Strategies To Reduce Your Risk Of Colorectal Cancer
Having regular colonoscopies is one of the most important preventive measures people with ulcerative colitis can take to reduce the risk of colorectal cancer.
There are also other steps people with UC can take to minimize risk, including avoiding smoking, limiting alcohol intake, maintaining a healthy weight, and exercising regularly.
Other tactics that have been shown to reduce the risk of colorectal cancer include the following:
Who Is At Risk For Developing Ulcerative Colitis
Anyone can get ulcerative colitis at any age. There are certain factors that can increase someones risk for getting ulcerative colitis. These factors include:
- Having a close relative with inflammatory bowel disease
- Being between 15 and 30, or older than 60
- Eating a high-fat diet
- Using frequent nonsteroidal anti-inflammatory drugs like ibuprofen
Having An Inherited Syndrome
About 5% of people who develop colorectal cancer have inherited gene changes that cause family cancer syndromes and can lead to them getting the disease.
The most common inherited syndromes linked with colorectal cancers are Lynch syndrome and familial adenomatous polyposis , but other rarer syndromes can increase colorectal cancer risk, too.
Lynch syndrome
Lynch syndrome is the most common hereditary colorectal cancer syndrome. It accounts for about 2% to 4% of all colorectal cancers. In most cases, this disorder is caused by an inherited defect in either the MLH1, MSH2 or MSH6 gene, but changes in other genes can also cause Lynch syndrome. These genes normally help repair DNA that has been damaged.
The cancers linked to this syndrome tend to develop when people are relatively young. People with Lynch syndrome can have polyps, but they tend to only have a few. The lifetime risk of colorectal cancer in people with this condition may be as high as 50% , but this depends on which gene is affected.
Women with this condition also have a very high risk of developing cancer of the endometrium . Other cancers linked with Lynch syndrome include cancer of the ovary, stomach, small intestine, pancreas, kidney, prostate, breast, ureters , and bile duct. People with Turcot syndrome who have a defect in one of the Lynch syndrome genes are at a higher risk of colorectal cancer as well as a specific type of brain cancer called glioblastoma.
Familial adenomatous polyposis
Also Check: Best Natural Remedies For Stomach Ulcers
How Colitis May Affect Your Cancer Risk
Signs and symptoms of colon cancer can be tougher to discern in ulcerative colitis patients. Blood in the stool, for example, which is a warning sign of cancer, may also happen as a result of a flare-up of the condition. The cancer itself is different, too, says Dr. Chang. Cancer in UC patients looks more like lesions, and less like masses or tumors, she says. But certain factors can increase your likelihood of developing cancer, including:
- The Severity of the Condition The longer you have uncontrolled inflammation, the more likely you are to develop dysplasia. Put another way, its not just having ulcerative colitis that ups your cancer risk its having uncontrolled UC that puts you in the danger zone.
- How Much of Your Colon is Affected If just the 5 to 10 centimeters of colon closest to the rectum is affected a condition called ulcerative proctitis your risk is similar to that of the normal population. If your entire colon is affected, your risk rises.
Crohns Disease Increases Risk Of Intestinal Cancer
According to a combined analysis of six studies, individuals with Crohns disease have an increased risk of developing colorectal cancer and small intestine cancer.
In order to evaluate the relationship between Crohns disease and risk of colorectal cancer and small intestine cancer, researchers in Sweden conducted a combined analysis of six previously published studies.
The combined analysis suggested that patients with Crohns disease had an increased risk of both colorectal cancer and small intestine cancer.
- The rate of colorectal cancer was almost twice as high in patients with Crohns disease than in the general population .
- The rate of small intestine cancer was roughly 27-times higher in patients with Crohns disease than in the general population.
References:
Jess T, Gamborg M, Matzen P et al. Increased Risk of Intestinal Cancer in Crohns Disease: A Meta-Analysis of Population-Based Cohort Studies. American Journal of Gastroenterology. 2005 100:2724-2729.
American Gastroenterological Association. Patient brochure: Inflammatory Bowel Disease. April 23, 2010.
Singh H, Nugent Z, Demers AA, Bernstein CN. Increased risk of nonmelanoma skin cancers among individuals with inflammatory bowel disease. Gastroenterology. 2011 141:1612-20.
Peyrin-Biroulet L, Khosrotehrani K, Carrat F et al. Increased risk for nonmelanoma skin cancers in patients who receive thiopurines for inflammatory bowel disease. Gastroenterology. 2011 141:1621-28.
Don’t Miss: Can Diverticulitis Cause Ulcerative Colitis
Poor Growth And Development
Ulcerative colitis, and some of the treatments for it, can affect growth and delay puberty.
Children and young people with ulcerative colitis should have their height and body weight measured regularly by healthcare professionals.
This should be checked against average measurements for their age.
These checks should be carried out every 3 to 12 months, depending on the person’s age, the treatment they’re having and the severity of their symptoms.
If there are problems with your child’s growth or development, they may be referred to a paediatrician .
Colorectal Cancer In Ulcerative Colitis And Crohns Disease
According to a Scandinavian population-based cohort study, individuals with ulcerative colitis are at increased risk of developing colorectal cancer compared with those without UC, are diagnosed with less advanced CRC, and are at increased risk of dying from CRC, although these excess risks have declined substantially over time.
Furthermore, patients with Crohn’s disease are at increased risk of diagnosis and death from CRC. Patients with Crohn’s disease who have CRC have a higher mortality than patients without Crohn’s disease who are also diagnosed with CRC. CRC surveillance should likely be focused on patients diagnosed with Crohn’s disease before the age of 40 years, on patients with colon inflammation, and on those who have primary sclerosing cholangitis .
Colorectal cancer in ulcerative colitis
The authors wrote in background of the study published on 11 January 2020 in The Lancet that UC is a risk factor for CRC. However, available studies reflect older treatment and surveillance paradigms, and most have assessed risks for incident CRC without taking surveillance and lead-time bias into account, such as by assessing CRC incidence by tumour stage, or stage-adjusted mortality from CRC.
During follow-up, the researchers observed 1336 incident CRCs in the UC cohort and 9544 incident CRCs in reference individuals .
In the UC cohort, 639 patients died from CRC , compared with 4451 reference individuals during the same time period.
Colorectal cancer in Crohns disease
Also Check: What Are Infusions For Ulcerative Colitis
Does Ibd Increase Your Risk For Colon Cancer
Regardless of the type of colitis, this type of sustained inflammation can cause lasting damage to sensitive tissues, causing pain, bloating, bowel issues and bleeding. If left untreated, IBD can create complications like dysplasia, which results in the growth of abnormal cells in the colon or rectum. Over time, these abnormal cells can mutate into cancer.
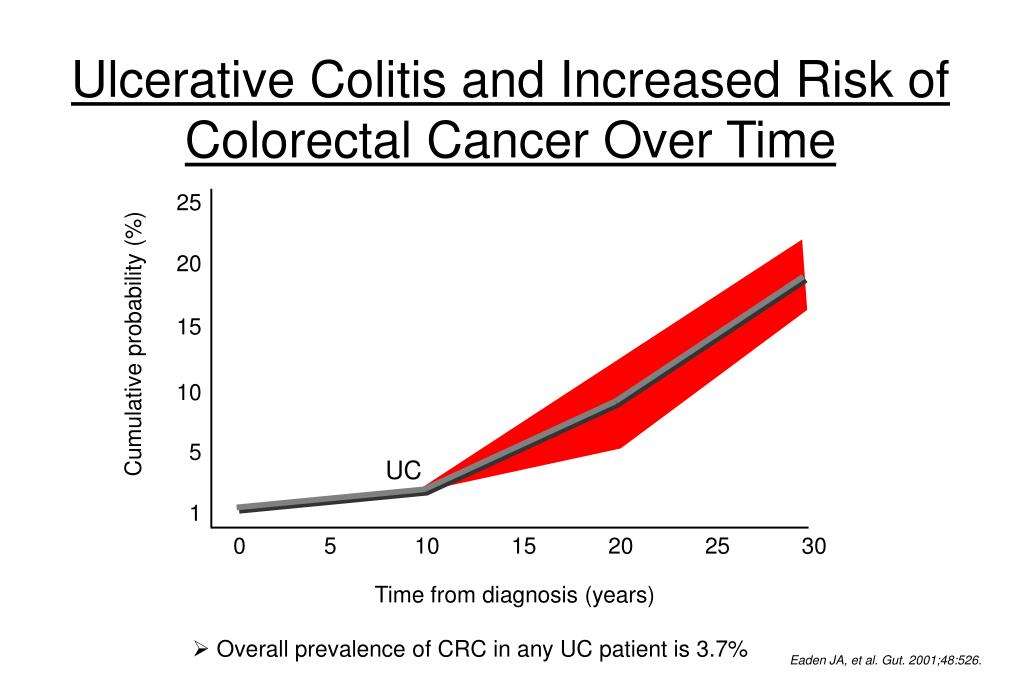
Your risk of developing colon cancer depends on a few factors, such as the type of inflammatory disease you have, how long youve had it and how much of your large intestine is affected, said Dr. Senatore. Research shows that your cancer risk doesnt increase until youve had IBD for at least eight years.
What Is Ulcerative Colitis
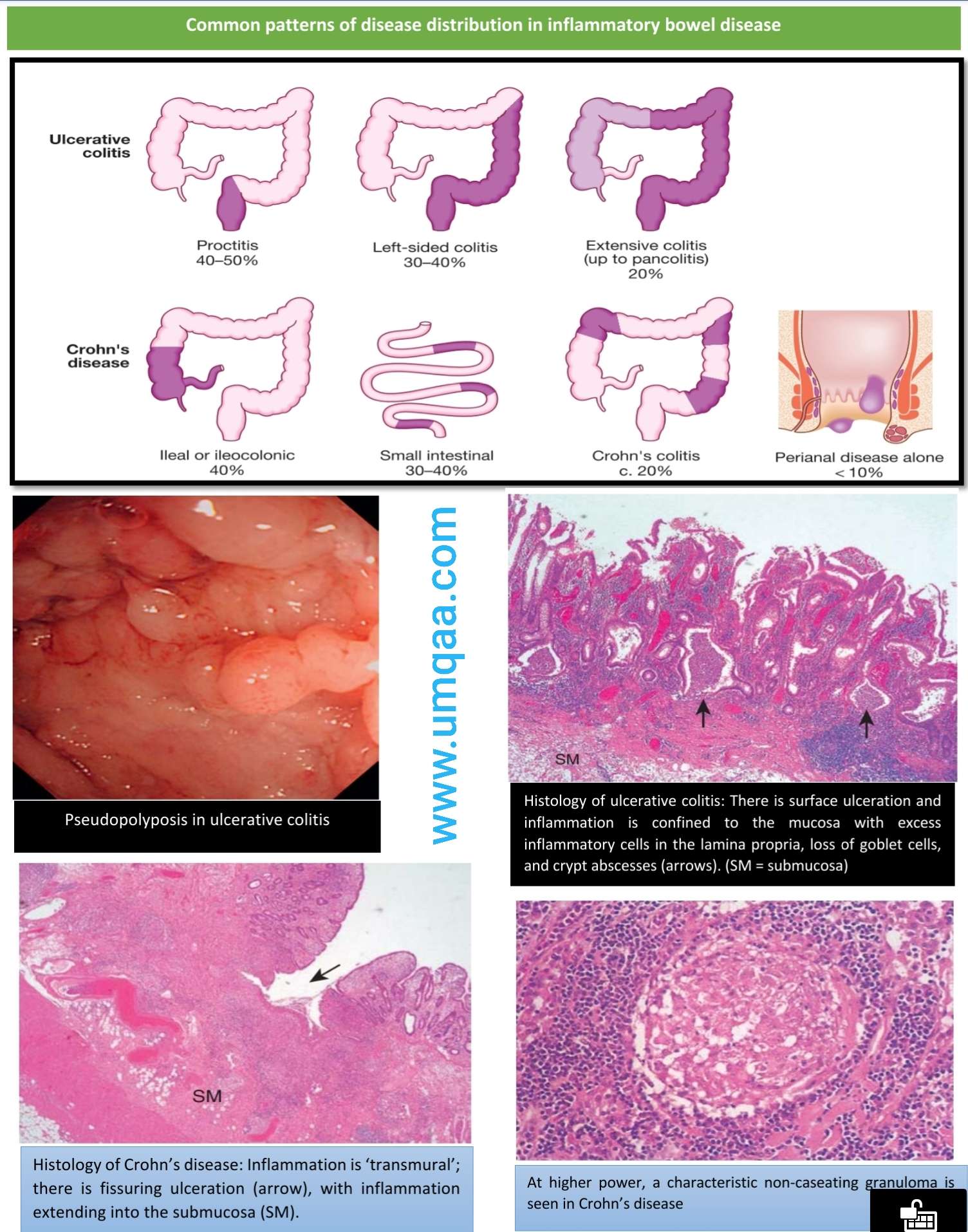
Ulcerative colitis is a form of inflammatory bowel disease that causes inflammation in the lining of the colon. Ulcers and open sores can also form on the colon lining in response to the inflammation. Ulcerative colitis is a lifelong chronic illness that can have recurrences or flare-ups throughout life.
You May Like: What Can I Take For A Stomach Ulcer
What Is Inflammatory Bowel Disease
Inflammatory bowel disease includes conditions such as ulcerative colitis and Crohns colitis, and it occurs when the large intestine becomesand remainsinflamed. Crohns colitis can affect any part of the digestive tract, from the mouth to the anus, whereas ulcerative colitis only impacts the colon or rectum.
Certain Types Of Diets
A diet that’s high in red meats and processed meats raises your colorectal cancer risk.
Cooking meats at very high temperatures creates chemicals that might raise your cancer risk. Its not clear how much this might increase your colorectal cancer risk.
Having a low blood level of vitamin D may also increase your risk.
Following a healthy eating pattern that includes plenty of fruits, vegetables, and whole grains, and that limits or avoids red and processed meats and sugary drinks probably lowers risk.
Also Check: Specific Carbohydrate Diet Ulcerative Colitis
Getting Screened For Cancer
Because your risk for colorectal cancer increases over time if you have UC, its important to receive regular screenings for colorectal cancer.
People with UC should talk to their doctors about getting a colonoscopy, the main test used to detect this cancer.
Getting regular colonoscopies can help lower your risk for developing colorectal cancer or dying from colorectal cancer.
For people with IBDs who underwent regular screenings, the odds of developing colorectal cancer dropped by 42 percent. The odds of dying from the cancer dropped by 64 percent.
How To Reduce Your Risk
Here are a few other things you can do to lower your chances of developing colorectal cancer and improve your odds of finding it early if you develop it:
- Ask your doctor about taking medications such as sulfasalazine , vedolizumab , or mesalamine . These drugs help manage UC, and they may help lower your risk for colorectal cancer.
- Take your medications as your doctor prescribed to keep your UC inflammation well managed.
- See your gastroenterologist for check-ups at least once a year.
- Let your doctor know if any of your family members had colorectal cancer or have recently been diagnosed.
- Eat more fruits, vegetables, and whole grains such as brown rice or wheat bread.
- Limit red meat, such as burgers, steaks, and pork. Also limit processed meats, such as hot dogs, bacon, and sausage. Theyve been linked to colorectal cancer risk.
- Avoid alcohol or limit yourself to no more than one drink a day.
- Try to walk, ride a bike, or do other exercises on most days of the week.
Along with getting regular screenings, look for these symptoms of colorectal cancer and report them to your doctor right away:
- a change in your bowel movements
- blood in your stool
You May Like: Best Dressing For Venous Stasis Ulcer
What Is Irritable Bowel Syndrome
Irritable bowel syndrome is a prevalent disorder that presents a range of varying symptoms, including abdominal pain, bloating, gas, cramping, and diarrhea or constipation, or sometimes both. You may also notice a change in the appearance or frequency of your bowel movements. Though typically not severe, symptoms often persist over an extended period of time.
Q: Does Having Inflammatory Bowel Disease Affect My Risk For Developing Colon Cancer
A: Yes. If you go back 20 years, the thinking was that just ulcerative colitis was associated with increased risk of colon cancer. But weve found more recently that inflammatory bowel disease does have a higher risk than the general population.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.Policy
There are two things we think about here when it comes to risk. The first one is the length of time that someone has had IBD. The second is the degree to which the bowel is affected. So patients that have had it longer and have more of their colon affected are at a higher risk and thats for both patients with Crohns and ulcerative colitis.
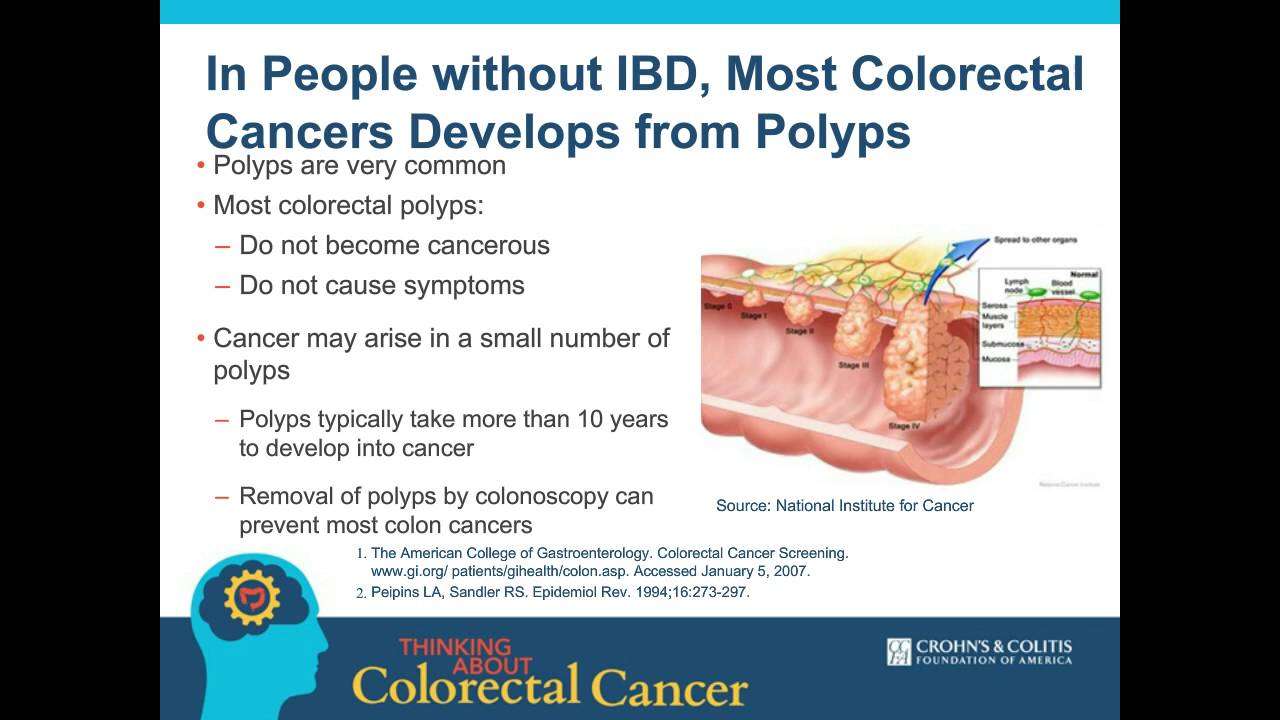
In people without inflammatory bowel disease, the pathway to cancer is pretty clear-cut, where you get a polyp, the polyp becomes dysplastic, and then ultimately you get cancer. But the IBD pathway can be different. So not only is it important that we control these patients inflammation, but also that we follow up with them at more frequent intervals to make sure they dont have cancer.
Don’t Miss: Triderma Diabetic Ulcer Defense Healing Cream
Family History Of Crc
A family history of sporadic CRC is also a risk factor for cancer. IBD patients with a first-degree relative with CRC have twice the risk of developing CRC than IBD patients without a family history of CRC . Moreover, among IBD patients who have a first-degree relative in whom CRC was diagnosed before the age of 50 years, the risk of IBD progression to CRC increases ninefold . However, the presence of a first-degree relative with IBD does not increase the risk of CRC among healthy family members .
Extent And Duration Of Ibd
The extent of colonic inflammation is a risk factor for CRC. UC patients with extensive disease have a greater risk of developing CRC than do UC patients with only proctitis or proctosigmoiditis . IBD duration is one of the most important risk factors for CRC among IBD patients. CRC risk is significantly increased after 8 years of IBD and continues to increase in subsequent years .
You May Like: Does Stomach Ulcer Cause Pain
Not All Screening Methods Work
Some methods used to screen for colorectal cancer in the general population are not appropriate for people with IBD, explains Dr. Rubin. These include CT colonography, also known as *virtual colonoscopy,*which does a poor job of finding flat precancers. Tests that look for blood in the stool as a sign of early cancer also wont work because patients with IBD may have blood in their stool due to inflammation.
Signs And Symptoms To Look Out For
Knowing the signs to look out for can help. However, many signs and symptoms of colorectal cancer also happen to be signs of inflammatory bowel diseases.
For instance, blood in the stool is a sign of colorectal cancer as well as a symptom of UC. It is easy to confuse the potential signs of cancer with those of a normal UC flare-up. For this reason, it is important to regularly check in with a doctor to discuss and monitor the progression of the condition.
Anyone with UC who experiences the following changes or symptoms should speak with a doctor:
You May Like: Venous Stasis Ulcer Right Lower Leg Icd 10
Colorectal Cancer Risk In Ibd
Colorectal cancer risk and IBD
Patients with IBD appear to be at notably increased risk of colorectal cancer compared to the general population , with one recent study demonstrating a 7% colorectal cancer risk after 30 years of disease . Patients with at least 8 years disease duration and colonic involvement are at increased risk of colorectal cancer . Patients at risk of colorectal cancer should be enrolled in a dysplasia surveillance plan as this appears to reduce the risk of colorectal cancer. Surveillance typically includes colonoscopy every 1-3 years, depending on individual patient risk .
Risk factors and surveillance intervals
In patients at high risk, consider ~1 year surveillance intervals. High risk features include: primary sclerosing cholangitis , prior history of dysplasia or colonic strictures, or strong family hx of colorectal cancer . Patients with low to moderate risk may be surveyed every 2-3 years. Moderate risk features include: extensive colitis with moderate inflammatory burden, family hx of CRC in first degree relative > age 50 and possibly extensive inflammatory polyps or pseudopolyps
Surveillance Protocols
Management of Endoscopic lesions
Any visible polyps or lesions should be endoscopically resected if feasible and the specimen should be sent in a separately labeled jar. If a lesion has indistinct borders or is not amenable to resection, biopsy sample should be taken and sent in a separate jar.
Management of Dysplasia
- Clinician Resources
Association Between Colorectal Cancer And Ulcerative Colitis
2/17/2020 3:23:47 PM
Patients with the inflammatory bowel disease ulcerative colitis have a higher risk of dying from colorectal cancer, despite modern therapy, even though the risk has declined in recent years. Olén et al published these findings in The Lancet.
Previous research has shown that patients with ulcerative colitis have an increased risk of colorectal cancer, and therefore, screening recommendations are in place for this patient group. But to what extent have new therapeutic methods helped to reduce risk? This much-debated question has now found new answers. A large study involving 96,000 patients diagnosed with ulcerative colitis between the years 1969 and 2017 has shown that these patients run a higher risk of developing and dying of colorectal cancer.
The risk of colorectal cancer has dropped substantially over the past 30 years, but in spite of this, patients who have had access to modern treatments for ulcerative colitis and screening for colorectal cancer still have a significantly elevated risk, said Ola Olén, MD, senior researcher in the Department of Medicine in Solna at the Karolinska Institutet in Sweden.
Recommended Reading: Artificial Sweeteners And Ulcerative Colitis
Can Ulcerative Colitis Increase Your Risk Of Colon Cancer Find Out
Ulcerative colitis is a condition that causes inflammation in the large intestine, including the colon. Two of the most common effects of this disease are symptoms like abdominal pain and diarrhea. You can also be at an increased risk of colorectal cancer if you have UC.
Duration of Ulcerative Colitis
According to the Crohns & Colitis Foundation, once youve lived with UC for about 8-10 years, your risk for colon cancer typically starts to increase. Your cancer risk is higher if youve had UC for long.
Colorectal cancer rates increase dramatically for people in North America after a person has lived with UC for 30 years, according to a 2019 literature review. In Asia, colorectal cancer rates dramatically increase after a UC duration of about 10-20 years.
Inflammation
Your risk for getting colorectal cancer also depends on how much your colon has inflamed. The highest risk for colorectal cancer has been seen in people with a lot of inflammation in their entire colon.
Primary Sclerosing Cholangitis
If you have this rare complication of UC, you need to be prepared. PSC affects the bile ducts that carry the digestive fluid to the intestine from the liver and causes scarring and inflammation, which narrows the ducts. Youre at higher risk of colorectal cancer, and this disease might start sooner than 8-10 years after youve been diagnosed with UC.
Here are some things you can do to lower your chances of developing colorectal cancer and diagnose it earlier: