Skin Disorders Associated With Ulcerative Colitis
Below are six skin conditions that people with ulcerative colitis can be at increased risk of developing.
1. Erythema Nodosum The most common skin condition associated with ulcerative colitis, erythema nodosum is a rash that consists of painful, raised bumps and is usually found on the legs.
It tends to develop when ulcerative colitis is active, notes Dr. Hagan. You may also run a fever, have joint pain, and generally feel ill, according to Medline Plus.
Treatment options include pain-relieving medication, steroids , and a potassium iodide solution to clear up the bumps.
A cool compress can also help alleviate discomfort and reduce inflammation, says Kally Papantoniou, MD, a dermatologist in private practice in Melville, New York. She also recommends elevating your legs to help lessen swelling and tenderness.
Compression stockings can also be helpful, but have your doctor evaluate you for vascular disease before using them, cautions Dr. Papantoniou.
Symptoms of erythema nodosum usually go away within three to six weeks, but the residual bruises may last for months. In about 20 percent of cases, the rash comes back.
2. Pyoderma Gangrenosum This is a severe and debilitating condition that starts as a rash made of red or purple bumps or blisters, and then quickly spreads. These blisters eventually join together and form deep open sores , according to the Crohn’s& Colitis Foundation.
Pyostomatitis vegetans is the same condition, but it occurs in the mouth, Brieva says.
Retrograde Labeling Of Bladder Afferent Neurons
Bladder afferent neurons were specifically labeled by conventional neuronal tracing dye Fast Blue in live animals through surgery as described previously . Briefly, the rat urinary bladder was exposed with a lower abdominal incision under anesthesia . FB was injected into 10 sites in the muscular wall of the bladder to label bladder afferent neurons in the DRG. Sterilized Hamilton syringe was used for injection. To prevent leakage and labeling of adjacent tissues, a cotton swab was used, close to the injection site, to wipe off any excess dye that might leak during needle withdrawal after each injection. We also avoided to inject dyes into the lumen, major blood vessels, or overlying fascial layers. The incision was closed with 40 sutures. The surgeries were done 7 days prior to harvest of tissues. We also checked the leakage of the dyes by examining the bladder and surrounding tissues after euthanasia of the rats. No contamination was found.
Read Also: Medihoney For Stage 1 Pressure Ulcer
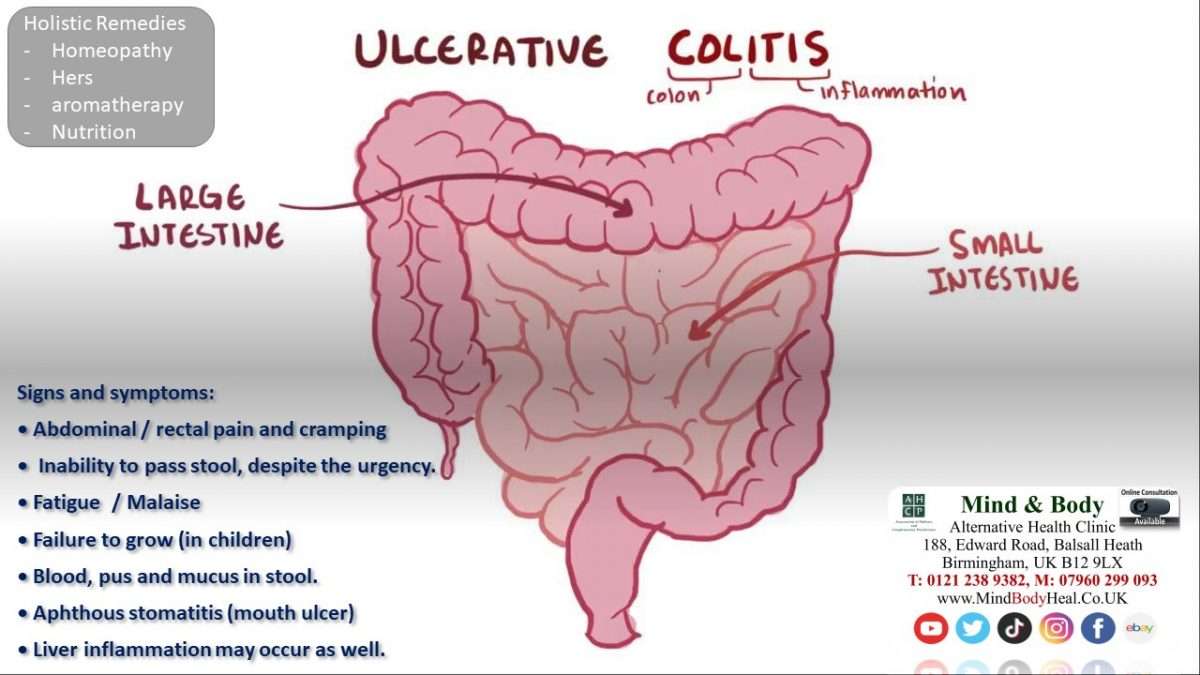
Inflammatory Bowel Disease And Colitis
Ulcerative colitis and Crohnâs disease are the two types of inflammatory bowel disease that cause colitis. Crohnâs disease and ulcerative colitis are considered autoimmune diseases .
- Ulcerative colitis always begins in the rectum and may spread to the rest of the rest of the colon, spreading from the rectum to the sigmoid, descending, transverse, and finally the ascending colon and cecum in that order. Ulcerative colitis is considered an autoimmune disease, and symptoms include abdominal pain, and bloody, diarrheal bowel movements.
- Crohnâs disease may occur anywhere in the gastrointestinal tract , including the esophagus, stomach, small intestine, and colon. In Crohnâs disease, there may be âskip lesions,â that is, abnormal segments of the GI tract interspersed with normal segments.
Both Crohnâs disease and ulcerative colitis may have other organ systems involved in addition to the gastrointestinal tract.
Either collagen or lymphocytes infiltrate into the layers of the wall of the colon, presumably as a result of inflammation. This is an uncommon illness and maybe an autoimmune disease. Diarrhea often is watery, and no blood is present in the stool.
Also Check: Can Ulcers Cause Black Stool
When To Contact A Doctor
People need to discuss any blood in the stools with their doctor, even if they have experienced it before.
A person may also wish to monitor their UC symptoms, so they know what is usual for them to experience. People can then discuss any abnormal symptoms with a healthcare professional.
If individuals have ongoing diarrhea that lasts for a couple of weeks, they can contact their doctor to discuss concerns and treatment.
The Crohnâs and Colitis Foundation advises people to seek emergency medical attention if they experience any of the following:
- inability to keep down liquids due to nausea, vomiting, or pain
- rectal bleeding with blood clots in stools
- continuous pain
Managing UC with treatment may help reduce bleeding. There are medications that may reduce inflammation in the rectum and large intestines, which may, in turn, reduce bleeding.
Anti-inflammatory medications for UC can include:
- 5-Aminosalicylic acid: Medication that may help reduce acute inflammation and causes inflammation to become inactive over time.
- Corticosteroids: A short-term treatment to help reduce inflammation.
- Immunosuppressants: These medications can help suppress the immune response that can cause inflammation. However, they may take up to 6 months to be effective.
- Biologics: For treatment of moderate to severe UC, biologics help block molecules that trigger inflammation.
Read Also: Early Stage Venous Leg Ulcer
Does Drinking Water Help Uc
Its important to drink water when you have UC. Having enough fluids will replenish what you lose through diarrhea.
Water alone may not be enough. Your body also loses electrolytes like salt, potassium, and magnesium when you have diarrhea.
Drinking water plus electrolytes can help you stay hydrated. You can find that combination in the form of an oral rehydration solution at your local pharmacy. Sports drinks such as Gatorade and Powerade also contain electrolytes and fluid.
Read Also: How To Get Rid Of Corneal Ulcer
Recommended Reading: Can Stress Cause Flare Up Ulcerative Colitis
Acne And Ulcerative Colitis
Introduction:
My 18 year old son was diagnosed with UC this year having had had sudden onset colitis after a holiday with his friends. I am interested to know if Ulcerative Colitis is related to allergies and systemic inflammation. He has always suffered from hay fever since he was a young child. I am considering his trying homeopathy for his hay fever and acne.
What To Do During A Flare
Most skin issues associated with UC are best treated by managing the UC as much as possible, as many of these rashes can coincide with UC flare-ups. Others may be the first sign of UC in someone who hasnt been diagnosed yet.
Corticosteroids can help with the inflammation that often causes the skin issues associated with UC. Eating a well-balanced diet can help promote overall health and may aid in preventing skin issues.
When you do experience a flare-up of UC skin rash, there are several things you can try:
- Keep the lesion clean to prevent infections.
- See your doctor for prescription antibiotic ointment or pain medication if needed.
- Keep
Don’t Miss: How To Treat A Diabetic Ulcer
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Read Also: Best Vitamins For Ulcerative Colitis
A Connection Between Acne And Ibd
A review done in 2011 speculated that there could actually be a connection between acne and IBD. Severe acne and IBD are both inflammatory conditions, and both are often diagnosed in adolescents and young adults. The authors went on to point out that if a young person is under the regular care of a physician, other conditions may be identified.
Read Also: How To Treat A Leg Ulcer At Home
Bladder Symptoms And Ibs
IBS is a group of symptoms, notably abdominal pain and changes in bowel habits. The condition doesnt damage your digestive system, but it often affects your quality of life.
IBS doesnt cause urinary problems directly. But many of the same triggers for IBS, including stress and infection, are believed to play a role in urinary problems.
The bladder symptoms often experienced by people with IBS include:
- Frequent urination
- Incomplete emptying of the bladder
- Nocturia
- Urinary urgency
Women with IBS may be more likely to experience urinary incontinence and overactive bladder than women without IBS.
A 2012 study from Asahikawa Medical University in Japan reported that 33.3% of people who had IBS had overactive bladder as well. Women were affected slightly more frequently than men.
It isnt known for sure why people who have IBS are at higher risk for urinary problems and vice versa. Sometimes improving one of the two problems may lead to an improvement in the other.
Since the bladder and bowel are close together, there could be interaction between some of the nerves and muscles.
Other possible reasons could be inflammation around the bladder and bowel, or a nervous system issue affecting the whole region.
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Also Check: Service Dog For Ulcerative Colitis
Differential Diagnosis Investigations And Treatment
On physical examination, the skin manifestation mainly involved the thorax region and the back.
Laboratory investigation showed no significant alterations except for a mild increase in fibrinogen and CRP levels. On March 2014, the patient underwent colonoscopy showing mucosal edema/erythema with diffuse erosions . In view of the steroiddependent UC and the unsatisfactory response to conventional therapy , he started therapy with adalimumab .
On the basis of the findings of comedones, papules, and, especially, pustules, the possibility of an AP was considered and the diagnosis of acne was fairly easy. However, we considered in differential diagnosis: rosacea, other dermatitis, flat warts, which were excluded by an expert dermatologist.
Living With Ulcerative Colitis And Kidney Disease
If you are living with UC and kidney disease, it is important to maintain a healthy lifestyle. Many MyCrohnsAndColitisTeam members have shared their tips on how they live with UC and kidney disease. I have regular appointments with my urologist/kidney specialist to check my blood and urine, one member noted. Another said, I exercise and stay at a good weight, while a third member wrote, I try to get enough potassium and vitamin D in my diet.
Other ways to manage UC and kidney disease include:
- Maintaining a healthy, well-balanced diet
Also Check: Can I Eat Eggs With Ulcerative Colitis
What Research Is Being Done Regarding Ulcerative Colitis
Active research is also ongoing to find other biological agents that are potentially more effective with fewer side effects in treating ulcerative colitis including adalimumab, visilizumab, and alpha-4 integrin blockers.
Research in ulcerative colitis is very active, and many questions remain to be answered. The cause, mechanism of inflammation, and optimal treatments have yet to be defined. Researchers have recently identified genetic differences among patients which may allow them to select certain subgroups of patients with ulcerative colitis who may respond differently to medications. Newer and safer medications are being developed. Improvements in surgical procedures to make them safer and more effective continue to emerge.
Health Maintenance
It is recommended that adults with inflammatory bowel disease generally follow the same vaccination schedules as the general population.
Osteoporosis has also increasingly been recognized as a significant health problem in patients with IBD. IBD patients tend to have markedly reduced bone mineral densities. Screening with a bone density study is recommended in:
- postmenopausal woman,
How Severe Can Acne Get
Dermatologists rank acne by severity:
- Grade 1 : mostly whiteheads and blackheads, with a few papules and pustules.
- Grade 2 : multiple papules and pustules, mostly on your face.
- Grade 3 : numerous papules and pustules, along with occasionally inflamed nodules. Your back and chest may also be affected.
- Grade 4 : numerous large, painful and inflamed pustules and nodules.
Don’t Miss: How Do You Check For A Stomach Ulcer
How Are Skin Rashes Treated
Skin complications for people with ulcerative colitis are often improved by treating UC flare-ups as they come. One study found that symptoms of erythema nodosum in particular decreased if the underlying UC condition improved.
Many ulcerative colitis skin problems respond well to topical or oral steroids. Sweets syndrome and mild cases of pyoderma gangrenosum are often initially treated with oral or topical corticosteroids. Mouth ulcers can also be treated with topical steroid agents.
If the conditions do not respond to those medications, Humira is often the second treatment of choice. Unfortunately, one of the side effects of Humira is a rash.
Have you experienced skin rashes as a part of ulcerative colitis? Do you have any tips for dealing with them? Comment below or start a new conversation on MyCrohnsandColitisTeam.
Uc Treatments And Urinary Changes
Sometimes, UC treatments can affect urinary habits. Corticosteroids such as prednisolone may cause urinary changes in people with UC. This medication usually causes someone to pee less, but it can also cause someone to pee more often.
Several members have noticed this effect. Has anybody ever experienced frequent, urgent urination whilst on prednisolone? asked one member. I am definitely peeing more often, but the urgency at which I need to get to the bathroom to have a pee is a bit worrying. Another member mentioned that they had experienced this effect. When I take prednisone or budesonide, I urinate much more frequently, which is a known side effect of steroids.
Using high doses of steroids or using steroids for a long time can sometimes lead to problems with the adrenal glands small organs that make hormones to regulate many body processes. Frequent urination can be a sign of this issue. Other symptoms include dizziness, a fast heart rate, irregular heartbeats, blurry vision, or feelings of weakness. Tell your doctor if you notice these symptoms while taking steroids.
Several other health conditions unrelated to UC could also lead to increased urination. They include:
- Bladder stones
Also Check: Easy To Digest Foods For Ulcerative Colitis
Don’t Miss: Does Turmeric Help Ulcerative Colitis
More Evidence Ties Acne Drug To Bowel Disease
4 Min Read
NEW YORK – Adding to evidence that the acne drug isotretinoin may lead to bowel disease in some users, a new study finds that patients on the medication were four times more likely than non-users to develop ulcerative colitis within a year.
Reporting in the American Journal of Gastroenterology, researchers say that the risk of any one isotretinoin user developing ulcerative colitis is likely quite small.
However, the findings do strengthen the evidence of a cause-and-effect relationship between the acne drug and inflammatory bowel disease — a group of digestive disorders that includes ulcerative colitis and Crohns disease.
Isotretinoin, which is used to treat severe acne, is probably best known by the brand-name Accutane. That drug was taken off the market last year in the face of competition from generic alternatives — though in pulling the medication, maker Roche Pharmaceuticals also cited costs from defending personal-injury lawsuits.
Earlier this year, the company was ordered to pay $25 million in damages to a former Accutane user who claimed that the drug caused his IBD.
The company has maintained that there is no strong evidence that the acne drug triggers IBD. Between 1997 and 2002, 83 cases of IBD among isotretinoin users were reported to the U.S. Food and Drug Administration, but that does not prove that the drug itself is to blame.
SOURCE: here 4a.html American Journal of Gastroenterology, online March 30, 2010.
What Imaging Tests And Procedures Diagnose Colitis
Colonoscopy: The length of the colon can be directly viewed by colonoscopy. A gastroenterologist uses a thin, flexible tube equipped with a fiberoptic camera to view the inside lining of the colon. The appearance of the colonic lining often allows the doctor to make the diagnosis and also provides the opportunity to look for tumors and polyps. Biopsies can be obtained from the mucosal lining during colonoscopy and evaluated under the microscope by a pathologist to determine the cause of colitis. A biopsy is the only way to diagnose microscopic colitis.
Computerized tomography and barium enema are tests that are sometimes ordered to help diagnose the potential cause of colitis. CT scan of the abdomen has become a more common test to evaluate patients with abdominal pain. However, it is important for the health care professional to balance the risk of radiation with the reward of the information that can be obtained. These tests usually are performed by a radiologist.
Don’t Miss: How Do You Get Ulcers In Your Mouth
Points To Consider About Acne Treatment
If you are considering using Accutane, or if you have used this drug in the past and are concerned about IBD, you should discuss your risk with your dermatologist. Keep in mind that if there is a risk of developing IBD after taking Accutane, it is still a very uncommon occurrence. One case-control study done in 2011 suggests that those considering taking Accutane should be made aware of the small risk of developing ulcerative colitis.
For people who already have IBD, especially ulcerative colitis, and who are seeking treatment for severe acne, first-line therapy is often with topical agents. If topical treatment is ineffective, antibiotics and antimicrobials may be used.
How You May Feel
Ulcerative colitis attacks the lining of your digestive tract. It causes swelling and sores in the lining.
If youâve just been diagnosed with it, hereâs what might happen during a flare-up:
You might have some of those symptoms, but not all. And they may change over time. They can range from very mild to very bad.
Read Also: I Think I Have Ulcerative Colitis
Read Also: Do You Still Have Ulcerative Colitis After Colectomy