Personalizing Treatment In Ibd: Hype Or Reality In 2020 Can We Predict Response To Anti
- 1Department of Medicine, Medical Clinic 1, University Hospital Erlangen, University of Erlangen-Nürnberg Erlangen, Erlangen, Germany
- 2Deutsches Zentrum Immuntherapie , Erlangen, Germany
- 3The Transregio 241 IBDome Consortium, Erlangen, Germany
- 4The Transregio 241 IBDome Consortium, Berlin, Germany
- 5Medizinische Klinik m. S. Gastroenterologie, Infektiologie und Rheumatologie, Charité – Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin, Humboldt-Universität zu Berlin, Berlin, Germany
- 6Berlin Institute of Health, Berlin, Germany
Adverse Effects Of Biological Therapy
The randomized, controlled trials have demonstrated a generally favorable safety profile for biological agents however, a few patients do experience side-effects and biological agents have been occasionally associated with severesometimes life threateningadverse effects necessitating careful monitoring of therapy . Many of these adverse effects are related to the immunosuppressive effects of biological agents. These are discussed below.
Read Also: Does Stelara Work For Ulcerative Colitis
Study Setting And Data Sources
We conducted a population-based study in adult patients with IBD residing in Ontario between 1 July 1995 and 31 March 2012 using provincial health administrative data. Ontario is a geographically and ethnically diverse province of Canada comprising more than 13 500 000 residents and close to 100000 individuals with IBD. The Ontario government covers 100% of the costs of medically necessary healthcare services for all its citizens, including hospital-based care, ambulatory physician visits and procedures and chronic care services. It also subsidises the cost of select prescription drugs for individuals aged 65 years or older and those requiring social assistance, through the Ontario Drug Benefits Programme, as well as the costs of expensive drugs, such as biologic therapies, on a case-by-case basis through the ODB Exceptional Access Programme. Across Canada, 41.8% of prescribed drug spending is paid for by provincial healthcare plans.
Also Check: Is Ginger Tea Good For Ulcerative Colitis
Recommended Reading: Can You Drink Coffee With Ulcerative Colitis
Beyond Tnf Inhibitors In Ulcerative Colitis: Promising Data
Nicola M. Parry, DVM
The availability of tumor necrosis factor inhibitors changed treatment for many patients with ulcerative colitis , but not everyone responds to these drugs, and even among those who do so initially, response often diminishes over time. Now, two trials, published online September 26 in the New England Journal of Medicine, show that many of these patients do respond to other types of biologic therapy.
In the head-to-head VARSITY trial, vedolizumab was superior to adalimumab with respect to achievement of clinical remission and endoscopic improvement, write Bruce E. Sands, MD, from the Icahn School of Medicine at Mount Sinai, New York City, and colleagues in the VARSITY study group.
In the UNIFI trial, ustekinumab was more effective than placebo for inducing and maintaining remission, write Sands and colleagues in the UNIFI study group.
The findings are potentially important for long-term outcomes, writes Richard J. Farrell, MD, from Connolly Hospital and the Royal College of Surgeons in Ireland, Dublin, in an accompanying editorial.
Despite an improving treatment landscape, long-term rates of colectomy for ulcerative colitis have not declined over a 10-year period, a fact that highlights the need for new biologic therapies and strategies, he writes.
Usketinumab Active In Moderate To Severe Disease
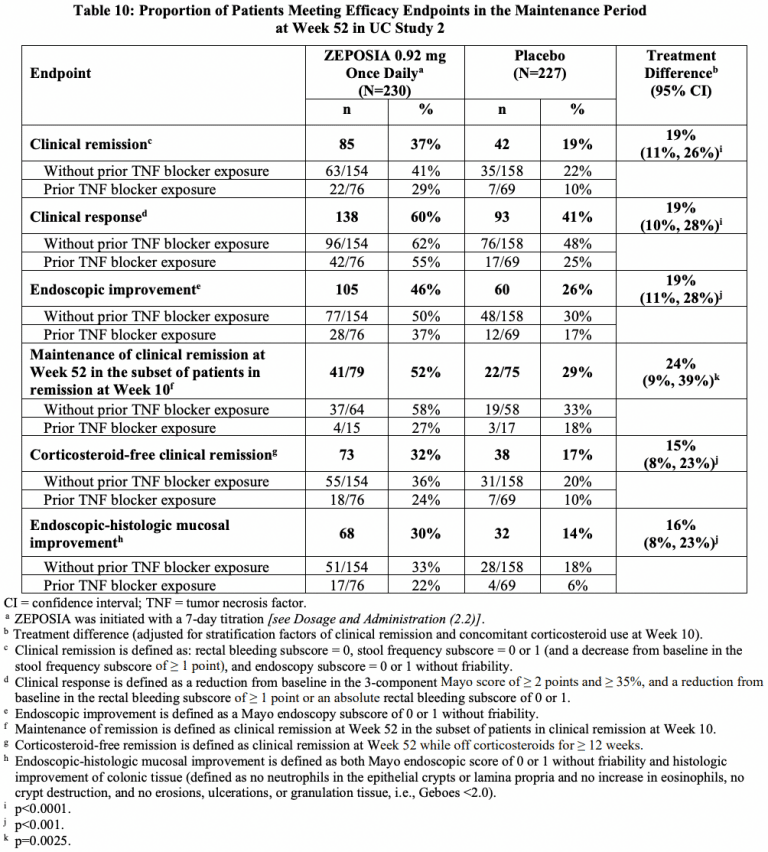
The trial enrolled 961 adults aged 18 years or older. Participants were randomly assigned to receive an IV induction dose of ustekinumab 130 mg , or a weight-range-based dose of approximately 6 mg/kg of body weight , or placebo .
“Patients who had a response to induction therapy 8 weeks after administration of intravenous ustekinumab were randomly assigned again to receive subcutaneous maintenance injections of 90 mg of ustekinumab or placebo ,” the authors say.
In both the induction and maintenance phases of the study, the primary endpoint was clinical remission.
During the induction phase, more patients in both ustekinumab groups achieved clinical remission at week 8 compared with those in the placebo group .
In addition, significantly more patients in the ustekinumab groups achieved endoscopic improvement , clinical response , and mucosal healing at week 8.
Similarly, among patients who underwent a second randomization, more patients in both ustekinumab groups achieved clinical remission in the maintenance phase at week 44 compared with those in the placebo group .
In the maintenance phase, more patients in the ustekinumab groups also achieved maintenance of clinical response through week 44 , endoscopic improvement , and corticosteroid-free remission .
According to the authors, the treatment regimen was well tolerated and safe.
Cancers developed in 7 of 825 patients who received ustekinumab , and in 1 of 319 who received placebo .
Don’t Miss: Do Ulcers Cause Acid Reflux
Biological Therapy And The Natural History In Ulcerative Colitis
The natural history of UC is that of a progressive disease leading to high rates of surgery and morbidity . Treatment with biological therapy has demonstrated the potential to alter the natural history of UC, including reduced colectomy rates and improved quality of life. This may be related to the mucosal healing effects of biological therapy as discussed above. Previous studies have suggested that improvement in mucosal healing rates is associated with better long-term outcomes and reduced rates of colectomy .
Using data from the ACT1 and ACT2 trials, a subsequent study demonstrated that patients treated with infliximab had a significantly lower rate of colectomy by week 54 than those treated with placebo . Additionally, patients treated with infliximab had a significantly lower rate of UC-related hospitalizations, surgeries/procedures per 100 patient-years than those treated with placebo.
In another randomized, double-blinded, placebo-controlled trial of 45 hospitalized patients with intravenous steroid-refractory flare of moderate-to-severe UC, patients who received a single infusion of infliximab after administration of steroids required colectomy significantly less frequently at 3 months following the infusion, than those who received placebo . A follow-up study on the same cohort also showed similar results at 3-year follow-up .
More Options Means More Questions
“Looking back almost 25 years ago, the struggle was how to work with just one biologic and how to make it last for patients who have already failed all the available therapies. All these years later, we have such riches that the question we most often deal with is ‘What’s my first treatment?’ for patients with inflammatory bowel disease,” Arun Swaminath, MD, told Medscape Medical News, when asked to comment on both studies.
“Increasingly, we are seeing industry do head-to-head trials of drugs, but this is a time-consuming and expensive process,” added Swaminath, chief of gastroenterology and director of the inflammatory bowel diseases program at Lenox Hill Hospital in New York City.
The study from Buisson and colleagues in UC approaches the design of a head-to-head trial, Swaminath said. “In the end, their primary endpoint was a statistical dead heat between the two options.”
In the VERSUS-CD study, vedolizumab was compared with ustekinumab “with more patients not discontinuing ustekinumab therapy compared to vedolizumab,” he said. “This study also seems to favor sicker patients being treated with ustekinumab.”
“In both cases, we are starting to see the ‘order’ of treatments take shape, even before the benefit of head-to-head trials,” Swaminath said.
ECCO 2022 Congress: DOP Abstract 76 and DOP Abstract 78. Presented February 18, 2022.
Don’t Miss: Foods That Prevent Stomach Ulcers
How You Take Them
Some TNF inhibitors, including Cimzia, Humira, Enbrel, Erelzi, and Simponi, are given as shots under the skin. Youll get your first one or two at your doctors office then your doctor or a nurse will show you how to give them to yourself. Once you get comfortable with that, pre-filled shots can be shipped to your home.
Every 1 to 4 weeks, youll inject your TNF inhibitor under the skin of your thigh or abdomen. You can use a different spot each time.
Remicade, Inflectra, and Simponi Aria, a version of Simponi, are given as infusions at a clinic or your doctors office. While you lie still, its slowly dripped into your vein through a tube. For Remicade, each session can take around 2 hours, and youll need treatment every 4 to 8 weeks. With Simponi Aria, the sessions last 30 minutes. After two starter doses one month apart, theyre given once every 8 weeks.
Your doctor may have you use a TNF inhibitor in combination with other drugs, such as methotrexate, prednisone, hydroxychloroquine , leflunomide , or sulfasalazine .
You may have to take these medications for a long time. If you go off them because you feel better, your inflammation can come back. Some people can cut down their dose instead of stopping the drugs altogether. Always take your medication as your doctor prescribes.
Read Also: Can Diet Help Ulcerative Colitis
What Are Biologics For Ulcerative Colitis
Biologics are medications that doctors use to treat chronic inflammatory conditions such as inflammatory bowel disease . Ulcerative colitis is one type of IBD.
These laboratory-made antibodies are targeted to block specific proteins responsible for the inflammation that drives ulcerative colitis. This makes biologics different from medications such as corticosteroids, which may cause more severe side effects.
The Food and Drug Administration has approved the following biologics to treat moderate-to-severe ulcerative colitis:
- anti-tumor necrosis factor agents, including:
The FDA approved the biosimilars of infliximab and adalimumab. As their name suggests, biosimilars are very similar to the originally approved biologics but may be more cost effective.
A person may receive biologics as an injection, as an infusion through an intravenous line, or by mouth.
The method of use, dosage, and frequency varies from one type of biologic to another.
Doctors typically prescribe an anti-TNF agent before they prescribe other types of biologics for moderate-to-severe ulcerative colitis. This is because anti-TNF medications are the most studied treatments.
Doctors may prescribe another type of biologic or a JAK inhibitor if the anti-TNF agent:
JAK inhibitors can include
Don’t Miss: Can Ulcerative Colitis Cause Acid Reflux
Different Gene Signature Profiles
A study in patients with colonic CD, identified a gene signature profile composed of TNFAIP6, S100A8, IL11, G0S2, and S100A9, which predicted primary infliximab response with 100% accuracy . A subsequent study performed by another group in their cohort of CD patients supported the role of the reported expression signature as predictive for primary anti-TNF outcome . High baseline IL13RA2 levels were associated with lack of mucosal healing in anti-TNF treated CD patients. The authors also showed TNF-driven pathways were significantly enriched in primary non-responders to infliximab and linked to increased mucosal IL13RA2 expression . GATA3 expressing lamina propria CD4+ T lymphocytes were increased in anti-TNF endoscopic primary non-responders compared to responders in CD patients .
One of the first studies to investigate the predictive capacity of gene expression profiles in UC patient samples and primary response to subsequent anti-TNF therapy was undertaken in 2009. Here, colonic tissue transcriptomics in biopsy samples that were taken prior to initiation of infliximab therapy in two cohorts of UC patients led to the identification of a five-gene signature consisting of osteoprotegerin, stanniocalcin-1, prostaglandin-endoperoxide synthase 2, IL-13 receptor alpha 2 , and IL-11, that are all involved in the adaptive immune response. This panel of genes separated responders from non-responders with 95% sensitivity and 85% specificity .
Indications For Tnf Inhibitors
Crohns Disease
European consensus guidelines and the American College of Gastroenterology guidelines list similar indications for TNF inhibitors for CD, which include
-
steroid refractory or dependant disease,
-
immunomodulator refractory disease,
-
severely active disease with adverse prognostic factors, and
-
fistulizing disease.
Negative prognostic factors for CD include disease onset below age 40 years, perianal disease, active smoking, prior intestinal surgical resection, need for steroids at diagnosis, stricturing disease, and small intestinal disease .
Ulcerative Colitis
Indications for TNF inhibitors in UC include
-
steroid refractory severe colitis,
-
oral steroid refractory disease, and
-
immunomodulator refractory disease.
Negative prognostic factors for UC include disease onset at the age of < 16 years, C-reactive protein > 10 mg/L after 1 year of extensive colitis, and admission for acute severe colitis .
Combination Therapy of anti-TNF Agents with Immunomodulators
Contraindications and Precaution
The relative or absolute contraindications of TNF inhibitors can be summarized by the acronym STOIC: Sepsis/abscess, Tuberculosis, Optic neuritis , Infusion reaction , Cancer/lymphoma and Congestive heart failure .
Prebiological Treatment Screening
Read Also: Can Ulcerative Colitis Cause Positive Ana
You May Like: Safety Considerations For Ulcerative Colitis
Disease Duration And Location
In patients with CD, shorter disease duration has been repeatedly described to predict higher responsiveness to anti-TNF drugs. In post hoc analyses of phase 3 clinical trials, patients with disease duration below 2 years had significantly better primary response rates to adalimumab and certolizumab pegol than those with long-standing disease. In UC, available data could not find a similar association .
Regarding disease location, differences between isolated ileal and colonic disease manifestation have been described. Post-hoc analysis of a placebo-controlled trial with certolizumab pegol showed higher probability of patients with colonic compared to isolated ileal disease to achieve clinical remission at week 6 of induction therapy . Several cohort studies also indicated better short-term and sustained clinical response to anti-TNF therapy in isolated colonic than in ileal CD . Endoscopic and histologic healing were also more frequent in colon that the ileum after 1 year of adalimumab therapy in the EXTEND trial . For UC, there was no association between disease extend and probability of therapeutic induction and maintenance response to anti-TNF treatment .
Tumour Necrosis Factor Alpha Blocking Agents For Treatment Of Active Ulcerative Colitis
Ulcerative colitis is a chronic relapsing inflammatory disorder of the large bowel. Although corticosteroids are effective for treating ulcerative colitis, approximately 20% of patients who respond become sick again when steroids are withdrawn and become steroid dependent. Furthermore, corticosteroids exhibit significant adverse effects. Tumour necrosis factor alpha is a proinflammatory cykotine that is involved in the pathogenesis of rheumatoid arthritis, Crohn’s disease and psoriasis. TNF- blocking drugs may provide an alternative treatment for patients who do not respond to corticosteroid and/or immunosuppressive drug treatment. This review shows that intravenous infusions of infliximab, a TNF- blocking agent is effective in inducing clinical remission, promoting mucosal healing, and reducing the need for colectomy in patients with active ulcerative colitis whose disease has not responded to conventional treatment.
In patients with moderate to severe ulcerative colitis whose disease is refractory to conventional treatment using corticosteroids and/or immunosuppressive agents, infliximab is effective in inducing clinical remission, inducing clinical response, promoting mucosal healing, and reducing the need for colectomy at least in the short term. Serious adverse events attributable to infliximab were not common in the included studies but physicians should be aware of and be prepared to deal with potential adverse events such as anaphylactic reactions and infections.
You May Like: Best Medicine For Ulcerative Colitis
How Do Biological Medications For Ibd Affect The Eyes
Biological medications are drugs produced using living cells. The most common biologics for IBD fall within a class of drugs called tumor necrosis factor -alpha inhibitors. TNF-alpha inhibitors help to block inflammation from the immune system, which makes them effective at treating the symptoms of Crohns and ulcerative colitis.
Typical TNF-alpha inhibitors include:
Many MyCrohnsAndColitisTeam members also report having taken another medication called ustekinumab . This is not a TNF-alpha inhibitor but works to reduce inflammation in people with IBD.
People who take TNF-alpha inhibitors typically tolerate them well regarding side effects. Eye complications from TNF-alpha inhibitors are rare and include:
Although someone with IBD can develop uveitis after taking a TNF-alpha inhibitor, uveitis is also linked to IBD itself. Taking a TNF-alpha inhibitor can help decrease the signs and symptoms of uveitis by treating IBD.
Eye complications associated with ustekinumab are rare. When they occur, they include:
- Light sensitivity
- Seeing halos around lights
If youre taking a steroid or biologic medication for IBD and experience changes to your vision, you should tell your doctor or health care provider as soon as possible. This allows the doctor to treat the visual problem promptly and/or refer you to a specialist if needed.
Lower Rates Of Remission Versus Younger Ibd Patients Japanese Study Finds
byZaina Hamza, Staff Writer, MedPage Today April 1, 2022
Tumor necrosis factor inhibitors were less effective for patients who developed inflammatory bowel disease later in life, a retrospective study in Japan found.
In an analysis of patients hospitalized for IBD and initiating biologic therapy, those diagnosed with IBD at age 60 or older had significantly lower rates of clinical remission after a year of TNF inhibitor treatment compared to younger patients , as well as lower rates of steroid-free remission , reported Tetsuo Takehara, MD, PhD, of the Osaka University Graduate School of Medicine in Japan, and colleagues.
But elderly IBD patients diagnosed before age 60 had clinical and steroid-free remission rates comparable to the younger group, they noted in Nature Scientific Reports.
Furthermore, severe adverse events leading to treatment discontinuation were more frequent in older IBD patients with elderly-onset disease and cumulative SAEs were significantly higher .
Among older IBD patients, identifying those with elderly-onset disease is important as those with longer disease duration may have fewer hospitalizations, IBD-related surgeries, and a lower rate of corticosteroid use during disease exacerbation, Takehara’s group noted.
“In practice, it may be preferred to consider different classes of biologic agents with more favorable safety profiles when treating this patient population,” she told MedPage Today.
Disclosures
Don’t Miss: How Long Do Stomach Ulcers Last
Tumor Necrosis Factor Alpha Blocking Agents As Treatment For Ulcerative Colitis Intolerant Or Refractory To Conventional Medical Therapy: A Meta
- Ruxi Lv ,
Contributed equally to this work with: Ruxi Lv, Weiguang Qiao
Affiliations School of Traditional Chinese Medicine, Southern Medical University, Guangzhou, People’s Republic of China, Research Institute of Traditional Chinese Medicine, Guangdong Medical College, Zhanjiang, Guangdong, People’s Republic of China
-
Contributed equally to this work with: Ruxi Lv, Weiguang Qiao
Affiliation Department of Gastroenterology, Nanfang Hospital, Southern Medical University, Guangzhou, People’s Republic of China
-
Affiliation School of Traditional Chinese Medicine, Southern Medical University, Guangzhou, People’s Republic of China
-
Affiliation Research Institute of Traditional Chinese Medicine, Guangdong Medical College, Zhanjiang, Guangdong, People’s Republic of China
-
Affiliation Emergency Department of Nanfang Hospital, Southern Medical University, Guangzhou, People’s Republic of China
-
* E-mail:
Affiliation Research Institute of Traditional Chinese Medicine, Guangdong Medical College, Zhanjiang, Guangdong, People’s Republic of China