What Are The Treatment Procedures For Diabetic Foot Ulcers
In the initial stages of foot ulcers, debridement may prove to be an effective solution. In debridement, your doctor uses a scalpel to remove the dead and infected tissues from the ulcerated wound. The doctors cover the wound with a sterile bandage and replace it regularly. Besides debridement, other non-surgical treatment methods for diabetic foot ulcers include off-loading or Total Contact Casting and hyperbaric oxygen therapy.
Along with debridement, your doctor may also enforce infection control methods. Your doctor may prescribe antibiotics that help to prevent infection in the wound. Usually, ointments and creams help in fastening the healing process.
In serious cases, however, surgery may be required. If the underlying cause of the ulcer is a vascular problem, vascular surgeries like atherectomy, balloon angioplasty, foot & ankle surgery, and vascular reconstruction are the treatment options depending on the severity of the condition. In many cases, surgical and non-surgical procedures are combined to effectively treat diabetic foot ulcers.
Fortunately, these vascular surgeries are available at Pristyn Care. Our team of experienced surgeons is capable enough to perform these procedures efficiently. If you have any queries about vascular surgeries, you can call us. Our medical coordinators will book the appointment with the best vascular surgeons for you.
Also Read:
What Causes Foot Ulcers
Some of the common reasons or ulcers are:
-
Pressure or Circulation problems – this could be resulting from an increased pressure to the foot, or poor blood flow to the foot
-
Open Wounds
-
Blisters
-
Poorly fitting shoes – this may cause blisters or aforementioned pressure problems
-
Nerve damage resulting in loss of sensation in your feet – often the loss of feeling in the foot means the above problems are not felt further aggravating the issue. ?
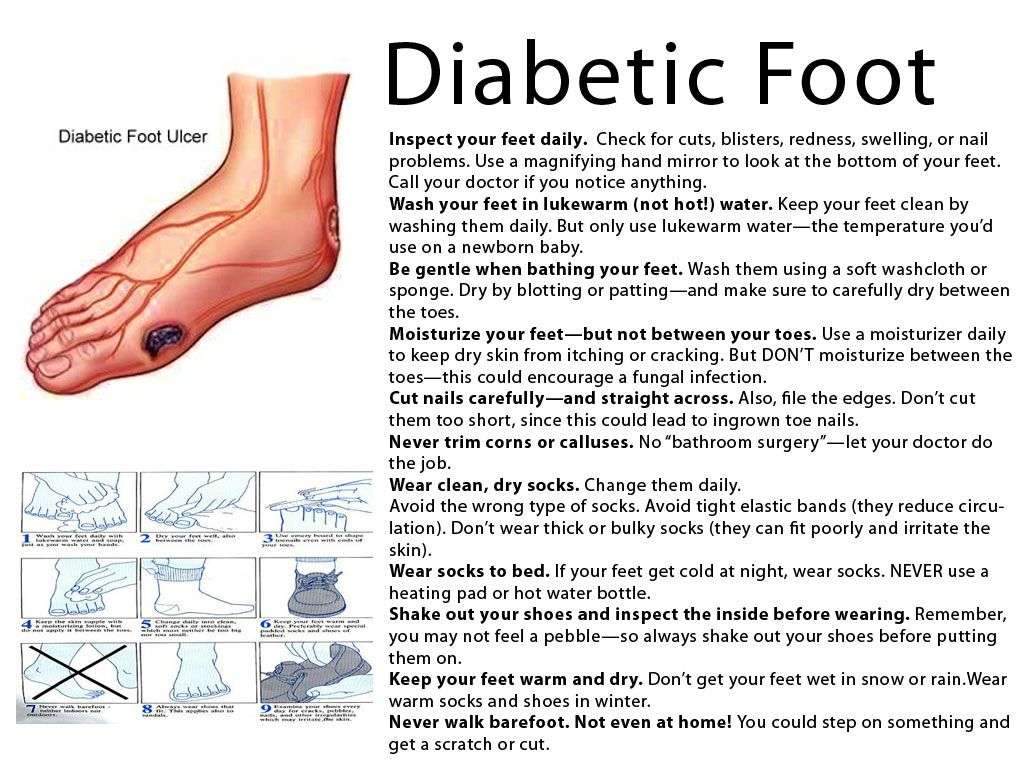
Prevention is always better than cure so here are our tips:
-
It is important to check your skin daily and if you notice open wounds to treat them immediately.
-
Wash your feet and moisture on the daily.
-
Wear protective footwear such as shoes and socks.
History Of Previous Ulceration And Amputation
A diabetic patient with a history of previous ulceration or amputation is at increased risk for further ulceration, infection and subsequent amputation. Alterations in foot dynamics due to ulceration, joint deformity or amputation can cause the abnormal distribution of plantar pressures and result in the formation of new ulcers28.
Recommended Reading: Over The Counter Ulcer Treatment For Horses
What Is A Diabetic Foot Ulcer
An ulcer is a chronic wound that remains open. Diabetic foot ulcers are common and serious complications of diabetes. If they are not recognized and treated promptly, said Dr. Bruyn, increase the risk of:
- infection
- amputation
- Death
Some ulcers can be difficult to heal, while others simply require minor treatment and adjustments to shoe wear.
The best thing we can do for an ulcer is to detect it early, hopefully while it is still a callus or a blister, said Dr. Bruyn. If an ulcer reaches bone level, treatment usually involves some form of procedure to remove devitalized tissue or infection.
Preventing ulcers from initiation or immediate treatment is key to warding off bigger problems.
If the foot becomes infected, amputation of the toes or part of the foot is often required to allow the remaining foot to heal, said Dr. Bruyn said. A toe or partial toe amputation increases the risk of injuries adjacent to the foot, and the overall mortality rate for a patient with a diabetic foot ulcer is actually worse than some cancers.
Foot ulcers are just one of the potential complications of living with diabetes. Click here to find out the rest.
Based On The Severity Of The Condition There Can Be 6 Stages In The Development Of A Diabetic Foot Ulcer
0: Intact skin
2: Deep ulcer extending to the tendon, bone or joint
3: Deep ulcer along with the formation of an abscess
4: Gangrene in the forefoot
5: Gangrene affecting the complete foot
If you notice any of these symptoms, consult a doctor immediately. Diabetic foot ulcers have a tendency to worsen over time and if left untreated, they can lead to serious complications and infections. Diabetic foot ulcers may even lead to foot amputations in serious cases.
Don’t Miss: Can A Heating Pad Help Ulcerative Colitis
More About Foot Ulcers
Why Does My Foot Hurt?
Use this tool to determine what condition may be causing your foot pain or other symptoms, and which foot-health professionals might help.
PLEASE NOTE: IPFH does not give, sell, rent or market your personal data to third parties. If we use your e-mail address to contact you, we will provide you a method described in the e-mail that you receive that allows you to opt-out of future correspondencevia e-mail back to us..
Assessment Of Possible Peripheral Neuropathy
Signs of peripheral neuropathy include loss of vibratory and position sense, loss of deep tendon reflexes , trophic ulceration, foot drop, muscle atrophy, and excessive callous formation, especially overlying pressure points such as the heel.
The nylon monofilament test helps diagnose the presence of sensory neuropathy. A 10-gauge monofilament nylon is pressed against each specific site of the foot just enough to bend the wire. If the patient does not feel the wire at 4 or more of these 10 sites, the test is positive for neuropathy. General use filaments can be obtained from the National Institute of Diabetes and Digestive and Kidney Diseases, or the clinician can use professional Semmes-Weinstein filaments.
References
Amin N, Doupis J. Diabetic foot disease: From the evaluation of the “foot at risk” to the novel diabetic ulcer treatment modalities. World J Diabetes. 2016 Apr 10. 7 :153-64. . .
Naves CC. The Diabetic Foot: A Historical Overview and Gaps in Current Treatment. Adv Wound Care . 2016 May 1. 5 :191-197. . .
Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for Medicare and private insurers. Diabetes Care. 2014. 37 :651-8. .
Gentile AT, Berman SS, Reinke KR, Demas CP, Ihnat DH, Hughes JD, et al. A regional pedal ischemia scoring system for decision analysis in patients with heel ulceration. Am J Surg. 1998 Aug. 176:109-14. .
Jeffcoate WJ, Harding KG. Diabetic foot ulcers. Lancet. 2003 May 3. 361:1545-51. .
Recommended Reading: Vsl 3 And Ulcerative Colitis
What To Do If You Notice A Problem
The signs of diabetic ulcers on the foot should never be left untreated. If you have any of the symptoms mentioned above or think you might have a foot sore or ulcer, you should be seen by a doctor as soon as possible to avoid further damage and possible infection. The earlier you seek medical help, the less chance of complications further down the line.
Here at the Midwest Institute for Non-Surgical Treatment , we have qualified podiatrists who can provide you with the right treatment for your diabetic foot ulcer. We’ll also advise you on how best to look after your feet to prevent reoccurrences.
Book an appointment with Dr. Akinwande and the team who can treat you at one of our convenient locations in the St Louis area. Call us today, and we’ll get you back on your feet and the path to recovery.
How Is A Diabetic Foot Infection Diagnosed
A doctor should be able to provide a diabetic foot infection diagnosis. During your appointment, you should expect the doctor to complete a thorough physical examination. They will look for local signs of an infection, like swelling and discharge, as well as systemic signs, like a fever. The doctor will remove any existing necrotic tissue and clean the wound, and they may take a sample to determine the severity of the infection. This tissue sample will be sent to a lab to determine which antibiotic treatment will best help. If the doctor suspects your diabetic foot infection is serious, they may order an X-ray and look for signs of bone infection.
While the signs of infection may sound easily recognizable, only a doctor has the experience and education necessary to provide an accurate diagnosis. If you think you may have a foot infection or other type of injury, schedule an appointment as soon as possible. Seeing a doctor earlier in the process can reduce the risk of developing irreversible health issues.
Don’t Miss: Signs Of Ulcers In Horses
Symptoms Of Foot Ulcers
A foot ulcer may be painful if the wound is open and doesnt heal however, if you have neuropathy, you may not feel pain and you wont realize you have an ulcer unless you inspect your feet daily. Blood or discharge stains on socks or in footwear may signify a sore, a cut or an ulcer, so if you have neuropathy also inspect your sockwear and shoes daily.
What Other Conditions Can Affect Diabetic Feet
People with diabetes also can develop Charcot foot, a rare complication that can cause permanent deformity. In Charcot foot, nerve damage weakens the bones and joints. The bones can break, and the joints can dislocate or collapse.
Read more about preventing diabetes complications.
A note from Cleveland Clinic
Diabetic feet are at risk for ulcers and infections, which may go unnoticed in people with diabetic neuropathy and numbness. If you have diabetes, its important to care for your feet every day and report any problems to your healthcare provider. Early treatment can prevent hospitalization, deformity and amputation.
Last reviewed by a Cleveland Clinic medical professional on 04/26/2021.
References
Recommended Reading: Artificial Sweeteners And Ulcerative Colitis
From Injury Or Blister To Ulcer
If a person with decreased sensation gets a blister or other injury, they may not notice it and it can develop into an ulcer.
Neuropathy:Neuropathy is a general term for nerve dysfunction. Peripheral neuropathy is the most common type of neuropathy in people with diabetes and typically affects the nerves of the feet, legs, and sometimes the arms and hands.
People with diabetes are at increased risk for peripheral neuropathy if they have a history of hyperglycemia and have had diabetes for a long time. Other risk factors for neuropathy include smoking and genetic predisposition.
Over time elevated blood sugar levels can affect nerve functioning and nerve signaling. Small nerve dysfunction results in the inability to feel pain, and large fiber dysfunction causes disturbances in balance, which can increase the risk of falls.
If a person has neuropathy and injures their foot without feeling it, they may not notice it until it gets much worse. Recurrent, unnoticed injuries to the foot can increase the risk of Charcot foot, in which progressive destruction of the bones and joints leads to foot deformity.
Autonomic neuropathy can cause a decrease in sweating, resulting in dry feet. Having dry feet can increase the risk of developing calluses. While calluses are healthy, if you have lost sensation, they can grow deeper cause damage to the skin surface known as breakdown, putting the foot at risk of blisters or ulcers.
Clinical Signs Of Wound Infection

Twelve clinical signs of localized wound infection have been reported. Erythema, edema, heat, and pain are signs of inflammation. Signs of inflammation plus purulent exudate are known as classic signs of infection, traditionally associated with wound infection. Serous exudate, delayed healing, friable granulation tissue, discolored granulation tissue, foul odor, pocketing of the wound base, and wound breakdown are thought of as signs specific to secondary wounds , those healing by secondary, rather than primary intention.
In a heterogeneous sample of chronic wounds, none of the classic signs or signs specific to secondary wounds was found to be a useful diagnostic test for infection . However, only two wounds were DFUs. The diagnostic validity of clinical signs may differ by chronic wound etiology. In addition, combining signs may be more useful in identifying infection than any one sign.
Don’t Miss: Pressure Relieving Mattress For Pressure Ulcers
Early Signs Of A Foot Ulcer
If you have diabetes, its imperative that you perform regular foot checks to look for the early warning signs of an ulcer or other foot issues. Here are some of the first hints that a foot ulcer may be developing:
1. Drainage/Sock Discoloration One of the first signs for a diabetic foot ulcer that you may notice is on your sock. If you begin to notice yellow or clear discoloration on your sock above an area where you may have a small irritation, its a sign that the body is attempting to repair a problem in the area. If the area cant get enough oxygenated blood, the wound may worsen and the drainage will get worse. If you notice fluid buildup or some discharge on your sock, take a closer look at your foot.
2. Redness Redness is also a sign that the body is attempting to address an issue, so if a certain spot on your foot is starting to get red or darker in color, its a sign that the area could be susceptible to ulcer formation.
3. Swelling If an area of your feet or your whole foot has started to swell a bit, its a sign that fluid is pooling in your foot and that healthy blood flow in and out of the area may not be all that effective. This means it will be harder for wounds or sores to heal. If you have any irritations or sores on your feet and they are swollen, know that the environment is right for a foot ulcer and you should take some mitigation steps.
What Are The Causes Of Diabetic Foot Ulcers
Even minor cuts, injuries, small blisters, or wounds can initiate diabetic foot ulcers. This happens because the presence of diabetes slows down the healing process. Along with this, most diabetes patients become ischemic over time which means they lose sensations in the nerves due to which they dont feel pain. As a result, the wound or cut becomes more serious and becomes prone to ulcers and infections without the knowledge of the patient.
Don’t Miss: Signs Of Ulcers In Colon
Sensory And Autonomic Neuropathy
Distal symmetric polyneuropathy is perhaps the most common complication affecting the lower extremities of patients with diabetes mellitus. This complication occurs in up to 58 percent of patients with longstanding disease.19 Neuropathy, a major etiologic component of most diabetic ulcerations, is present in more than 82 percent of diabetic patients with foot wounds.4 This lack of protective sensation, combined with unaccommodated foot deformities, exposes patients to undue sudden or repetitive stress that leads to eventual ulcer formation with a risk of infection and possible amputation.20
In the diabetic foot, autonomic neuropathy has several common manifestations. First, denervation of dermal structures leads to decreased sweating. This causes dry skin and fissure formation, which predispose the skin to infection. In vascularly competent patients, this autosympathectomy may lead to increased blood flow, which has been implicated as one of the primary etiologic factors in the development of Charcot’s joint and severe foot deformity.2123
The nylon monofilament test is a simply performed office test to diagnose patients at risk for ulcer formation due to peripheral sensory neuropathy.24 The test is abnormal if the patient cannot sense the touch of the monofilament when it is pressed against the foot with just enough pressure to bend the filament25 . Physicians can obtain a monofilament kit at a small cost from the National Diabetes Information Clearing-house .
Irritated Or Wounded Feet
Ulcers can sometimes be a result of improperly fitting or even inappropriate shoes. Wearing improper footwear can cause abnormal weight-bearing, areas of concentrated pressure, and abnormal shear forces on the feet. This can then increase the likelihood of experiencing foot stress.
There are three main types of ulcers.
Don’t Miss: How To Heal Venous Stasis Ulcers
How To Spot The Signs Of A Diabetic Ulcer On The Foot
A foot ulcer is one of the most common and serious complications for people with diabetes, occurring in approximately 15% of patients, according to the American Podiatric Medical Association. Diabetic ulcers on the foot can occur in anyone with type 1 and type 2 diabetes and refer to an open sore on the foot, usually forming under big toes and at the bottom of feet. The main reasons people with diabetes develop foot ulcers are:
- Trauma or injury to the foot
- Poorly fitting shoes
- Poor blood flow to the foot
- Increased pressure to the foot
- Nerve damage which means you are unable to feel your feet properly
If you’ve had a diabetic ulcer on the foot for a long time, you are at greater risk of infection, which can spread from the wound to the bone. While there are antibiotics that can treat these infections, if too much bone has been damaged, the foot will have to be removed or amputated.
Therefore patients and caregivers need to be able to identify these types of wounds to prevent them from getting worse. So how do you know if you have a diabetic foot ulcer?
If the ulcer is at an advanced stage, it should be obvious. A foot ulcer looks like a round red crater in the skin bordered by thickened callused skin. Severe ulcers can be deep enough to expose tendons or bones. However, other symptoms may not be easy to identify or could be an indication of another problem. That being said, here are some of the common signs of diabetic foot ulcers to look out for.
How Is A Diabetic Foot Ulcer Treated
Care for diabetic foot pain may involve a doctor who specializes in the feet, called a podiatrist. Treatment may include:
- Cleaning the wound.
- Draining any fluid or pus from the ulcer.
- Removing or cutting away dead or infected tissue .
- Applying special bandages and ointments to absorb extra fluid, protect the wound and help it heal.
- Prescribing a wheelchair or crutches to take weight off the affected foot .
- Prescribing oral or IV antibiotics to control and eliminate infection.
Depending on how severe the infection is, your healthcare provider may recommend hospitalization. Sometimes amputation is necessary to prevent infection from spreading to other parts of the body.
Don’t Miss: Crohn’s Versus Ulcerative Colitis Pathology