Good Bacteria Might Help You Feel Better
UC has been linked to harmful bacteria in the gut. Probiotics are beneficial bacteria that help get rid of bad germs. Adding these supplements to your treatment could help keep you in remission.
No all probiotics are the same, however, and not all of them have evidence to show they can help with UC. People should speak to their doctor before using this option.
Ulcerative Colitis Treatment In Children
Ulcerative colitis tends to be more severe and aggressive in childrenand the inflammation tends to affect more of the colon, according to Yale Medicine1. But the good news is that it can be treated so that kids with UC can live largely normal lives.
Overall, management of ulcerative colitis in children is similar to management in adults, according to Dr. Pasha. For example, kids have similar medication options available to them, such as 5-ASAs, steroids, biologics, and immunomodulators. However, nutrition and growth issues are usually closely monitored. A childs doctor will keep a close eye on any signs of loss of appetite and weight loss, since those can impede a childs growth.
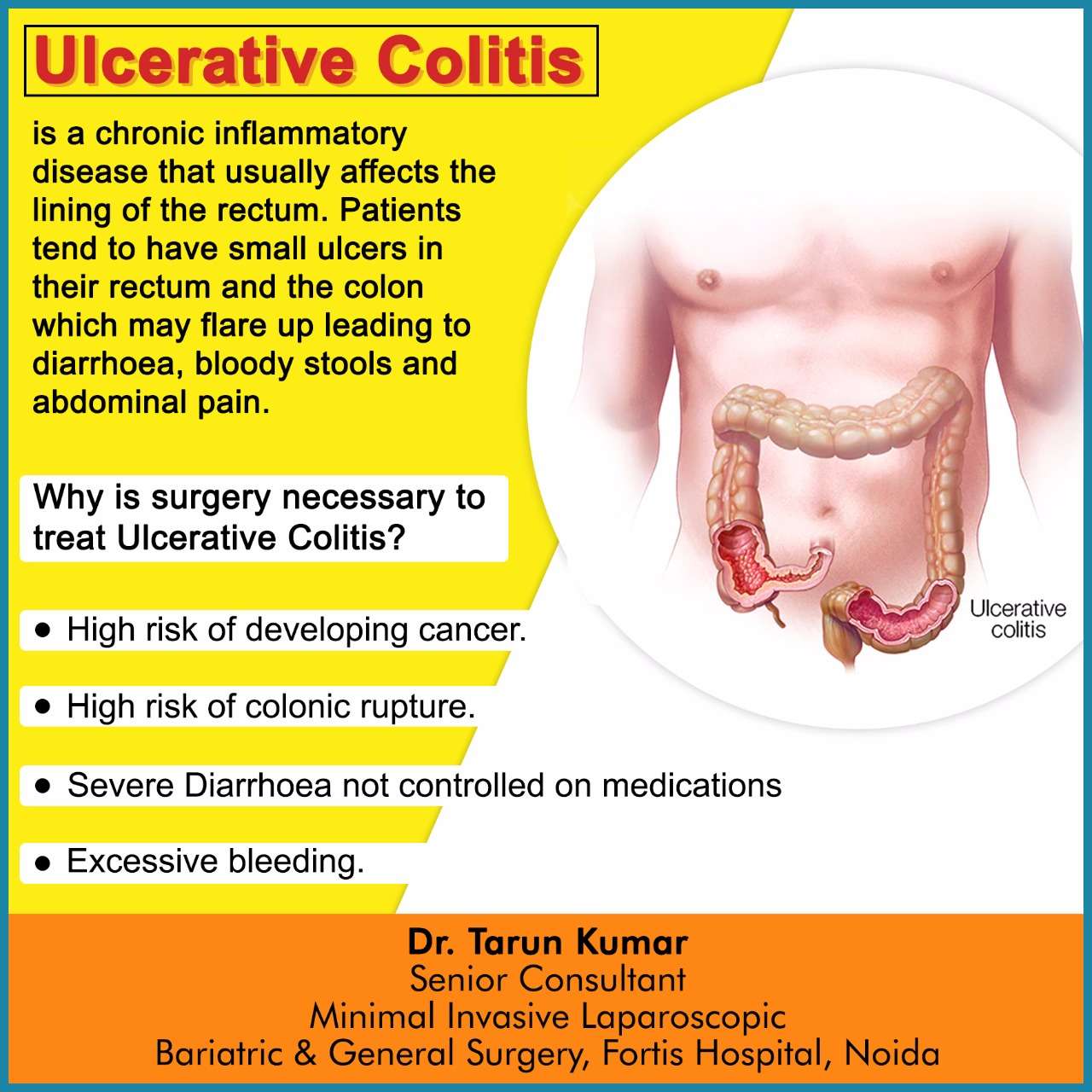
In severe cases, surgery, such as the surgical removal of the colon, may also be an option if the children dont respond well enough to medications, or they experience a ruptured colon or severe bleeding. But ulcerative colitis surgery in kids is much less common these days, thanks to advances in medications like biologics that help control symptoms and let the children enjoy longer periods of remission.
Common Treatments For Ulcerative Colitis
Ulcerative colitis canât be cured, but you can usually manage the symptoms through diet, medication and/or surgery. Your consultant will discuss options with you, based on your symptoms and the extent of your bowel inflammation.
During a very severe flare-up, you may require hospital treatment as an in-patient.
Diet
Making small changes to your daily diet may relieve your symptoms. Try:
- Changing from three daily main meals to five or six small meals every day
- Drinking lots of water
- Avoiding caffeine, alcohol and fizzy drinks
Also, your consultant may recommend taking food supplements to replace nutrients lost as a result of frequent diarrhoea. You may also be referred to a dietitian, wholl help you follow an ulcerative colitis diet plan.
Medication
To prevent symptoms recurring or relieve symptoms during a flare-up, your consultant may prescribe:
- Immunosuppressants
- Aminosalicylates or steroids â to reduce inflammation
- Monoclonal antibodies â drugs which target specific cells
Surgery
If ulcerative colitis is affecting your daily life and other treatments are unsuccessful, your consultant may suggest surgery. In most cases, this involves removing your large bowel so that waste is passed out of your small intestine instead. This requires either:
- An ileostomy an opening in your abdomen for your small intestine to drain into an external pouch
Don’t Miss: Peptic Ulcer Vs Gastric Ulcer
Moderate Or Extensive Disease
Patients with inflammation proximal to the sigmoid colon or left-sided disease unresponsive to topical agents should receive an oral 5-ASA 5-Aminosalicylic Acid Several classes of drugs are helpful for inflammatory bowel disease . Details of their selection and use are discussed under each disorder . Details of their selection and use are discussed under each disorder . Details of their selection and use are discussed under each disorder or corticosteroid therapy as well as those who are corticosteroid-dependent. Moreover, a combination of immunomodulator and anti-TNF therapy Anti-TNF drugs Several classes of drugs are helpful for inflammatory bowel disease . Details of their selection and use are discussed under each disorder (see Crohn disease treatment and ulcerative colitis… read more is sometimes helpful. Finally, in some patients who fail to respond to corticosteroids, immunosuppressants, or biologics, a trial of the Janus kinase inhibitor tofacitinib, or a trial of sphingosine 1-phosphate receptor modulator ozanimod can be considered.
Treating Uc Symptoms At The Source

To get ahead of UC symptoms, first you have to know whats behind them. UC symptoms are linked to excess inflammation that causes damage to your colon lining.
Controlling inflammation over time can help reduce UC symptoms such as frequent and urgent bowel movements, bloody stools, and abdominal pain. Controlling inflammation can also help repair the colon lining.
Controlling inflammation to help repair your colon lining and improve your symptoms is a goal of UC treatment.
UC treatments are designed to control the excess inflammation in your colon. When inflammation is suppressed, it can help relieve common UC symptoms, achieve and maintain remission, and also help heal the tissue in your colon lining.
While many UC treatments are designed to control excess inflammation, some treatments work in different ways than others. You and your doctor should discuss all treatment options and considerations to find the one that may be right for you.
What is remission?
When your UC is in remission, it means you are experiencing no symptoms. If you think about all the ways UC symptoms may be impacting your life, its easy to see why achieving and maintaining remission is so important.
Recommended Reading: Why Did I Get Ulcerative Colitis
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
A Note About Mental Health
Living with a chronic illness like ulcerative colitis can be challenging and frustrating. You may worry about pain, possible complications, and coping with potentially embarrassing accidents. You may struggle to get used to new dietary changes or new bathroom habits.
As a result, having ulcerative colitis can take quite a toll on your mood and your mental health. Your body image and self esteem may suffer, and you may feel like youre the only person whos coping with this kind of stress and anxiety.
But youre not alone. At least 3 million other people in the United States have some sort of inflammatory bowel disease, according to the CDC. It might help you to connect with some others who have firsthand experience with your condition and the stress that it can cause. A support group can be a lifeline when youre feeling all alone and anxious. Find a local support group through the Crohns & Colitis Foundation or ask your doctor for resources. Or you might prefer a virtual support group, like the .
You might also consider talking with a counselor or therapist, especially one who specializes in working with people with chronic illnesses.
Remember, you can live a happy, rich life with ulcerative colitis, and it doesnt affect your life expectancyall good things.
You May Like: Is Beer Bad For Ulcerative Colitis
Technical Aspects Of Surgical Approaches For Refractory Moderate
IPAA may be constructed using either a stapled or a handsewn technique, with comparable functional outcomes. Thus, the type of anastomosis should be left to the surgeons discretion
Overall, stapled and handsewn IPAAs seem to result in comparable complication rates, functional outcomes, and QoL. In a meta-analysis of four randomised controlled trials including 184 patients , no significant differences were observed in terms of functional outcomes, sphincter resting pressure, or squeeze pressures. Based on low-quality evidence, the stapled technique may be more likely to achieve perfect continence compared with the handsewn approach. Despite slightly better functional outcomes after stapled anastomosis, overall QoL appears equivalent between the two groups.,
Due to a paucity of high-quality data, no recommendations can be made with regards to sexual function, strictures, and septic complications between stapled and handsewn techniques, although stapled IPAA is likely associated with a higher rate of cuffitis.,
Laparoscopic surgery is the preferred approach to patients with medically refractory UC, as it is associated with lower intra- and postoperative morbidity, faster recovery, fewer adhesions and incisional hernias, shorter hospital length of stay, improved female fecundity, and better cosmesis
Get Regular Exercise To Reduce Uc Inflammation
Snider says exercise is useful in managing many of the complications associated with ulcerative colitis, including decreased bone density, a weakened immune system, emotional health problems, stress, and weight gain.
“Try to engage in a moderate-intensity exercise like swimming or biking, three or four days per week,” he says. A review published in August 2016 in Pharmacological Reports noted that moderate exercise releases protective myokines such as irisin from working skeletal muscles, which promotes healing and helps with inflammatory bowel disease inflammation.
Snider also strongly recommends yoga as a natural treatment for ulcerative colitis, as it promotes relaxation and targets the digestive system, flooding the area with oxygen and nutrition for healing. Find what type and frequency of exercise works for you and take it slow: Too much exercise can cause mild systemic inflammation.
Research indicates that stress plays a role in inflammatory bowel diseases such as ulcerative colitis. Researchers analyzed data on 2,007 adults in a Swiss IBD study and found a relationship between depression and anxiety and disease symptoms. The results were published in June 2016 in Clinical Gastroenterology and Hepatology.
Counteract stress with relaxation techniques such as meditation, deep breathing, and progressive muscle relaxation to help your body relax.
Also Check: What Is The Best Thing To Put On Leg Ulcers
Consider Therapy To Help Manage Stress And Pain
Working with a therapist on certain mind-body techniques can help you control ulcerative colitis symptoms.
Cognitive behavioral therapy and a technique called biofeedback may be useful, as these processes teach skills to cope with stress and pain. In CBT, you learn to recognize and change behaviors and emotions that affect you physically. According to an article in Therapeutic Advances in Gastroenterology, CBT can ease abdominal pain for some people. Biofeedback will teach you how to identify and control some bodily processes, such as heart rate or tension in your muscles, and it can be effective in helping manage chronic pain.
How To Treat An Ulcerative Colitis Flare
The great thing about the internet is that you have constant access to information on any topic you want to learn about. The bad thing about the internet is that it can be difficult to determine a credible source from a phony one. When it comes to finding information on how to best manage GI conditions like Ulcerative Colitis , online information can often be contradicting and confusing. Thankfully, were up to date on the current research and recommendations to help you best manage your Ulcerative Colitis symptoms.
The tough part about ulcerative colitis management is that our recommendations are specifically tailored to your stage of ulcerative colitis- active or dormant .
Also Check: List Of Foods Good For Ulcers
Care For Your Child Before And After Surgery
Before either surgery, your childs surgical team will explain the details, including:
- What will happen before, during and after your childs operation
- How long its likely to take
- How long your child may need to stay in the hospital afterward
- What kind of care your child will need at home after surgery
Some children who have pouch surgery have complications afterward. The IBD Center team provides care and support for these conditions, which include urgent need to use the bathroom, bleeding, inflammation of the pouch and problems emptying stool from the pouch. Treatment options offered through the IBD Center include dietary therapies, antibiotics, probiotics, medicines that reduce inflammation, treatments done with an endoscope and surgery.
Toxic Megacolon And Other Complications Of Severe Uc
Toxic megacolon may be defined as colonic dilatation of more than 5.5 cm along with signs of systemic toxicity. Lifetime incidence of toxic megacolon in patients with UC varies from 1%-2.5% and approximately 5% severe UC patients who are hospitalized may develop toxic megacolon. Risk factors include dyselectrolytemia, full bowel preparation and medications . Earlier identification of this condition, prompt institution of medical therapy and low threshold of surgery in cases of non-response to medical therapy within 48 h will decrease the morbidity and mortality of this condition.
Other complications include perforation which is the most serious complication of severe UC. Risk factors include inappropriate total colonoscopy and delaying treatment of toxic megacolon. Diagnosis of perforation can often be delayed as abdominal signs can be masked when patient is on steroids. Therefore, patients with severe UC should be monitored closely for abdominal signs and on the slightest suspicion abdominal radiographs should be obtained. Other complication includes severe hemorrhage.
Recommended Reading: Mesalamine Medication For Ulcerative Colitis
When To Contact A Medical Professional
Contact your provider if:
- You develop ongoing abdominal pain, new or increased bleeding, fever that does not go away, or other symptoms of ulcerative colitis
- You have ulcerative colitis and your symptoms worsen or do not improve with treatment
- You develop new symptoms
There is no known prevention for this condition.
Rice Water To Fight Ulcerative Colitis
One cup of rice water as soon as you wake up and another before bed will help control ulcerative colitis and its symptoms.
Ingredients
Preparing this drink is very simple.
Dont Miss: Difference Between Ulcerative Colitis And Crohns Disease Ppt
Recommended Reading: What Causes Ulcerative Colitis Flare Ups
Complementary And Alternative Remedies
Alternative treatments such as acupuncture may help reduce and regulate bowel inflammation, reducing UC pain.
Another form of alternative treatment called moxibustion may also have a positive effect on UC symptoms. Moxibustion is a type of heat therapy. It uses dried plant materials burned in a tube to warm the skin, often in the same areas targeted by acupuncture.
Squeeze More Exercise Into Your Daily Routine
Exercise has many benefits for your physical and mental health. And it can help you manage the anxiety and stress associated with ulcerative colitis.
Gentle exercises like walking and yoga are exceptionally helpful. Research has shown that exercise in conjunction with other interventions like medication helped to reduce symptoms, improve immunological response, and improve nutrition levels.
Other low-intensity options include swimming, biking, and gentle stretching.
Also Check: Stomach Ulcer And Weight Loss
You May Like: Ulcerative Colitis And Lactose Intolerance
How Is Colitis Diagnosed
Your healthcare provider will begin by asking you about your symptoms, when they began and what you were eating and drinking at the time. Theyll ask you about your current medications and any health conditions that youve been recently treated for. Theyll physically examine you, then move on to medical tests. These are likely to include blood tests, stool tests and imaging tests to look at your colon.
Blood tests involve drawing a small amount of your blood through a needle and sending it to a lab to analyze. Stool tests involve taking a sample of your poop and sending it to the lab. Proteins in your blood and stool can show evidence of inflammation and sometimes indicate a particular type of infection. Imaging tests can confirm inflammation and give more detailed information about your condition.
In particular, endoscopic tests that visualize the inside of your colon with a lighted scope can be helpful in diagnosing the type of colitis you have. Endoscopic exams, including colonoscopy and flexible sigmoidoscopy, allow healthcare providers to take tissue samples from the inside of your colon . Healthcare providers can learn important information by examining tissue samples in the lab.
Active Uc Of Any Extent Not Responding To Aminosalicylates
In mild-to-moderate UC of any extent, aminosalicylates such as mesalamine are the preferred initial treatment . In patients with disease activity limited to the rectum, topical therapy alone might suffice, but combination therapy is more effective and is also recommended for left-sided and extensive UC . Table 2 gives an overview on current treatment options.
Table 2.
Medical therapy for UC
Fig. 1.
Active ulcerative colitis of any extent not responding to 5-aminosalicylates . MMX, multimatrix AZA, azathioprine 6-MP, 6-mercaptopurine.
Except in case of isolated proctitis, where topical corticosteroids alone may be considered, treatment with oral corticosteroids should be initiated in patients who do not respond adequately to 5-ASA . In case of isolated proctitis, topical corticosteroids alone might be considered. The introduction of corticosteroids should be a shared decision-making process that includes patients preference of therapy and tolerance to 5-ASA. It is, however, recommended to start corticosteroids in patients with sustained rectal bleeding for 2 weeks, persistent abdominal symptoms after 6 weeks of adequate therapy with 5-ASA or if symptoms deteriorate . In selected cases, a prolonged therapy with up to 16 weeks might still be able to achieve remission.
You May Like: What Is An Ulcer Diet
You May Like: High Dose Remicade For Ulcerative Colitis
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.