of Diabetes and Digestive and Kidney Diseases . Its not comfortable, to put it mildly, and not something that will clear up quickly.
Ulcerative colitis is a chronic illness that does not yet have a medical cure. That doesnt mean nothing can be done though, so dont despair if youre experiencing symptoms. Sidhartha Sinha, M.D., a gastroenterologist, assistant professor at Stanford Medicine, and researcher who specializes in IBD, tells SELF that while there arent medical cures for ulcerative colitis, there are medical treatments. And we have made great advancements in these treatments, he says. The last resort is a surgical option called colectomythe removal of the entire colonwhich can eliminate U.C. entirely.
Read Also: What Is The First Sign Of Stomach Ulcer
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
What Triggers Flare
Many different factors can play a role in bringing on symptoms of a flare. Even if you have been avoiding potential triggers, you can still experience a flare.
However, being familiar with common causes and your triggers can help reduce and manage flare-ups. Common causes include:
- Medication changes: If you miss, skip, or take the wrong dose of your medication, it can trigger a flare. If you take your medication as prescribed but still experience a flare, you may need a change. Talk with your healthcare professional about possible changes in the dose, frequency, or type of medication to help improve your symptoms.
- Nonsteroidal anti-inflammatory drugs : Medications such as aspirin, ibuprofen, and naproxen could worsen symptoms and should generally be avoided.
- Antibiotics: Sometimes antibiotics can trigger a flare due to changes in your gut bacteria. If you experience a flare-up while taking antibiotics, talk with your healthcare professional.
- Smoking: Smoking cigarettes can increase the risk of flares. Additionally, extended exposure to secondhand smoke may also trigger a flare.
- Stress: Stress can worsen your symptoms during a flare-up.
- Diet: During a flare-up, certain foods can make your symptoms worse. Which foods are triggers will vary from person to person. Keeping a food diary during times of a flare can help you identify your food and beverage triggers.
Also Check: Ulcerated Nodular Basal Cell Carcinoma
What To Look For
The key is to pay attention to your specific symptoms. The more you’re aware of them, the better able you are to spot changes.
And there are lots of ways your symptoms can change. You might get new ones. Or the ones you have may get worse, last longer, or come on more often.
Usually, a flare-up brings at least:
- An urgent need to poop
- Blood or mucus in your stool
- Cramps in your lower belly
If it spreads to more areas of the colon, everything gets more intense. You have more diarrhea. Cramps get more severe. You have more mucus, pus, and blood in your stool. Pain in your belly gets worse and more widespread, especially up the left side. It can also affect your desire to eat and cause you to lose weight.
And some of those symptoms may just be signs of a stronger flare-up. You’ll need to see your doctor to find out for sure. Read more on ulcerative colitis symptoms to look for.
Diet Tips During A Flare
A modified diet may help you manage and reduce your UC symptoms. Depending on the person, specific foods may trigger flare-ups or worsen symptoms. As a result, its important to identify and limit these foods.
Your doctor and a dietitian can work with you to find a diet that best manages your symptoms while providing the nutrition you need.
You May Like: Best Prebiotic For Ulcerative Colitis
How Are Causes And Risk Factors The Same And Different
Doctors arenât sure what causes you to get UC or diverticulitis, but the two conditions have some common risk factors:
- Age. Your odds for either condition go up as you get older.
- Race. White people are more likely than those of any other race to have UC or diverticulitis.
UC might be caused by an abnormal immune response in your body. This means that if your immune system is fighting off a virus or bacteria, it may mistakenly attack cells in your digestive tract, too.
Genes might also play a role. If a close relative like your parent or sibling has UC, youâre more likely to have it, too. If youre of Ashkenazi Jewish descent , your risk is even higher. Diet and stress donât cause UC, but they may trigger your symptoms and cause flare-ups.
As for what causes diverticulitis, experts believe bacteria found in your poop might get pushed into the bulging sacs as it passes through the colon. This causes the sacs to become infected or inflamed. Another theory is that your poop, especially if youâre constipated, might put a lot of pressure against the colon walls as it passes through. This can cause tears in the sacs and increase your chances of an infection.
Other risk factors for diverticulitis include:
- Diet low in fiber and high in animal fat
- Certain medications
Dont Miss: Hospital Acquired Pressure Ulcers Reimbursement