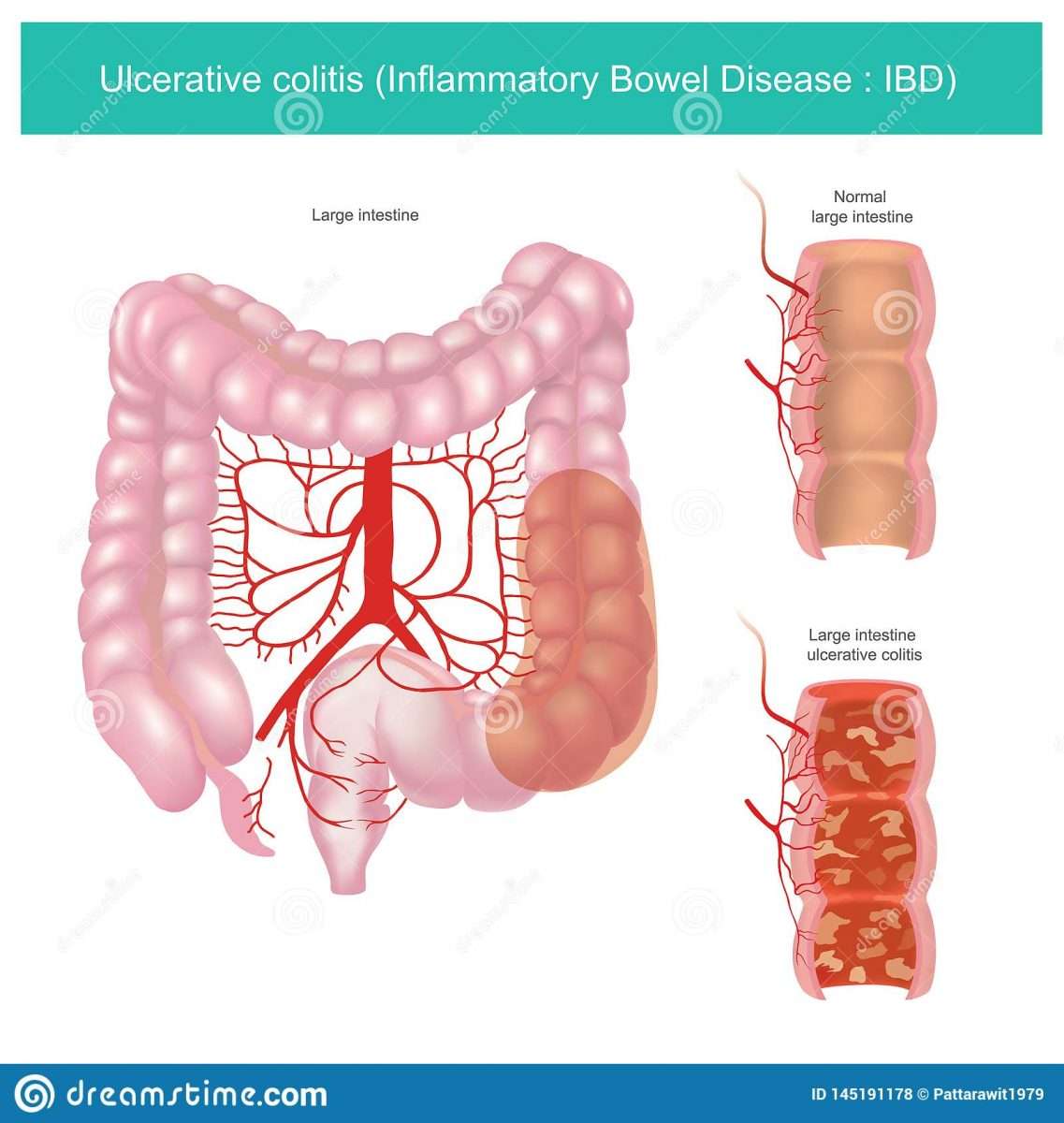
What Is Ulcerative Colitis
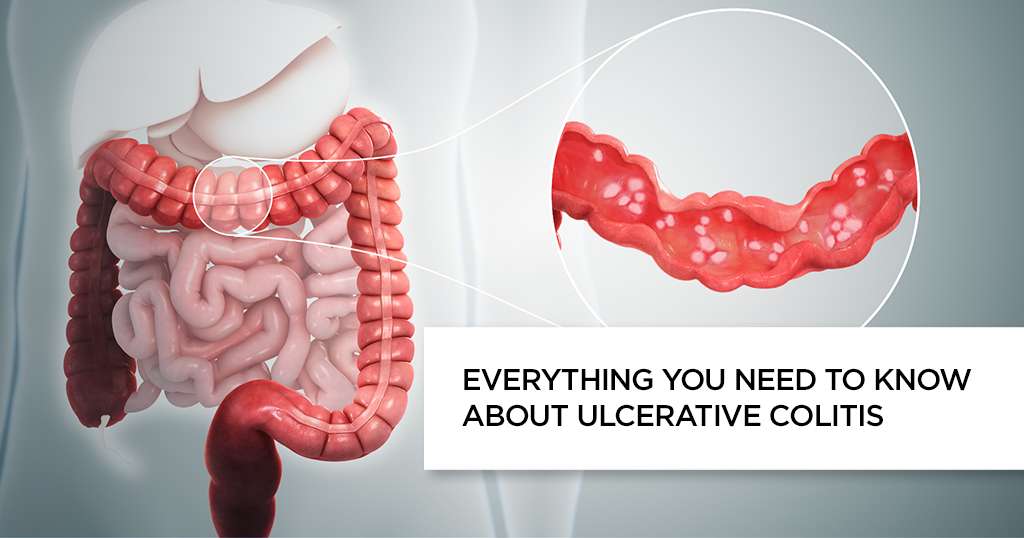
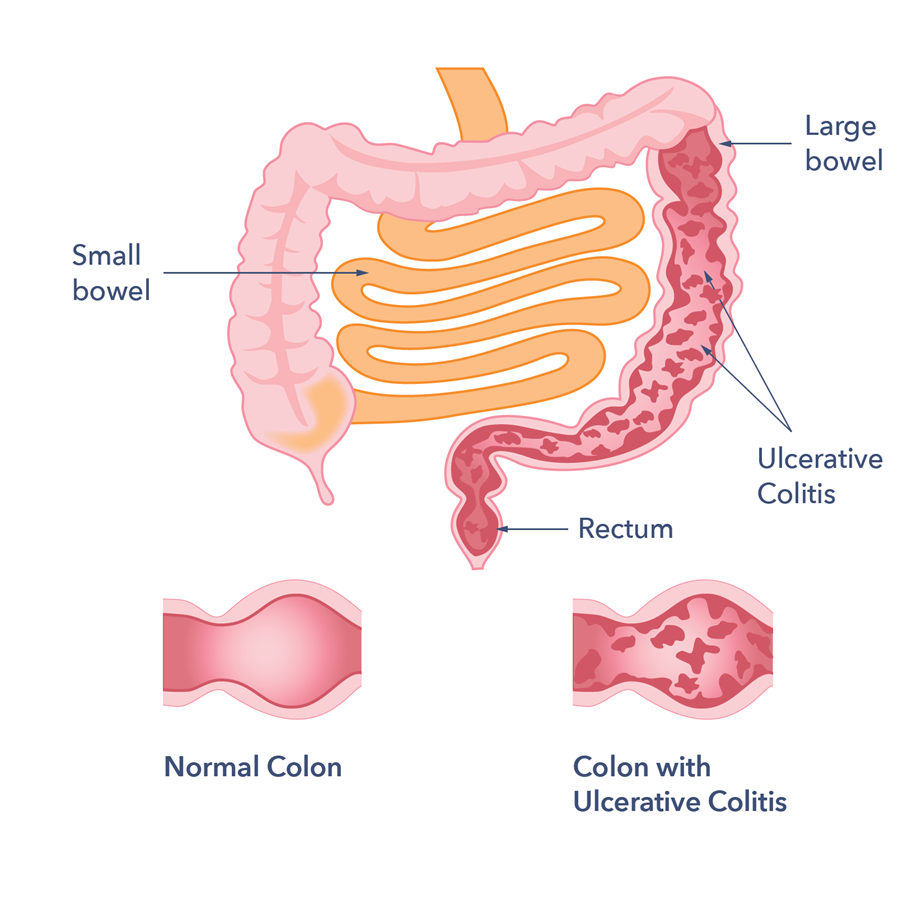
Ulcerative colitis is a chronic disease of the colon or large intestine. It is marked by inflammation and ulceration in the colons innermost lining. Tiny, open sores form on the surface of this lining they bleed and produce pus and mucus. Because the inflammation makes the colon empty frequently, symptoms include diarrhea and, often, abdominal cramping.
The inflammation usually begins in the rectum and lower colon, but it may involve the entire colon. When it affects only the lowest part of the colon the rectum it is called ulcerative proctitis. If it affects only the left side of the colon, it is known as limited or distal colitis. Ulcerative colitis involving the entire colon is called pancolitis.
Daily Life For People With Ibd
People with IBD lead useful and productive lives, even though they need to take medications. When they are not experiencing a flare-up of their disease, they feel quite well and are often free of symptoms.People with IBD can marry, enjoy sexual activity and have children. They can hold down jobs, care for families and enjoy sport and recreational activities.Even though there is currently no cure for IBD, medical therapy has improved the health and quality of life of most people with Crohns disease and ulcerative colitis. Research underway today may lead to further improvements in medical and surgical treatment, and even a cure.
Complementary And Alternative Treatments For Ulcerative Colitis
Some complementary treatments may help some people in their efforts to deal with ulcerative colitis. These treatments, sometimes referred to as alternative therapies, are used in conjunction with traditional medical treatments. Complementary treatments are not meant to substitute for traditional medical care. Be sure to notify your doctor if you are consuming nutritional supplements or homeopathic remedies as they may interact with the prescribed medical therapy.
Complementary treatments may include:
- Massage therapy
- Nutritional dietary supplements, herbal remedies, tea beverages, and similar products
- Probiotics, which in one study had a positive effect on symptoms and quality of life as reported by patients with UC
- Yoga
Read Also: What Desserts Can I Eat With Ulcerative Colitis
Skin Disorders Associated With Ulcerative Colitis
Below are six skin conditions that people with ulcerative colitis can be at increased risk of developing.
1. Erythema Nodosum The most common skin condition associated with ulcerative colitis, erythema nodosum is a rash that consists of painful, raised bumps and is usually found on the legs.
It tends to develop when ulcerative colitis is active, notes Dr. Hagan. You may also run a fever, have joint pain, and generally feel ill, according to Medline Plus.
Treatment options include pain-relieving medication, steroids , and a potassium iodide solution to clear up the bumps.
A cool compress can also help alleviate discomfort and reduce inflammation, says Kally Papantoniou, MD, a dermatologist in private practice in Melville, New York. She also recommends elevating your legs to help lessen swelling and tenderness.
Compression stockings can also be helpful, but have your doctor evaluate you for vascular disease before using them, cautions Dr. Papantoniou.
Symptoms of erythema nodosum usually go away within three to six weeks, but the residual bruises may last for months. In about 20 percent of cases, the rash comes back.
2. Pyoderma Gangrenosum This is a severe and debilitating condition that starts as a rash made of red or purple bumps or blisters, and then quickly spreads. These blisters eventually join together and form deep open sores , according to the Crohn’s& Colitis Foundation.
Pyostomatitis vegetans is the same condition, but it occurs in the mouth, Brieva says.
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Don’t Miss: Signs Of Ulcerative Colitis Flare Up
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Vitamin And Mineral Supplements For Ibd
A person with IBD who eats a healthy, varied diet does not usually need to take vitamin supplements. But if they have a dietary deficiency, they may need tablets or occasional vitamin B12 injections. For example, a person on a low-fibre diet may need extra vitamin C and folic acid because they dont eat enough fruit and vegetables.A person with Crohns disease who experiences steatorrhoea may need calcium and magnesium supplements. Most children with IBD should take supplements to help them grow and develop normally.
Also Check: Difference Between Ulcerative Colitis And Crohn’s Disease Ppt
How Does Ulcerative Colitis Affect Quality Of Life
Ulcerative colitis is a chronic, complex disease that requires much mental, emotional and physical energy to manage. Determinants of quality life include disease symptoms, social and emotional health, sexual functioning, and overall health. People with UC have a lower quality of life compared to a general population . The more severe the disease, the greater the impact on quality of life.
There is evidence from quality of life studies that people who perceive their UC as more severe and disabling also report greater symptoms of anxiety and depression. This is important as a patients outlook is a significant factor in overall functioning and quality of life, especially with chronic diseases.
The greatest impact on quality of life for UC patients is fecal incontinence and other gastrointestinal symptoms. Other factors include:
- Unemployment
- Withdrawal from social engagements or group activities
In a Danish study looking at UC quality of life, the most important medical-related attribute to patients was improvement of symptoms within eight weeks. Not surprisingly, there is a preference for oral medications over injections or infusions. Many UC patients who took part in the study noted a preference for not taking steroids, even during a UC flare.
Whats The Difference Between Ulcerative Colitis And Crohns Disease
UC and Crohns disease are the most common forms of IBD. Both conditions are thought to be the result of an overactive immune system.
They also share many symptoms, including:
- cramps
- diarrhea
- fatigue
However, UC and Crohns disease do have distinct differences. Understanding the key differences between them can help you obtain a proper diagnosis.
Location
These two conditions affect different portions of the GI tract.
Crohns disease may affect any part of the GI tract, from the mouth to the anus. Its most often found in the small intestine. UC only affects the large intestine and rectum.
Response to treatment
Similar medications are prescribed to treat both conditions. Surgery is also a treatment option. Its a last resort for both conditions, but it can be a cure for UC, whereas its only a temporary therapy for Crohns.
Read Also: What To Eat With Gastric Ulcer
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use:For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Ulcerative Colitis Can Take A Toll On Your Mental Health Too
Being told you have a chronic illness can feel like someone has just rerouted the course of your whole life. I went through my own acceptance process, Skomski says. I definitely went through a period of questioning if my life would ever be normal. With time, processing the reality of having ulcerative colitis became easier. I had to learn there’s nothing wrong with me it’s just part of who I am, Skomski says. You have to do a lot of mental work to flip the way you perceive it because otherwise it can really eat away at you.
Dealing with the symptoms can also be mentally and emotionally taxing. The psychological side of the pain is a lot worse than the actual physical sensation, Sam says. It’s when you feel like it’s never going to end, or you’re going to be stuck in that high level of pain for a long period of time, or that no one gets how hard it is to deal with it. This has led to constant vigilance about her health. It’s very hard for me to not be closely monitoring my body 24/7, Sam says. The catch-22 is that stress is definitely a trigger for me.
Also Check: What Can You Eat When You Have An Ulcer
Crohns Disease And Ulcerative Colitis And Digesting Food
Your mouth and stomach break down food by mechanical and chemical means. When the food has reached a pulp-like consistency, it is slowly released into the first part of the small intestine . The food is then massaged along the length of the small intestine. Organs like the pancreas and the gall bladder make digestive enzymes to further break down the food into its simpler components.
The small intestine is lined with microscopic , finger-like projections that lie close to tiny blood vessels . Nutrients pass into the bloodstream through these villi. The rest of the food is pushed into the large bowel, which absorbs excess water. The waste is then temporarily stored in the colon before it is eliminated from the anus.The two ways in which Crohns disease and ulcerative colitis disturb the digestion and absorption processes are:
- Crohns disease an inflamed ileum impairs absorption of vitamin B12 and bile salts. Inflammation along the length of the small intestine impairs absorption of all food nutrients. Inflammation of the large bowel impairs water absorption, causing diarrhoea.
- Ulcerative colitis digestion and absorption are generally not affected. Inflammation of the large bowel impairs water absorption, causing diarrhoea.
Other factors that may affect your nutritional status include:
Goals Of Ulcerative Colitis Treatment
At the IBD Center, our goals for treating your childs ulcerative colitis are to:
- Restore balance and health to your childs body
- Relieve any pain or other symptoms caused by ulcerative colitis
- Make sure your child is getting good nutrition
- Restore your childs growth and development
- Ensure your child builds the best bone density
- Help your child and family with the mental, emotional and social effects of IBD
Read Also: Chicken Recipes For Ulcerative Colitis
People Describe How They Were Diagnosed With Ulcerative Colitis
Ulcerative colitis, or UC for short, is a form of inflammatory bowel disease that affects portions or all of your large intestine and rectum. The Centers for Disease Control and Prevention estimates that 3.1 million Americans have IBD, which also includes Crohns disease .
UC is a chronic condition that can cause long-term inflammation and ulceration, severe diarrhea, abdominal pain, blood and mucous in your stool, urgency, nausea, joint paint, fever, weight loss, and fatigue. UC is also a risk factor in colorectal cancer, according to the Mayo Clinic. And while theres no known cure for ulcerative colitis, removal of the colon and rectum in a procedure called a proctocolectomy can eliminate the disease.
Other treatment options include corticosteroids, anti-inflammatory drugs called 5-aminosalicylates, immunosuppressant biologics , and bowel resection or removal. Patients can also manage symptoms with pain medication, anti-nausea medication, and antidiarrheals, though all medications should be taken under the care of a doctor. IBD is often confused with irritable bowel syndrome , a disorder that causes pain and cramping of the large intestine. But unlike IBD, IBS doesnt cause long-term damage to your intestinal tissue or increase your risk of colorectal cancer.
Managing UC is a complex puzzle of treatment options and unpredictable symptoms. We spoke with nine women to find out what life is like with the disease.
Responses have been edited for length and clarity.
Related:
Should I Keep My Ibd Appointments At This Time
Yes, you should keep your appointments, but do so virtually, if possible. Most of our IBD patients are having their appointments by telephone, MyChart, or video visits. We can handle many of your concerns and questions as well as your routine healthy follow up visits this way. If your IBD symptoms worsen and you are feeling sick, it is safe to come to an appointment at the clinic. We will work with you to find the best way to make an appointment happen. We have deferred most elective colonoscopies or other endoscopic procedures at this time. If you need a procedure because of something thats time sensitive or essential in other ways for your management, we certainly are able to do that. The best thing to do is to call your doctor to find out what options are available for you.
Also Check: How To Heal Ulcerative Colitis Flare
You May Like: Ulcerative Colitis And Stomach Pain
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
How Does Ulcerative Proctitis Affect The Body
Ulcerative proctitis causes inflammation in the tissues that line the rectum, which is the last six to eight inches of the large intestine leading to the anus. This swelling can be painful. Open, bleeding sores called ulcers often form in the rectum as well. It can lead to ulcerative colitis, a more extensive condition, or it may be caused by ulcerative colitis. Ulcerative proctitis can cause pain, bloody diarrhea, constipation, and rectal discharge of mucus or pus.
Recommended Reading: How To Treat Mouth Ulcers
Your Priorities May Change
Facing chronic health challenges tends to make you realize what you value most. I know where I want to put my energy and what’s worth it and what’s not, Skomski says.
Getting diagnosed shifted Sams approach to her health in a similar way. I tend to be a very intense person and kind of a workaholic, she says. Being diagnosed with ulcerative colitis completely changed my priorities for life. I was always a health-conscious person, but now health is absolutely my number one priority. I am no longer willing to sacrifice my health for something else, like a job or even a passion.
It also affected her long-term goals. I originally wanted to become a professor and work in academia, she says. Now she works for an online pharmacy. As I went through this and I saw how amazing the health care system in this country is in some ways and how awful it is in so many ways, it really inspired me to go into health care and work with other people going through my struggle, she says. That was never on my radar before, and now that’s what I want to go into for the rest of my life.
Related:
Ibd And Changing Your Diet
Some dietary changes that may help a person with IBD include:
- Low-fibre diet when IBD is active, most people find a bland , low-fibre diet helps to ease diarrhoea and abdominal cramping. People with Crohns disease who have a narrowed small intestine may need to eat a low-fibre diet most of the time.
- Low-fat diet people with Crohns disease who experience steatorrhoea may benefit from a low-fat diet.
- Low-lactose diet the milk sugar lactose is broken down by the enzyme lactase, commonly found in the lining of the small intestine. Some people with Crohns disease lack this enzyme, so should avoid milk and other dairy products. Lactose intolerance can be diagnosed with a simple test ask your doctor.
- Liquid diet a person with severe Crohns disease may need a nutritionally balanced liquid diet.
- Plenty of water people with IBD need to drink plenty of fluids to prevent dehydration.
Also Check: Best Diet For Gerd And Ulcers
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
What Should You Eat When You Have Ulcerative Colitis
When it comes to food, theres no known dietary cause of ulcerative colitis, but different foods may aggravate or help limit symptoms of the disease.
Youre more likely to need to change your diet during periods of active disease , when eating soft, bland foods can help limit symptoms like cramping and diarrhea. With guidance from a doctor, a liquid meal replacement diet known as an elemental diet, can also help achieve remission from active disease.
During flares, you may also want to avoid or limit high-fiber and high-fat foods, as well as alcohol, dairy products, and spicy foods.
If youre losing nutrients and water in your diet due to diarrhea, you may need to focus on increasing your fluid intake and getting enough calories, protein, vitamins, and minerals from foods or supplements.
Editor’s Picks
Don’t Miss: How To Control Ulcerative Colitis